Hernia
| Hernia | |
|---|---|
| Diagnostic method | Based on symptoms, medical imaging[1] |
| Treatment | Observation, surgery[1] |
| Frequency | 18.5 million (2015)[4] |
| Deaths | 59,800 (2015)[5] |
A hernia (pl.: hernias or herniae, from
Various types of hernias can occur,[6] most commonly involving the abdomen, and specifically the groin.[6] Groin hernias are most commonly inguinal hernias but may also be femoral hernias.[1] Other types of hernias include hiatus, incisional, and umbilical hernias.[6] Symptoms are present in about 66% of people with groin hernias.[1] This may include pain or discomfort in the lower abdomen, especially with coughing, exercise, or urinating or defecating.[1] Often, it gets worse throughout the day and improves when lying down.[1] A bulge may appear at the site of hernia, that becomes larger when bending down.[1]
Groin hernias occur more often on the right than left side.
Risk factors for the development of a hernia include
Groin hernias that do not cause symptoms in males do not need to be repaired.
Globally in 2019, there were 32.53 million prevalent cases of inguinal, femoral, and abdominal hernias, with a 95% uncertainty interval ranging from 27.71 to 37.79 million. Additionally, there were 13.02 million incident cases, with an uncertainty interval of 10.68 to 15.49 million. These figures reflect a 36.00% increase in prevalent cases and a 63.67% increase in incident cases compared to the numbers reported in 1990. [11]About 27% of males and 3% of females develop a groin hernia at some point in their lives.[1] Inguinal, femoral and abdominal hernias were present in 18.5 million people and resulted in 59,800 deaths in 2015.[4][5] Groin hernias occur most often before the age of 1 and after the age of 50.[2] It is not known how commonly hiatus hernias occur, with estimates in North America varying from 10% to 80%.[3] The first known description of a hernia dates back to at least 1550 BC, in the Ebers Papyrus from Egypt.[12]
Pathogenesis
Most hernias happen when the muscles and tendons in the belly weaken or get damaged, which makes it hard for them to keep your insides in place and support your body properly. Our belly and pelvis act like a container made of muscles, tendons, and bones. When pressure builds up inside this container, the muscles push back to keep everything in place. But if the pressure gets too high, it can cause the belly's wall to break, leading to a hernia. Once a hernia starts, it keeps getting bigger because the tension on the wall there increases.[13]
Epidemiology
About 27% of males and 3% of females develop a groin hernia at some time in their lives.[1] In 2013 about 25 million people had a hernia.[14] Inguinal, femoral and abdominal hernias resulted in 32,500 deaths globally in 2013 and 50,500 in 1990.[15] Healthcare costs associated with abdominal wall hernias account for an annual expenditure of approximately 2.5 to 3 billion dollars.[16]
Signs and symptoms


Symptoms and signs vary depending on the type of hernia. By far the most common hernias develop in the
Hernias might manifest with pain in the area, a noticeable lump, or less specific symptoms caused by pressure on an organ stuck within the hernia, potentially leading to organ dysfunction. Typically, fatty tissue is the initial entrant into a hernia, but it might also involve an organ. Hernias are caused by a disruption or opening in the fascia, or fibrous tissue, which forms the abdominal wall. It is possible for the bulge associated with a hernia to come and go, but the defect in the tissue will persist.
Symptoms may or may not be present in some
Irreducible abdominal hernias or incarcerated hernias may be painful, but their most relevant symptom is that they cannot return to the abdominal cavity when pushed in. They may be chronic, although painless, and can lead to strangulation (loss of blood supply), obstruction (kinking of intestine), or both. Strangulated hernias are always painful and pain is followed by tenderness.
In the diagnosis of abdominal hernias, imaging is the principal means of detecting internal diaphragmatic and other nonpalpable or unsuspected hernias. Multidetector CT (MDCT) can show with precision the anatomic site of the hernia sac, the contents of the sac, and any complications. MDCT also offers clear detail of the abdominal wall allowing wall hernias to be identified accurately.[19]

Complications
Untreated hernia may be complicated by:
- Inflammation
- Obstruction of any lumen, such as bowel obstruction in intestinal hernias
- Strangulation
- Hydrocele of the hernial sac
- Hemorrhage
- Autoimmuneproblems
- Irreducibility or incarceration, in which it cannot be reduced, or pushed back into place,[20] at least not without very much external effort.[21] In intestinal hernias, this also substantially increases the risk of bowel obstruction and strangulation.
Causes
Causes of hiatus hernia vary depending on each individual. Among the multiple causes, however, are the mechanical causes which include: improper heavy weight lifting, hard

Furthermore, conditions that increase the pressure of the abdominal cavity may also cause hernias or worsen the existing ones. Some examples would be: obesity, straining during a bowel movement or urination (constipation,
Also, if muscles are weakened due to
The physiological school of thought contends that in the case of
Abdominal wall hernia may occur due to trauma. If this type of hernia is due to blunt trauma it is an emergency condition and could be associated with various solid organs and hollow viscus injuries.
Diagnosis
Inguinal



By far the most common hernias (up to 75% of all abdominal hernias) are inguinal hernias, which are further divided into the more common
There are special cases where a direct and indirect hernia appear together. A
Additionally, though very rare, two or more indirect hernias may appear together such as in a
Femoral
Femoral hernias occur just below the inguinal ligament, when abdominal contents pass into the weak area at the posterior wall of the femoral canal. They can be hard to distinguish from the inguinal type (especially when ascending cephalad)[clarification needed]: however, they generally appear more rounded, and, in contrast to inguinal hernias, there is a strong female preponderance in femoral hernias. The incidence of strangulation in femoral hernias is high. Repair techniques are similar for femoral and inguinal hernia.
A Cooper's hernia is a femoral hernia with two sacs, the first being in the femoral canal, and the second passing through a defect in the superficial fascia and appearing almost immediately beneath the skin.
Umbilical
They involve protrusion of intra-abdominal contents through a weakness at the site of passage of the umbilical cord through the abdominal wall. Umbilical hernias in adults are largely acquired, and are more frequent in
Incisional
An incisional hernia occurs when the defect is the result of an incompletely healed surgical wound. When these occur in median
Diaphragmatic
Higher in the abdomen, an (internal) "diaphragmatic hernia" results when part of the stomach or intestine protrudes into the chest cavity through a defect in the diaphragm.
A
A
Other hernias
Since many organs or parts of organs can herniate through many orifices, it is very difficult to give an exhaustive list of hernias, with all synonyms and
- Abdominal wall hernias:
- Umbilical hernia
- Epigastric hernia: a hernia through the linea alba above the umbilicus.
- Spigelian hernia, also known as spontaneous lateral ventral hernia
- Amyand's hernia: containing the appendix vermiformis within the hernia sac
- skull.
- Double indirect hernia: an indirect inguinal hernia with two hernia sacs, without a concomitant direct hernia component (as seen in a pantaloon hernia).[26]
- Hiatus hernia: a hernia due to "short oesophagus" — insufficient elongation — stomach is displaced into the thorax
- Littre's hernia: a hernia involving a Meckel's diverticulum. It is named after the French anatomist Alexis Littré(1658–1726).
- Lumbar hernia: a hernia in the lumbar region (not to be confused with a lumbar disc hernia), contains the following entities:
- Jean Louis Petit(1674–1750).
- Grynfeltt's hernia: a hernia through Grynfeltt-Lesshaft triangle (superior lumbar triangle). It is named after physician Joseph Grynfeltt (1840–1913).
- Maydl's hernia: two adjacent loops of small intestine are within a hernial sac with a tight neck. The intervening portion of bowel within the abdomen is deprived of its blood supply and eventually becomes necrotic.
- Obturator hernia: hernia through obturator canal

- Parastomal hernias, which is when tissue protrudes adjacent to a stoma tract.
- Paraumbilical hernia: a type of umbilical hernia occurring in adults
- Perineal hernia: a perineal hernia protrudes through the muscles and fascia of the perineal floor. It may be primary but usually is acquired following perineal prostatectomy, abdominoperineal resection of the rectum, or pelvic exenteration.
- Properitoneal hernia: rare hernia located directly above the deep inguinal ringto the preperitoneal space.
- mesocolon.
- Richter's hernia: a hernia involving only one sidewall of the bowel, which can result in bowel strangulation leading to perforation through ischaemia without causing bowel obstruction or any of its warning signs. It is named after German surgeon August Gottlieb Richter (1742–1812).
- sliding hernias of the stomach.
- Sciatic hernia: this hernia in the sciaticneuralgia.
- superficial inguinal ring.
- Velpeau hernia: a hernia in the groin in front of the femoral blood vessels
Treatment

Truss
The benefits of the use of an external device to maintain reduction of the hernia without repairing the underlying defect (such as hernia trusses, trunks, belts, etc.) are unclear.[1]
Surgery
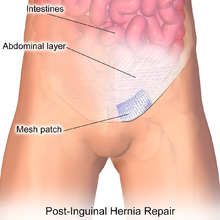
Surgery is recommended for some types of hernias to prevent complications such as obstruction of the bowel or strangulation of the tissue, although umbilical hernias and hiatus hernias may be watched, or are treated with medication.[34] Most abdominal hernias can be surgically repaired, but surgery has complications. Prior to surgery patients should be medically optimized receive guidance about changing factors that can be controlled, such as quitting smoking, managing medical conditions like diabetes effectively, and working on losing weight.
Three primary methods can be utilized: open surgery, laparoscopy, or robotic techniques. Fixing an inguinal hernia using laparoscopy causes less pain, speeds up recovery, and shows similar low rates of the hernia coming back compared to the traditional open repair method. However, open surgery can be done sometimes without general anesthesia. Using local anesthesia for open groin hernia repair, particularly in patients with additional health issues, leads to fewer complications and reduced costs.[35] Studies show that compared to regional or general anesthesia, local anesthesia results in less postoperative pain, shorter recovery times, and decreased unplanned overnight stays.[36] However, it might not be enough for repairing large hernias or in patients with abdominal domain loss, where general anesthesia is preferred.
| Advantages | Disadvantages |
|---|---|
|
Robot-assisted hernia surgery has also recently gained popularity as safe alternatives to open surgery. Robotic surgery for inguinal hernia repair shows outcomes comparable to laparoscopic surgery. The rates of overall complications, long-lasting postoperative pain, urinary retention, and 30-day re-admission are very similar between these two methods.[39] Just like in other areas of general surgery, it has been noted that robotic surgery for inguinal hernia repair takes more time in the operating room compared to the laparoscopic approach.[39]
Uncomplicated hernias are principally repaired by pushing back, or "reducing", the herniated tissue, and then mending the weakness in muscle tissue (an operation called herniorrhaphy). If complications have occurred, the surgeon will check the viability of the herniated organ and remove part of it if necessary.

Muscle reinforcement techniques often involve synthetic materials (a
Evidence suggests that tension-free methods (with or without mesh) often have lower percentage of recurrences and the fastest recovery period compared to
The frequency of surgical correction ranges from 10 per 100,000 (U.K.) to 28 per 100,000 (U.S.).[1] After elective surgery, the 30-day mortality rate for inguinal or femoral hernia repair stands at 0.1 percent, but it increases to 2.8 to 3.1 percent after urgent surgery.[42] When a bowel resection is part of the hernia repair, the mortality rate is even higher.[43] Older age, femoral hernias, female sex, and urgent repair are identified as other factors linked to a higher risk of mortality.[44]
Post-Operative Complications
Some complications from surgery in order of prevalence include a
Recovery
Many patients are managed through
References
- ^ PMID 25693015.
- ^ ISBN 9781451188509. Archivedfrom the original on 2017-08-22.
- ^ S2CID 7141090.
- ^ PMID 27733282.
- ^ PMID 27733281.
- ^ a b c "Hernia". MedlinePlus. U.S. National Library of Medicine. 9 August 2014. Archived from the original on 16 March 2015. Retrieved 12 March 2015.
- PMID 29018803.
- PMID 27115767.
- S2CID 22999363.
- PMID 8014965.
- PMID 37093073.
- ISBN 9788189866938. Archivedfrom the original on 2017-09-08.
- PMID 16679124.
- PMID 26063472.
- PMID 25530442.
- ^ Park AE, Roth JS, Kavic SM. Abdominal wall hernia. Curr Probl Surg. 2006 May;43(5):326-75. doi: 10.1067/j.cpsurg.2006.02.004. PMID 16679124.
- ^ "Inguinal hernia". The Mayo Clinic. Archived from the original on 2010-02-13. Retrieved 2010-05-24.
- ^ "What is Hernia? - Causes, Symptoms, Diagnosis". www.pristyncare.com. Retrieved 2023-12-16.
- ^ Lee HK, Park SJ, Yi BH (2010). "Multidetector CT reveals diverse variety of abdominal hernias". Diagnostic Imaging. 32 (5): 27–31. Archived from the original on 2010-06-18. Retrieved 2010-06-25.
- ISBN 978-0-7817-7447-5.
- ^ "Incarcerated". onlinedictionary.datasegment.com. Archived from the original on 2008-11-20. Citing: Webster 1913
- ^ "Hiatal Hernia Symptoms, Causes And Relation To Acid Reflux And Heartburn". Archived from the original on October 28, 2008. Retrieved 2010-05-24.
- ^ Balentine JR. Stöppler MC (ed.). "Hernia Causes". eMedicineHealth.com. WebMD. Archived from the original on 2010-05-31. Retrieved 2010-05-24.
- PMID 12697071.
- S2CID 205095374.
- ^ .
- PMID 26389785.
- PMID 19527083.
- S2CID 212739555.
- PMID 16552826.
- PMID 24497767.
- PMID 32476672.
- PMID 28638493.
- ^ "Hernia". U.K. National Health Service. Archived from the original on 2017-07-14. Retrieved 2017-07-23.
- PMID 33002663.
- S2CID 22487510.
- ^ ISBN 978-0-7817-7447-5.
- ^ a b "Overview | Laparoscopic surgery for inguinal hernia repair | Guidance | NICE". www.nice.org.uk. 2004-09-22. Retrieved 2023-11-09.
- ^ PMID 34609697.
- PMID 25337167.
- PMID 15184492.
- PMID 12549685.
- PMID 21680204.
- PMID 17414617.
- ^ PMID 21187992.
