Lyme disease
| Lyme disease | |
|---|---|
| Other names | Lyme borreliosis |
tiredness[1] | |
| Complications | Facial nerve paralysis, arthritis, meningitis,[1] Heart rhythm irregularities[2] |
| Usual onset | A week after a bite[1] |
| Causes | Borrelia spread by ticks[3] |
| Diagnostic method | Based on symptoms, tick exposure, blood tests[4] |
| Prevention | Prevention of tick bites (clothing the limbs, DEET), doxycycline[3] |
| Medication | Doxycycline, amoxicillin, ceftriaxone, cefuroxime[3] |
| Frequency | ~476k/year in U.S. (a likely overestimate), 200k/year in Europe[5][6][7] |
Lyme disease, also known as Lyme borreliosis, is a
Lyme disease is transmitted to humans by the bites of infected ticks of the genus Ixodes.
Prevention includes efforts to prevent tick bites by wearing clothing to cover the arms and legs and using
Lyme disease is the most common disease spread by ticks in the Northern Hemisphere.[21][7] Infections are most common in the spring and early summer.[3] Lyme disease was diagnosed as a separate condition for the first time in 1975 in Lyme, Connecticut. It was originally mistaken for juvenile rheumatoid arthritis.[22] The bacterium involved was first described in 1981 by Willy Burgdorfer.[23] Chronic symptoms following treatment are known as "post-treatment Lyme disease syndrome" (PTLDS).[20] PTLDS is different from chronic Lyme disease, a term no longer supported by scientists and used in different ways by different groups.[20][24] Some healthcare providers claim that PTLDS is caused by persistent infection, but this is not believed to be true because no evidence of persistent infection can be found after standard treatment.[25]
As of 2023[update] clinical trials of proposed human vaccines for Lyme disease were being carried out, but no vaccine was available. A vaccine, LYMERix, was produced, but discontinued in 2002 due to insufficient demand.[26] There are several vaccines for the prevention of Lyme disease in dogs.
Signs and symptoms
Lyme disease can produce a broad range of symptoms.
The incubation period is usually one to two weeks, but can be much shorter (days) or much longer (months to years).[33] Lyme symptoms most often occur from the month of May to September in the Northern Hemisphere because the nymphal stage of the tick is responsible for most cases.[33]
Early localized infection
80% of Lyme infections begin with a rash of some sort at the site of a tick bite, often near skin folds such as the
The rash is usually circular or oval, red or bluish, and may have an elevated or darker center.[3][28][29] This rash is termed an Erythema Migrans (EM) which translates as "Redness Migrating." In about 79% of cases in Europe, this rash gradually clears from the center toward the edges possibly forming a "bull's eye" or "target-like" pattern, but this clearing only happens in 19% of cases in endemic areas of the United States.[31][28][29] The rash may feel warm, usually is not itchy, is rarely tender or painful, and takes up to four weeks to resolve if untreated.[3]
The Lyme rash is often accompanied by symptoms of a flu-like illness, including fatigue, headache, body aches, fever, and chills [though usually neither nausea nor upper-respiratory problems]. These symptoms may also appear without a rash or linger after the rash has disappeared. Lyme can progress to later stages without a rash or these symptoms.[3]
People with high fever for more than two days or whose other symptoms of viral-like illness do not improve despite
Of course, not everyone with Lyme disease has all the symptoms, and many of these symptoms can occur with other diseases as well.[35]
Asymptomatic infection exists, but occurs in less than 7% of infected individuals in the United States.[36] Asymptomatic infection may be much more common among those infected in Europe.[37]
Early disseminated infection
Within days to weeks after the onset of local infection, the Borrelia bacteria may spread through the lymphatic system or bloodstream. In 10–20% of untreated cases, EM rashes develop at sites across the body that bear no relation to the original tick bite.[27] Transient muscle pains and joint pains are also common.[27]
In about 10–15% of untreated people, Lyme causes neurological problems known as
In North America, facial palsy is the typical early neuroborreliosis presentation, occurring in 5–10% of untreated people, in about 75% of cases accompanied by lymphocytic meningitis.
In about 4–10% of untreated cases in the U.S. and 0.3–4% of untreated cases in Europe, typically between June and December, about one month (range 4 days – 7 months) after the tick bite, the infection may cause heart complications known as Lyme
Another skin condition, found in Europe but not in North America, is
Late disseminated infection

Lyme arthritis occurs in up to 60% of untreated people, typically starting about six months after infection.[27] It usually affects only one or a few joints, often a knee or possibly the hip, other large joints, or the temporomandibular joint.[34][49] Usually, large joint effusion and swelling occur, but only mild or moderate pain.[34] Without treatment, swelling and pain typically resolve over time, but periodically return.[34] Baker's cysts may form and rupture.
In early US studies of Lyme disease, a rare peripheral neuropathy was described that included numbness, tingling, or burning starting at the feet or hands and over time possibly moving up the limbs. In a later analysis that discovered poor documentation of this manifestation, experts wondered if it exists at all in the US or is merely very rare.[34][50]
A neurologic syndrome called Lyme encephalopathy is associated with subtle memory and cognitive difficulties,
Acrodermatitis chronica atrophicans is a chronic skin disorder observed primarily in Europe among the elderly.[47] It begins as a reddish-blue patch of discolored skin, often on the backs of the hands or feet. The lesion slowly atrophies over several weeks or months, with the skin becoming first thin and wrinkled and then, if untreated, completely dry and hairless.[55] It is also associated with peripheral neuropathy.[50]
Cause

Lyme disease is caused by
B. burgdorferi sensu lato is a species complex made up of 20 accepted and three proposed genospecies. Eight species are known to cause Lyme disease: B. mayonii (found in North America), B. burgdorferi
Tick life cycle
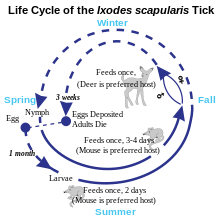

Three stages occur in the life cycle of a tick - larva, nymph, and adult. During the nymph stage, ticks most frequently transmit Lyme disease and are usually most active in late spring and early summer in regions where the climate is mild. During the adult stage, Lyme disease transmission is less common because adult ticks are less likely to bite humans and tend to be larger in size, so can be easily seen and removed.[62]
Transmission
Lyme disease is classified as a
Within the tick midgut, the Borrelia's outer surface protein A (OspA) binds to the tick receptor for OspA, known as TROSPA. When the tick feeds, the Borrelia downregulates OspA and upregulates OspC, another surface protein. After the bacteria migrate from the midgut to the salivary glands, OspC binds to Salp15, a tick salivary protein that appears to have immunosuppressive effects that enhance infection.[70] Successful infection of the mammalian host depends on bacterial expression of OspC.[71]
Tick bites often go unnoticed because of the small size of the tick in its nymphal stage, as well as tick secretions that prevent the host from feeling any itch or pain from the bite. However, transmission is quite rare, with only about 1.2 to 1.4 percent of recognized tick bites resulting in Lyme disease.[72]
While
Budding research has suggested that B. burgdorferi sensu lato may also be able to form enzootic cycle among lizard populations;[74] this was previously assumed not to be possible in major areas containing populations of lizards, such as California. Except for one study in Europe,[73] much of the data implicating lizards is based on DNA detection of the spirochete and has not demonstrated that lizards are able to infect ticks feeding upon them.[74][75][76][77] As some experiments suggest lizards are refractory to infection with Borrelia, it appears likely their involvement in the enzootic cycle is more complex and species-specific.[78]

In Europe, the main vector is
The lone star tick (
On the
Transmission can occur across the placenta during pregnancy and as with a number of other spirochetal diseases, adverse pregnancy outcomes are possible with untreated infection; prompt treatment with antibiotics reduces or eliminates this risk.[85][86][87][88]
There is no scientific evidence to support Lyme disease transmission via blood transfusion, sexual contact, or breast milk.[89]
Tick-borne co-infections
Ticks that transmit B. burgdorferi to humans can also carry and transmit several other microbes, such as Babesia microti and Anaplasma phagocytophilum, which cause the diseases babesiosis and human granulocytic anaplasmosis (HGA), respectively.[90] Among people with early Lyme disease, depending on their location, 2–12% will also have HGA and 2–10% will have babesiosis.[54] Ticks in certain regions also transmit viruses that cause tick-borne encephalitis and Powassan virus disease.[91][54] Co-infections of Lyme disease may not require additional treatment, since they may resolve on their own or—as in the case of HGA—can be treated with the doxycycline prescribed for Lyme.[34] Persistent fever or compatible anomalous laboratory findings may be indicative of a co-infection.[54]
Pathophysiology
B. burgdorferi can spread throughout the body during the course of the disease, and has been found in the skin, heart, joints, peripheral nervous system, and central nervous system.[71][92] B. Burgdorferi does not produce toxins.[93] Therefore, many of the signs and symptoms of Lyme disease are a consequence of the immune response to spirochete in those tissues.[94]
B. burgdorferi is injected into the skin by the bite of an infected Ixodes tick.
Days to weeks following the tick bite, the spirochetes spread via the bloodstream to joints, heart, nervous system, and distant skin sites, where their presence gives rise to the variety of symptoms of the disseminated disease. The spread of B. burgdorferi is aided by the attachment of the host protease plasmin to the surface of the spirochete.[98]
If untreated, the bacteria may persist in the body for months or even years, despite the production of B. burgdorferi antibodies by the immune system.[99] The spirochetes may avoid the immune response by decreasing expression of surface proteins that are targeted by antibodies, antigenic variation of the VlsE surface protein, inactivating key immune components such as complement, and hiding in the extracellular matrix, which may interfere with the function of immune factors.[100][101]
Immunological studies
Exposure to the Borrelia bacterium during Lyme disease possibly causes a long-lived and damaging
Chronic symptoms from an autoimmune reaction could explain why some symptoms persist even after the spirochetes have been eliminated from the body. This hypothesis may explain why chronic arthritis persists after antibiotic therapy, similar to rheumatic fever, but its wider application is controversial.[106][107]
Diagnosis
Lyme disease is
In the absence of an EM rash or history of tick exposure, Lyme diagnosis depends on laboratory confirmation.
In some cases, when history, signs, and symptoms are strongly suggestive of early disseminated Lyme disease,
Laboratory testing
Tests for antibodies in the blood by ELISA and Western blot is the most widely used method for Lyme diagnosis. A two-tiered protocol is recommended by the Centers for Disease Control and Prevention (CDC): the sensitive ELISA test is performed first, and if it is positive or equivocal, then the more specific Western blot is run.[115] The immune system takes some time to produce antibodies in quantity. After Lyme infection onset, antibodies of types IgM and IgG usually can first be detected respectively at 2–4 weeks and 4–6 weeks, and peak at 6–8 weeks.[116] When an EM rash first appears, detectable antibodies may not be present. Therefore, it is recommended that testing not be performed and diagnosis be based on the presence of the EM rash.[34] Up to 30 days after suspected Lyme infection onset, infection can be confirmed by detection of IgM or IgG antibodies; after that, it is recommended that only IgG antibodies be considered.[116] A positive IgM and negative IgG test result after the first month of infection is generally indicative of a false-positive result.[117] The number of IgM antibodies usually collapses 4–6 months after infection, while IgG antibodies can remain detectable for years.[116]
Other tests may be used in neuroborreliosis cases. In Europe, neuroborreliosis is usually caused by
In Lyme carditis, electrocardiograms are used to evidence heart conduction abnormalities, while echocardiography may show myocardial dysfunction.[45] Biopsy and confirmation of Borrelia cells in myocardial tissue may be used in specific cases but are usually not done because of risk of the procedure.[45]
Several other forms of laboratory testing for Lyme disease are available, some of which have not been adequately validated. OspA antigens, shed by live Borrelia bacteria into urine, are a promising technique being studied.[123] The use of nanotrap particles for their detection is being looked at and the OspA has been linked to active symptoms of Lyme.[124][125] High titers of either immunoglobulin G (IgG) or immunoglobulin M (IgM) antibodies to Borrelia antigens indicate disease, but lower titers can be misleading, because the IgM antibodies may remain after the initial infection, and IgG antibodies may remain for years.[126]
The CDC does not recommend urine antigen tests, PCR tests on urine, immunofluorescent staining for cell-wall-deficient forms of B. burgdorferi, and lymphocyte transformation tests.[121]
Imaging
Neuroimaging is controversial in whether it provides specific patterns unique to neuroborreliosis, but may aid in differential diagnosis and in understanding the pathophysiology of the disease.[127] Though controversial, some evidence shows certain neuroimaging tests can provide data that are helpful in the diagnosis of a person. Magnetic resonance imaging (MRI) and single-photon emission computed tomography (SPECT) are two of the tests that can identify abnormalities in the brain of a person affected with this disease. Neuroimaging findings in an MRI include lesions in the periventricular white matter, as well as enlarged ventricles and cortical atrophy. The findings are considered somewhat unexceptional because the lesions have been found to be reversible following antibiotic treatment. Images produced using SPECT show numerous areas where an insufficient amount of blood is being delivered to the cortex and subcortical white matter. However, SPECT images are known to be nonspecific because they show a heterogeneous pattern in the imaging. The abnormalities seen in the SPECT images are very similar to those seen in people with cerebral vasculitis and Creutzfeldt–Jakob disease, which makes them questionable.[128]
Differential diagnosis
Community clinics have been reported to misdiagnose 23–28% of
Unlike
Lyme radiculopathy affecting the limbs is often misdiagnosed as a radiculopathy caused by nerve root compression, such as sciatica.[112][130] Although most cases of radiculopathy are compressive and resolve with conservative treatment (e.g., rest) within 4–6 weeks, guidelines for managing radiculopathy recommend first evaluating risks of other possible causes that, although less frequent, require immediate diagnosis and treatment, including infections such as Lyme and shingles.[131] A history of outdoor activities in likely tick habitats in the last 3 months possibly followed by a rash or viral-like symptoms, and current headache, other symptoms of lymphocytic meningitis, or facial palsy would lead to suspicion of Lyme disease and recommendation of serological and lumbar puncture tests for confirmation.[131]
Lyme radiculopathy affecting the trunk can be misdiagnosed as myriad other conditions, such as diverticulitis and acute coronary syndrome.[44][112] Diagnosis of late-stage Lyme disease is often complicated by a multifaceted appearance and nonspecific symptoms, prompting one reviewer to call Lyme the new "great imitator".[132] As all people with later-stage infection will have a positive antibody test, simple blood tests can exclude Lyme disease as a possible cause of a person's symptoms.[133]
Prevention
Tick bites may be prevented by avoiding or reducing time in likely tick habitats and taking precautions while in and when getting out of one.[134][8]
Most Lyme human infections are caused by
As a precaution, CDC recommends soaking or spraying clothes, shoes, and camping gear such as tents, backpacks and sleeping bags with 0.5% permethrin solution and hanging them to dry before use.[134][139] Permethrin is odorless and safe for humans but highly toxic to ticks.[140] After crawling on permethrin-treated fabric for as few as 10–20 seconds, tick nymphs become irritated and fall off or die.[140][141] Permethrin-treated closed-toed shoes and socks reduce by 74 times the number of bites from nymphs that make first contact with a shoe of a person also wearing treated shorts (because nymphs usually quest near the ground, this is a typical contact scenario).[140] Better protection can be achieved by tucking permethrin-treated trousers (pants) into treated socks and a treated long-sleeve shirt into the trousers so as to minimize gaps through which a tick might reach the wearer's skin.[138] Light-colored clothing may make it easier to see ticks and remove them before they bite.[138] Military and outdoor workers' uniforms treated with permethrin have been found to reduce the number of bite cases by 80–95%.[141] Permethrin protection lasts several weeks of wear and washings in customer-treated items and up to 70 washings for factory-treated items.[139] Permethrin should not be used on human skin, underwear or cats.[139][142]
The
After coming indoors, clothes, gear and pets should be checked for ticks.[134] Clothes can be put into a hot dryer for 10 minutes to kill ticks (just washing or warm dryer are not enough).[134] Showering as soon as possible, looking for ticks over the entire body, and removing them reduce risk of infection.[134] Unfed tick nymphs are the size of a poppy seed, but a day or two after biting and attaching themselves to a person, they look like a small blood blister.[145] The following areas should be checked especially carefully: armpits, between legs, back of knee, bellybutton, trunk, and in children ears, neck and hair.[134]
Tick removal

Attached ticks should be removed promptly. Risk of infection increases with time of attachment, but in North America risk of Lyme disease is small if the tick is removed within 36 hours.[146] CDC recommends inserting a fine-tipped tweezer between the skin and the tick, grasping very firmly, and pulling the closed tweezer straight away from the skin without twisting, jerking, squeezing or crushing the tick.[147] After tick removal, any tick parts remaining in the skin should be removed with a clean tweezer, if possible.[147] The wound and hands should then be cleaned with alcohol or soap and water.[147] The tick may be disposed by placing it in a container with alcohol, sealed bag, tape or flushed down the toilet.[147] The bitten person should write down where and when the bite happened so that this can be informed to a doctor if the person gets a rash or flu-like symptoms in the following several weeks.[147] CDC recommends not using fingers, nail polish, petroleum jelly or heat on the tick to try to remove it.[147]
In Australia, where the Australian paralysis tick is prevalent, the Australasian Society of Clinical Immunology and Allergy recommends not using tweezers to remove ticks, because if the person is allergic, anaphylaxis could result.[148] Instead, a product should be sprayed on the tick to cause it to freeze and then drop off.[148] Another method consists in using about 20 cm of dental floss or fishing line for slowly tying an overhand knot between the skin and the tick and then pulling it away from the skin.[149][150]
Preventive antibiotics
The risk of infectious transmission increases with the duration of tick attachment.[27] It requires between 36 and 48 hours of attachment for the bacteria that causes Lyme to travel from within the tick into its saliva.[27] If a deer tick that is sufficiently likely to be carrying Borrelia is found attached to a person and removed, and if the tick has been attached for 36 hours or is engorged, a single dose of doxycycline administered within the 72 hours after removal may reduce the risk of Lyme disease. It is not generally recommended for all people bitten, as development of infection is rare: about 50 bitten people would have to be treated this way to prevent one case of erythema migrans (i.e. the typical rash found in about 70–80% of people infected).[3][27]
Garden landscaping
Several landscaping practices may reduce the risk of tick bites in residential yards.
Occupational exposure
Outdoor workers are at risk of Lyme disease if they work at sites with infected ticks. This includes construction, landscaping, forestry, brush clearing, land surveying, farming, railroad work, oil field work, utility line work, park or wildlife management.
Host animals
Ticks can feed upon the blood of a wide array of possible host species, including
In the United States, one approach to reducing the incidence of Lyme and other deer tick-borne diseases has been to greatly reduce the deer population on which the adult ticks depend for feeding and reproduction. Lyme disease cases fell following deer eradication on an island, Monhegan, Maine,[156] and following deer control in Mumford Cove, Connecticut.[157] Advocates have suggested reducing the deer population to levels of 8 to 10 deer per square mile, compared to levels of 60 or more deer per square mile in the areas of the country with the highest Lyme disease rates.[158]
Others have noted that while deer are reproductive hosts, they are not Borrelia burgdorferi reservoirs. Researchers have suggested that smaller, less obviously visible Lyme reservoirs, like
Tick-borne diseases are estimated to affect ~80 % of cattle worldwide.[159] They also affect cats, dogs, and other pets. Routine veterinary control of ticks of domestic animals through the use of acaricides has been suggested as a way to reduce exposure of humans to ticks. However, chemical control with acaricides is now criticized on a number of grounds. Ticks appear to develop resistance to acaricides; acaricides are costly; and there are concerns over their toxicity and the potential for chemical residues to affect food and the environment.[160]
In Europe, known reservoirs of Borrelia burgdorferi were 9 small mammals, 7 medium-sized mammals and 16 species of birds (including passerines, sea-birds and pheasants).
Vaccination
As of 2023[update] no human vaccines for Lyme disease were available.[26] The only human vaccine to advance to market was LYMErix, which was available from 1998, but discontinued in 2002.[166] The vaccine candidate VLA15 was scheduled to start a phase 3 trial in the third quarter of 2022, with other research ongoing. Multiple vaccines are available for the prevention of Lyme disease in dogs.
LYMErix
The vaccine LYMErix was available from 1998 to 2002. The
Following approval of the
Despite the lack of evidence that the complaints were caused by the vaccine, sales plummeted and LYMErix was withdrawn from the U.S. market by GlaxoSmithKline in February 2002,
VLA15
The hexavalent (OspA) protein subunit-based vaccine candidate VLA15 was developed by
A phase 3 trial of VLA15 was scheduled for late 2022, recruiting volunteers at test sites located across the northeastern United States and in Europe.[178][179] Participants were scheduled to receive an initial three-dose series of vaccines over the course of five to nine months, followed by a booster dose after twelve months, with both the initial series and the booster dose scheduled to be complete before the year's peak Lyme disease season.[179]
Other research
An mRNA vaccine designed to cause a strong fast immune response to tick saliva allowed the immune system to detect and remove the ticks from test animals before they were able to transmit the infectious bacteria.[180] The vaccine contains mRNAs for the body to build 19 proteins in tick saliva which, by enabling quick development of erythema (itchy redness) at the bite site, protects guinea pigs against Lyme disease. It also protected the test animals if the tick is not removed if only one tick, but not three, remain attached.[181][182]
Canine vaccines
Treatment
Treatment regimens for Lyme disease range from 14 days in early localized disease, to 14–21 days in early disseminated disease to 14–28 days in late disseminated disease.[184] Neurologic complications of Lyme disease may be treated with doxycycline as it can be taken by mouth and has a lower cost, although in North America evidence of efficacy is only indirect.[119] In case of failure, guidelines recommend retreatment with injectable ceftriaxone.[119] Several months after treatment for Lyme arthritis, if joint swelling persists or returns, a second round of antibiotics may be considered; intravenous antibiotics are preferred for retreatment in case of poor response to oral antibiotics.[27][34] Outside of that, a prolonged antibiotic regimen lasting more than 28 days is not recommended as no evidence shows it to be effective.[27][185] IgM and IgG antibody levels may be elevated for years even after successful treatment with antibiotics.[27] As antibody levels are not indicative of treatment success, testing for them is not recommended.[27]
Facial palsy may resolve without treatment; however, antibiotic treatment is recommended to stop other Lyme complications.[34] Corticosteroids are not recommended when facial palsy is caused by Lyme disease.[43] In those with facial palsy, frequent use of artificial tears while awake is recommended, along with ointment and a patch or taping the eye closed when sleeping.[43][186]
About a third of people with Lyme carditis need a temporary pacemaker until their heart conduction abnormality resolves, and 21% need to be hospitalized.[45] Lyme carditis should not be treated with corticosteroids.[45]
People with Lyme arthritis should limit their level of physical activity to avoid damaging affected joints, and in case of limping should use crutches.
People receiving treatment should be advised that reinfection is possible and how to prevent it.[114]
Prognosis
Lyme disease's typical first sign, the erythema migrans (EM) rash, resolves within several weeks even without treatment.[3] However, in untreated people, the infection often disseminates to the nervous system, heart, or joints, possibly causing permanent damage to body tissues.[34]
People who receive recommended antibiotic treatment within several days of appearance of an initial EM rash have the best prospects.[112] Recovery may not be total or immediate. The percentage of people achieving full recovery in the United States increases from about 64–71% at end of treatment for EM rash to about 84–90% after 30 months; higher percentages are reported in Europe.[188][189] Treatment failure, i.e. persistence of original or appearance of new signs of the disease, occurs only in a few people.[188] Remaining people are considered cured but continue to experience subjective symptoms, e.g. joint or muscle pains or fatigue.[190] These symptoms usually are mild and nondisabling.[190]
People treated only after nervous system manifestations of the disease may end up with objective neurological deficits, in addition to subjective symptoms.[34] In Europe, an average of 32–33 months after initial Lyme symptoms in people treated mostly with doxycycline 200 mg for 14–21 days, the percentage of people with lingering symptoms was much higher among those diagnosed with neuroborreliosis (50%) than among those with only an EM rash (16%).[191] In another European study, 5 years after treatment for neuroborreliosis, lingering symptoms were less common among children (15%) than adults (30%), and in the latter was less common among those treated within 30 days of the first symptom (16%) than among those treated later (39%); among those with lingering symptoms, 54% had daily activities restricted and 19% were on sick leave or incapacitated.[192]
Some data suggest that about 90% of Lyme
In Europe, about a quarter of people with
Recovery from late neuroborreliosis tends to take longer and be less complete than from early neuroborreliosis, probably because of irreversible neurologic damage.[34]
About half the people with Lyme carditis progress to complete heart block, but it usually resolves in a week.[45] Other Lyme heart conduction abnormalities resolve typically within 6 weeks.[45] About 94% of people have full recovery, but 5% need a permanent pacemaker and 1% end up with persistent heart block (the actual percentage may be higher because of unrecognized cases).[45] Lyme myocardial complications usually are mild and self-limiting.[45] However, in some cases Lyme carditis can be fatal.[45]
Recommended antibiotic treatments are effective in about 90% of Lyme arthritis cases, although it can take several months for inflammation to resolve and a second round of antibiotics is often necessary.
Reinfection is not uncommon. In a U.S. study, 6–11% of people treated for an EM rash had another EM rash within 30 months.[188] The second rash typically is due to infection by a different Borrelia strain.[197]
Post-treatment Lyme disease syndrome
Chronic symptoms like pain, fatigue, or cognitive impairment are experienced by 10–20% of people who contract Lyme disease, even after completing treatment. This is called Post-treatment Lyme disease syndrome, or PTLDS.[198][199]
The cause is unknown. One hypothesis is that a persistent, difficult-to-detect infection remains. Work with mice, dogs, and non-human primates have shown evidence of persistent B. burgdorferi, although these remaining bacteria are hard to cultivate and Koch's postulates are hard to prove. Another hypothesis is that autoimmunity has been triggered by the infection. Auto–immune responses are known to occur following other infections, including Campylobacter (
There is no proven treatment for Post-treatment Lyme disease syndrome. While short-term antibiotics are effective in early Lyme disease, prolonged antibiotics are not. They have been shown ineffective in placebo-controlled trials and carry the risk of serious, sometimes deadly complications. Generally, treatment is symptomatic and is similar to the management of
Epidemiology

Lyme disease occurs regularly in Northern Hemisphere temperate regions.[201] An estimated 476,000 people a year are diagnosed and treated for the disease in the United States. This number is likely an overestimate due to overdiagnosis and overtreatment.[5][6] Over 200,000 people a year are diagnosed and treated in Europe.[7][3][202] There is a suggestion that tick populations and Lyme disease occurrence are increasing and spreading into new areas, due in part to the warming temperatures of climate change. However, tick-borne disease systems are complex, and determining whether changes are due to climate change or other drivers can be difficult.[155][203] Lyme disease effects are comparable among males and females. A wide range of age groups is affected, though the number of cases is highest among 10- to 19-year-olds.
Africa
In northern Africa, B. burgdorferi sensu lato has been identified in Morocco, Algeria, Egypt and Tunisia.[204][205][206]
Lyme disease in sub-Saharan Africa is presently unknown, but evidence indicates it may occur in humans in this region. The abundance of hosts and tick vectors would favor the establishment of Lyme infection in Africa.[207] In East Africa, two cases of Lyme disease have been reported in Kenya.[208] According The Federation of Infectious Diseases Societies of Southern Africa, Lyme disease is not known to be endemic in either South Africa or Mozambique.[209]
Asia
B. burgdorferi sensu lato-infested ticks are being found more frequently in Japan, as well as in northwest China, Nepal, Thailand and far eastern Russia.[210][211] Borrelia has also been isolated in Mongolia.[212]
Australia
Lyme disease is not considered endemic to Australia.[213] While there have been reports of people acquiring Lyme disease in Australia, and even evidence of closely related Borrelia species in ticks,[214] the evidence linking these cases to local transmission is limited. Ongoing research on resolving potential Borrelia species to Debilitating Symptom Complexes Attributed to Ticks (DSCATT) in Australia are ongoing.[215]
Europe
In Europe, Lyme disease is caused by infection with one or more pathogenic European genospecies of the spirochaete B. burgdorferi sensu lato, mainly transmitted by the tick Ixodes ricinus.[216] Cases of B. burgdorferi sensu lato-infected ticks are found predominantly in central Europe, particularly in Slovenia and Austria, but have been isolated in almost every country on the continent.[217] Number of cases in southern Europe, such as Italy and Portugal, is much lower.[218] Diagnosed cases in some Western countries, such as Iceland, are rising.[219] Lyme disease is rare in Iceland. On average around 6 to 7 cases are diagnosed every year, primarily localised infections presenting as erythema migrans. None of the cases had a definitive Icelandic origin and the yearly number of cases has not been increasing.[220]
United Kingdom
In the United Kingdom the number of laboratory-confirmed cases of Lyme disease has been rising steadily since voluntary reporting was introduced in 1986[221] when 68 cases were recorded in the UK and Ireland combined.[222] In the UK there were 23 confirmed cases in 1988 and 19 in 1990,[223] but 973 in 2009[221] and 953 in 2010.[224] Provisional figures for the first 3 quarters of 2011 show a 26% increase on the same period in 2010.[225]
It is thought, however, that the actual number of cases is significantly higher than suggested by the above figures, with the UK's Health Protection Agency estimating that there are between 2,000 and 3,000 cases per year,[224] (with an average of around 15% of the infections acquired overseas[221]), while Dr Darrel Ho-Yen, Director of the Scottish Toxoplasma Reference Laboratory and National Lyme Disease Testing Service, believes that the number of confirmed cases should be multiplied by 10 "to take account of wrongly diagnosed cases, tests giving false results, sufferers who weren't tested, people who are infected but not showing symptoms, failures to notify and infected individuals who don't consult a doctor."[226][227]
Despite Lyme disease (Borrelia burgdorferi infection) being a notifiable disease in Scotland[228] since January 1990[229] which should therefore be reported on the basis of clinical suspicion, it is believed that many GPs are unaware of the requirement.[230] Mandatory reporting, limited to laboratory test results only, was introduced throughout the UK in October 2010, under the Health Protection (Notification) Regulations 2010.[221]
Although there is a greater number of cases of Lyme disease in the
Tests on pet dogs carried out throughout the country in 2009 indicated that around 2.5% of ticks in the UK may be infected, considerably higher than previously thought.
North America
Many studies in North America have examined ecological and environmental correlates of the number of people affected by Lyme disease. A 2005 study using climate suitability modelling of I. scapularis projected that climate change would cause an overall 213% increase in suitable vector habitat by 2080, with northward expansions in Canada, increased suitability in the central U.S., and decreased suitable habitat and vector retraction in the southern U.S.[239] A 2008 review of published studies concluded that the presence of forests or forested areas was the only variable that consistently elevated the risk of Lyme disease whereas other environmental variables showed little or no concordance between studies.[240] The authors argued that the factors influencing tick density and human risk between sites are still poorly understood, and that future studies should be conducted over longer time periods, become more standardized across regions, and incorporate existing knowledge of regional Lyme disease ecology.[240]
Canada
The range of ticks able to carry Lyme disease has expanded from a limited area of Ontario to include areas of southern Quebec, Manitoba, northern Ontario, southern New Brunswick, southwest Nova Scotia and limited parts of Saskatchewan and Alberta, as well as British Columbia. Cases have been reported as far east as the island of Newfoundland.[111][241][242][243] A model-based prediction by Leighton et al. (2012) suggests that the range of the I. scapularis tick will expand into Canada by 46 km/year over the next decade, with warming climatic temperatures as the main driver of increased speed of spread.[244]
Mexico
A 2007 study suggests Borrelia burgdorferi infections are endemic to Mexico, from four cases reported between 1999 and 2000.[245]
United States
Lyme disease is the most common tick-borne disease in North America and Europe, and one of the fastest-growing infectious diseases in the United States. Of cases reported to the United States CDC, the ratio of Lyme disease infection is 7.9 cases for every 100,000 persons. In the ten states where Lyme disease is most common, the average was 31.6 cases for every 100,000 persons for the year 2005.[246][247][248]
Although Lyme disease has been reported in all states due to travel-associated infections, about 99% of all reported cases are confined to just five geographic areas (New England, Mid-Atlantic, East-North Central, South Atlantic, and West North-Central).[89][249][250] CDC implemented national surveillance of Lyme disease cases in 1991. Since then, reporting criteria has been modified multiple times.[251] The 2022 surveillance case definition classifies cases as confirmed, probable, and suspect.[252] The number of reported cases of the disease has been increasing, as are endemic regions in North America.
The CDC emphasizes that, while surveillance data has limitations, it is useful due to "uniformity, simplicity, and timeliness." While cases are under-reported in high-incidence areas, over-reporting is likely in low-incidence areas. Additionally, surveillance cases are reported by county of residence and not where an infection was necessarily contracted.[253][89]
Several similar but apparently distinct conditions may exist, caused by various species or subspecies of Borrelia in North America. A regionally restricted condition that may be related to Borrelia infection is southern tick-associated rash illness (STARI), also known as Masters disease. Amblyomma americanum, known commonly as the lone-star tick, is recognized as the primary vector for STARI. In some parts of the geographical distribution of STARI, Lyme disease is quite rare (e.g., Arkansas), so people in these regions experiencing Lyme-like symptoms—especially if they follow a bite from a lone-star tick—should consider STARI as a possibility. It is generally a milder condition than Lyme and typically responds well to antibiotic treatment.[254]
In recent years there have been 5 to 10 cases a year of a disease similar to Lyme occurring in Montana. It occurs primarily in pockets along the Yellowstone River in central Montana. People have developed a red bull's-eye rash around a tick bite followed by weeks of fatigue and a fever.[250]
South America
In Brazil, a Lyme-like disease known as Baggio–Yoshinari syndrome was identified, caused by microorganisms that do not belong to the B. burgdorferi sensu lato complex and transmitted by ticks of the Amblyomma and Rhipicephalus genera.[255] The first reported case of BYS in Brazil was made in 1992 in Cotia, São Paulo.[256]
Etymology
Lyme disease was diagnosed as a separate condition for the first time in 1975 in Lyme, Connecticut.[257]
History
The evolutionary history of Borrelia burgdorferi genetics has been the subject of recent studies. One study has found that prior to the
John Josselyn, who visited New England in 1638 and again from 1663 to 1670, wrote "there be infinite numbers of ticks hanging upon the bushes in summertime that will cleave to man's garments and creep into his breeches, eating themselves in a short time into the very flesh of a man. I have seen the stockings of those that have gone through the woods covered with them."[259]
This is also confirmed by the writings of
Perhaps the first detailed description of what is now known as Lyme disease appeared in the writings of John Walker after a visit to the island of Jura (Deer Island) off the west coast of Scotland in 1764.[261] He gives a good description both of the symptoms of Lyme disease (with "exquisite pain [in] the interior parts of the limbs") and of the tick vector itself, which he describes as a "worm" with a body which is "of a reddish color and of a compressed shape with a row of feet on each side" that "penetrates the skin". Many people from this area of Great Britain emigrated to North America between 1717 and the end of the 18th century.[citation needed]
The examination of preserved museum specimens has found Borrelia DNA in an infected
The early European studies of what is now known as Lyme disease described its skin manifestations. The first study dates to 1883 in
At a 1909 research conference, Swedish dermatologist
The modern history of medical understanding of the disease, including its cause, diagnosis, and treatment, has been difficult.[265]
Neurological problems following tick bites were recognized starting in the 1920s. French physicians Garin and Bujadoux described a farmer with a painful sensory
Carl Lennhoff, who worked at the Karolinska Institute in Sweden, believed many skin conditions were caused by spirochetes. In 1948, he used a special stain to microscopically observe what he believed were spirochetes in various types of skin lesions, including EM.[267] Although his conclusions were later shown to be erroneous, interest in the study of spirochetes was sparked. In 1949, Nils Thyresson, who also worked at the Karolinska Institute, was the first to treat ACA with penicillin.[268] In the 1950s, the relationship among tick bite, lymphocytoma, EM and Bannwarth's syndrome was recognized throughout Europe leading to the widespread use of penicillin for treatment in Europe.[269][270]
In 1970, a dermatologist in Wisconsin named Rudolph Scrimenti recognized an EM lesion in a person after recalling a paper by Hellerström that had been reprinted in an American science journal in 1950. This was the first documented case of EM in the United States. Based on the European literature, he treated the person with penicillin.[271]
The full
Before 1976, the elements of B. burgdorferi sensu lato infection were called or known as tick-borne meningopolyneuritis, Garin-Bujadoux syndrome, Bannwarth syndrome, Afzelius's disease,[275] Montauk Knee or sheep tick fever. Since 1976 the disease is most often referred to as Lyme disease,[276][277] Lyme borreliosis or simply borreliosis.[278][279]
In 1980, Steere, et al., began to test
After the identification of B. burgdorferi as the causative agent of Lyme disease, antibiotics were selected for testing, guided by in vitro antibiotic sensitivities, including tetracycline antibiotics, amoxicillin, cefuroxime axetil, intravenous and intramuscular penicillin and intravenous ceftriaxone.[283][284] The mechanism of tick transmission was also the subject of much discussion. B. burgdorferi spirochetes were identified in tick saliva in 1987, confirming the hypothesis that transmission occurred via tick salivary glands.[285]
Society, culture, & controversy
Landscape changes & urbanization
Urbanization and other
The dilution effect
Given these habitat-host dynamics, some researchers have begun to postulate whether the dilution effect could mitigate the spread of Lyme disease.[286] The dilution effect is a hypothesis that predicts that an increase in host biodiversity will result in a decrease in the number of vectors infected with B. burgdorferi.[286] Scientific research has shown that nymphal infection prevalence (NIP) decreases as the number of host species increases, supporting the dilution effect.[286] That said, these findings should not be misinterpreted to suggest that there is a direct relationship between decreased NIP and decreased epidemiological risk, as this has yet to be proven.[286] Additionally, it is important to note that, thus far, the dilution effect is only supported in the Northeastern United States, and has been disproved in other parts of the world that also experience high Lyme disease incidence rates [289]
Chronic Lyme disease
The term "chronic Lyme disease" is controversial and not recognized in the medical literature,
The 2008 documentary Under Our Skin is known for promoting controversial and unrecognized theories about "chronic Lyme disease".[293]
Other animals
Dogs
Prevention of Lyme disease is an important step in keeping dogs safe in endemic areas. Prevention education and a number of preventive measures are available. First, for dog owners who live near or who often frequent tick-infested areas, routine vaccinations of their dogs is an important step.[294]
Another crucial preventive measure is the use of persistent acaricides, such as topical repellents or pesticides that contain triazapentadienes (
Examination of a dog for ticks after being in a tick-infested area is an important precautionary measure to take in the prevention of Lyme disease. Key spots to examine include the head, neck, and ears.[296]
In dogs, a serious long-term prognosis may result in glomerular disease,[297] which is a category of kidney damage that may cause chronic kidney disease.[183] Dogs may also experience chronic joint disease if the disease is left untreated. However, the majority of cases of Lyme disease in dogs result in complete recovery with, and sometimes without, treatment with antibiotics.[298][verification needed] In rare cases, Lyme disease can be fatal to both humans and dogs.[299]
Cats
Unlike dogs, it is very rare for a cat to be infected with Lyme disease. However, cats are nevertheless capable of being infected with B. burgdorferi , following a bite from an infected tick. Cats who are infected with Lyme Disease may show symptoms including but not limited to lameness, fatigue, or loss of appetite.[300] In two cases, the infected cats experienced cardiac irregularities similar to symptoms of Lyme in both dogs and humans.[301] However, cats who are infected with Lyme disease are likely to be asymptomatic, and show no noticeable signs of the disease.[301][300] Cats with Lyme are often treated with antibiotics, much like other animals. In some cases, additional treatment or therapy may be required.[300]
Horses
While Lyme disease can occur in horses, not every infection with B. burgdorferi is associated with symptoms.[302] Especially, detection of specific antibodies against B. burgdorferi alone is not sufficient for a diagnosis of equine Lyme disease and unspecific testing for antibodies is not recommended.[303]
References
- ^ a b c d e f g h i j k "Signs and Symptoms of Lyme Disease". cdc.gov. 11 January 2013. Archived from the original on 16 January 2013. Retrieved 2 March 2015.
- ^ "Lyme disease - Symptoms and causes". Mayo Clinic. Retrieved 7 June 2022.
- ^ PMID 24785207. Archived from the original(PDF) on 21 August 2016. Retrieved 5 July 2016.
- ^ a b "Lyme Disease Diagnosis and Testing". cdc.gov. 10 January 2013. Archived from the original on 2 March 2015. Retrieved 2 March 2015.
- ^ a b "How many people get Lyme disease?". Centers for Disease Control and Prevention. 13 January 2021. Retrieved 11 January 2023.
- ^ PMID 33496229.
- ^ PMID 34286689.
- ^ a b c Wenner M (11 June 2021). "Let's Do a Tick Check - These pervasive bloodsuckers can give you more than just Lyme disease. Here's how to protect yourself. (Interactive)". The New York Times. Retrieved 19 June 2021.
- ^ PMID 34161868.
- PMID 19486523.
- PMID 25999226.
- from the original on 7 February 2009.
- ^ a b "Lyme disease transmission". cdc.gov. 11 January 2013. Archived from the original on 3 March 2015. Retrieved 2 March 2015.
- ^ PMID 27976670.
- ECDC. Archived(PDF) from the original on 29 September 2018. Retrieved 29 September 2018.
- ^ PMID 26856777.
- ^ "Two-step Laboratory Testing Process". cdc.gov. 15 November 2011. Archived from the original on 12 March 2015. Retrieved 2 March 2015.
- ^ "Testing of Ticks". cdc.gov. 4 June 2013. Archived from the original on 19 February 2015. Retrieved 2 March 2015.
Although some commercial groups offer testing, in general it is not recommended
- ^ "Tick Removal". cdc.gov. 23 June 2014. Archived from the original on 10 March 2015. Retrieved 2 March 2015.
- ^ a b c "Post-Treatment Lyme Disease Syndrome". cdc.gov. 1 December 2017. Archived from the original on 27 February 2015. Retrieved 20 June 2018.
- ISBN 978-1-4289-1143-7. Archivedfrom the original on 8 September 2017.
- ISBN 978-0-7637-2879-3. Archivedfrom the original on 8 September 2017.
- ^ "Willy Burgdorfer – obituary". Daily Telegraph. 1 December 2014. Archived from the original on 1 December 2014. Retrieved 1 December 2014.
- S2CID 36141950.
- PMID 25999227.
- ^ a b "Lyme disease vaccine". Centers for Disease Control and Prevention. 11 August 2022. Retrieved 7 June 2023.
- ^ from the original on 27 September 2013.
- ^ a b c "Lyme disease rashes and look-alikes". Lyme Disease. Centers for Disease Control and Prevention. 21 December 2018. Archived from the original on 2 April 2019. Retrieved 18 April 2019.
- ^ a b c "Lyme disease: erythema migrans". Lyme disease NICE guideline [NG95]. National Institute for Health and Care Excellence. Archived from the original on 9 May 2019. Retrieved 8 May 2019.
- PMID 38407256.
- ^ PMID 17579230.
- PMID 30216021.
- ^ a b Lyme disease at eMedicine
- ^ PMID 17029130.
- ^ "Lyme Disease". The Lecturio Medical Concept Library. Retrieved 9 July 2021.
- PMID 12905137. (primary source)
- ^ PMID 23319969.
- ^ S2CID 10590435.
- ^ (PDF) from the original on 8 August 2017. Retrieved 30 April 2019.
- ^ PMID 6516450.
- S2CID 35345898.
- ^ PMID 27161773.
- ^ PMID 29110887.
- ^ PMID 21127770.
- ^ (PDF) from the original on 29 August 2017. Retrieved 9 May 2019.
- ^ S2CID 31461047.
- ^ PMID 18452805.
- S2CID 245705028.
- PMID 18452802.
- ^ PMID 27914746.
- PMID 18452688.
- S2CID 20746489.
- PMID 10665700.
- ^ PMID 33417672.
- PMID 15358567.
- PMID 31214329.
- ISBN 978-1-913652-61-6.
- PMID 27523487.
- PMID 21414082.
- from the original on 29 January 2020. Retrieved 29 January 2020.
- PMID 18650352.
- ^ "UpToDate". www.uptodate.com. Retrieved 10 July 2021.
- ^ PMID 18452798.
- ^ ISBN 978-0-8385-8529-0.
- ^ Smith-Fiola D, Hamilton GC (March 2005). "2005 Fact Sheet, Prevent Tick Bites: Prevent Lyme Disease" (PDF). Rutgers University, Rutgers Cooperative Research & Extension, New Jersey Agricultural Experiment Station. Archived from the original (PDF) on 26 June 2013.
- ^ Scribner H (31 May 2019). "People are freaking out over the CDC's photo of a muffin with ticks in it". Deseret News. Utah. Archived from the original on 25 January 2020.
The U.S. CDC published a picture of a poppy seed muffin in which some of the "poppy seeds" were actually ticks
- ^ PMID 15117014.
- ^ "Westport Weston Health District". 2004. Archived from the original on 29 September 2013. Retrieved 26 September 2013.
- ^ a b "Lyme Disease Data and surveillance". Lyme Disease. Centers for Disease Control and Prevention. 5 February 2019. Archived from the original on 13 April 2019. Retrieved 12 April 2019.
- (PDF) from the original on 16 February 2019. Retrieved 9 September 2019.
- ^ PMID 15085185.
- ^ Hu L (13 May 2019). "Patient education: What to do after a tick bite to prevent Lyme disease (Beyond the Basics)". www.uptodate.com. UpToDate. Archived from the original on 1 January 2020. Retrieved 30 January 2020.
- ^ PMID 16820453.
- ^ PMID 17417956.
- S2CID 42617030.
- S2CID 18882042.
- PMID 17326941.
- ^ S2CID 24200639.
- PMID 9169184.
- S2CID 19214181.
- S2CID 270178.
- PMID 18452807.
- PMID 15528699.
- PMID 15709249.
- S2CID 31929160.
- S2CID 26801402.
- PMID 19926325.
- PMID 2668764.
- ^ a b c "CDC Lyme disease FAQ". Centers for Disease Control and Prevention. 8 January 2021. Retrieved 11 January 2023.
- PMID 17041141.
- S2CID 336323.
- S2CID 11600373.
- ^ "Does Borrelia burgdorferi produce a neurotoxin ?". American Lyme Disease Foundation. Retrieved 30 July 2022.
- S2CID 24311718.
- PMID 37814488.
- PMID 16698304.
- PMID 17404293.
- S2CID 18750257.
- PMID 11450660.
- from the original on 3 April 2015.
- from the original on 7 July 2019. Retrieved 5 July 2019.
- PMID 19076824.
- PMID 15214872.
- S2CID 16089636.
- PMID 15695691.
- PMID 12118171.
- S2CID 43045224.
- PMID 10404913.
- S2CID 19701481.
- PMID 16142659.
- ^ a b "Lyme Disease risk areas map". Risk of Lyme disease to Canadians. Government of Canada. 27 January 2015. Archived from the original on 10 May 2019. Retrieved 8 May 2019.
- ^ PMID 19486523.
- ^ "Lyme disease diagnosis". Centers for Disease Control and Prevention (CDC). 7 October 2008. Archived from the original on 28 August 2009. Retrieved 6 July 2009.
- ^ a b "Lyme disease". NICE guideline [NG95]. National Institute for Health and Care Excellence. 11 April 2018. Archived from the original on 11 May 2019. Retrieved 24 May 2019.
- S2CID 30818459.
- ^ PMID 16050454.
- ^ "Are serological tests of any value in the diagnosis of Lyme disease?". American Lyme Disease Foundation. Archived from the original on 19 December 2019. Retrieved 2 December 2019.
- S2CID 23797801.
- ^ PMID 17522387.
- PMID 11438915.
- ^ PMID 16020686.
- PMID 8272083.
- PMID 2913036.
- PMID 24449537.
- PMID 24449537.
- S2CID 245118295.
- PMID 19346313.
- S2CID 2807397.
- S2CID 10894629.
- PMID 26028977.
- ^ S2CID 15518713. Archived from the original(PDF) on 20 February 2019.
- S2CID 3862308.
- PMID 21865190.
- ^ a b c d e f g h i j "Preventing tick bites on people". Lyme Disease. Centers for Disease Control and Prevention. 8 March 2019. Archived from the original on 15 June 2019. Retrieved 21 May 2019.
- ^ a b "About ticks – preventative measures". Tick-borne diseases. Companion Vector-Borne Diseases. Archived from the original on 7 June 2019. Retrieved 21 May 2019.
- ^ PMID 27330093.
- ^ "Host seeking". CVBD: Companion Vector-Borne Diseases. Archived from the original on 16 October 2016. Retrieved 8 December 2016.
- ^ a b c "Tips to prevent tick bytes". Insect repellents. Environmental Protection Agency. 15 July 2013. Archived from the original on 15 April 2019. Retrieved 21 May 2019.
- ^ a b c d e f g h "Protection against Mosquitoes, Ticks, & Other Arthropods". Travelers' Health. Centers for Disease Control and Prevention. Archived from the original on 9 May 2019. Retrieved 21 May 2019.
- ^ PMID 21485369.
- ^ PMID 28754599.
- PMID 18498556.
- ^ a b "Repellents: protection against mosquitoes, ticks and other arthropods". Insect repellents. Environmental Protection Agency. 9 July 2013. Archived from the original on 20 May 2019. Retrieved 21 May 2019.
- ^ S2CID 53246686.
- ^ a b c d e Stafford KC (2007). "Tick management handbook (rev. ed.)" (PDF). Bulletins. Connecticut Agricultural Experiment Station. Archived (PDF) from the original on 3 April 2019. Retrieved 21 May 2019.
- S2CID 39805040.
- ^ a b c d e f "Tick removal and testing". Lyme Disease. Centers for Disease Control and Prevention. 22 April 2019. Archived from the original on 23 November 2017. Retrieved 21 May 2019.
- ^ a b "Tick Allergy". 2014. Archived from the original on 14 May 2015. Retrieved 30 April 2015.
- PMID 12092975.
- PMID 20832708.
- ^ a b c d e "Preventing tick bites in the yard". Lyme Disease. Centers for Disease Control and Prevention. 8 March 2019. Archived from the original on 15 June 2019. Retrieved 21 May 2019.
- ^ "CDC – Lyme Disease – NIOSH Workplace Safety and Health Topic". www.cdc.gov. 3 August 2017. Archived from the original on 13 November 2015. Retrieved 3 November 2015.
- ^ "Risks: Lyme Disease | NIOSH | CDC". www.cdc.gov. 14 November 2018. Archived from the original on 26 April 2019. Retrieved 26 April 2019.
- ^ "Lyme disease". The Centers for Disease Control and Prevention. 12 October 2016. Archived from the original on 17 June 2017. Retrieved 22 June 2017.
 This article incorporates public domain material from websites or documents of the Centers for Disease Control and Prevention.
This article incorporates public domain material from websites or documents of the Centers for Disease Control and Prevention.
- ^ . Retrieved 4 March 2022.
- S2CID 5853201.
- ^ "Figure 2: Changes in deer density and cases of Lyme disease in Mumford Cove, Connecticut, 1996–2004 (CT DEP data)" (PDF). Managing Urban Deer in Connecticut (2nd ed.). Connecticut Department of Environmental Protection – Wildlife Division. June 2007. p. 4. Archived (PDF) from the original on 2 June 2013.
- ^ Stafford KC (2004). Tick Management Handbook (PDF). Connecticut Agricultural Experiment Station and Connecticut Department of Public Health. p. 46. Archived (PDF) from the original on 25 October 2007. Retrieved 21 August 2007.
- PMID 32478654.
- PMID 17048307.
- ^ PMID 9580423.
- ^ PMID 24352572.
- PMID 1404260.
- PMID 7815401.
- PMID 23571115.[permanent dead link]
- ^ PMID 33289681.
- PMID 11257352.
- ^ PMID 21217172.
- ^ Rowe C (13 June 1999). "Lukewarm Response To New Lyme Vaccine". The New York Times. Archived from the original on 10 February 2012. Retrieved 11 July 2008.
- ^ S2CID 4315588.
- ^ "Sole Lyme Vaccine Is Pulled Off Market". The New York Times. 28 February 2002. Archived from the original on 30 August 2010. Retrieved 11 July 2008.
- ^ PMID 16893489.
- PMID 16452935.
- PMID 22709388.
- ^ "Anti-vaxxers stopped the last Lyme disease vaccine. The FDA has just fast-tracked a new one". Newsweek. 25 July 2017. Archived from the original on 25 December 2017. Retrieved 25 December 2017.
- ^ Brooks D (6 August 2018). "A Lyme vaccine for humans is getting closer, says French biotech firm". Concord Monitor. Retrieved 20 July 2021.
- ^ Taylor NP (4 February 2022). "Pfizer's $130M Lyme disease vaccine advances to phase 3 after 3rd shot shown to increase antibodies". Fierce Biotech. Retrieved 5 June 2022.
- ^ Neergaard L, Lum S (8 August 2022). "Major test of first possible Lyme vaccine in 20 years begins". Associated Press. Retrieved 11 August 2022.
- ^ a b "An Efficacy, Safety, Tolerability, Immunogenicity, and Lot-Consistency Clinical Trial of a 6-Valent OspA-Based Lyme Disease Vaccine (VLA15) (VALOR)". ClinicalTrials.gov. National Institute of Health. 28 July 2022. Retrieved 11 August 2022.
- ^ Klein A (17 November 2021). "An mRNA vaccine that causes a red, itchy skin rash in response to bites by ticks may allow them to be removed before they transmit Lyme disease-causing bacteria". New Scientist.
- ^ Hathaway B. "Novel Lyme vaccine shows promise". Yale University. Retrieved 13 December 2021.
Compared to non-immunized guinea pigs, vaccinated animals exposed to infected ticks quickly developed redness at the tick bite site. None of the immunized animals developed Lyme disease if ticks were removed when redness developed. In contrast, about half of the control group became infected with B. burgdorferi after tick removal. When a single infected tick was attached to immunized guinea pigs and not removed, none of vaccinated animals were infected compared to 60 percent of control animals. However, protection waned in immunized guinea pigs if three ticks remained attached to the animal. Ticks in immunized animals were unable to feed aggressively and dislodged more quickly than those on guinea pigs in the control group.
- S2CID 244375227.
- ^ a b Brooks WC. "Lyme Disease". Veterinary Information Network. Archived from the original on 4 April 2015. Retrieved 10 February 2012.
- PMID 32352736.
- PMID 27028911.
- ^ Stephenson M (4 October 2012). "OTC Drops: Telling the Tears Apart". Review of Ophtalmology. Jobson Medical Information LLC. Archived from the original on 17 April 2019. Retrieved 16 April 2019.
- ^ PMID 25999223.
- ^ S2CID 3083800.
- PMID 22523260.
- ^ PMID 9233865.
- S2CID 42290158.
- S2CID 28306612.
- ^ S2CID 85021.
- ^ PMID 10194080.
- PMID 11133377.
- ^ S2CID 25596860.
- PMID 23150958.
- PMID 37711861.
- ^ a b c "Post-Treatment Lyme Disease Syndrome". CDC. 3 November 2016. Archived from the original on 17 June 2017.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ "Post-treatment Lyme Disease as a Model for Persistent Symptoms in Lyme Disease", Frontiers in Medicine (Lausanne), Alison W Rebman, John N Aucott, PMCID: PMC7052487, Feb. 25, 2020.
- PMID 15702720.
- ISBN 978-1-4988-0343-4. Archivedfrom the original on 8 September 2017.
- S2CID 231300522.
- PMID 16929760.
- (PDF) from the original on 19 July 2018. Retrieved 5 July 2019.
- PMID 10946521.
- PMID 2699499.
- PMID 16119758.
- ^ "Case of the Month". Federation of Infectious Diseases Societies of Southern Africa (FIDSSA). December 2015. Retrieved 2 November 2023.
- PMID 9647853.
- from the original on 22 January 2013.
- PMID 16524782.
- PMID 30746341.
- PMID 35502617.
- PMID 36365042.
- from the original on 9 July 2011.
- PMID 16819127.
- from the original on 17 June 2012.
- S2CID 208170787.
- S2CID 73424569.
- ^ a b c d "Epidemiology of Lyme borreliosis in the UK". HPA. Archived from the original on 10 June 2013. Retrieved 15 December 2012.
- S2CID 25295954.
- ^ a b "Lyme Disease". Parliamentary Debates (Hansard). 11 November 1991. Archived from the original on 15 June 2013.
- ^ a b "Tick Lyme disease off your holiday list" (Press release). Health Protection Agency. 14 April 2011. Archived from the original on 28 April 2011. Retrieved 29 March 2013.
- ^ "Concern about rise in Lyme disease cases". Lyme Disease Action. 15 December 2011. Archived from the original on 19 June 2013. Retrieved 15 December 2012.
- ^ Cassidy F (14 March 2011). "Tayside revealed as a Lyme disease hotspot as cases soar". Press and Journal. Archived from the original on 11 March 2016.
- ^ "Lyme disease: A clear and present danger". RCN. 28 April 2009. Archived from the original on 29 March 2013. Retrieved 15 December 2012.
- ^ "Guidance on Part 2 – Notifiable Diseases, Notifiable Organisms and Health Risk States". Scotland.gov.uk. 10 September 2012. Retrieved 15 December 2012.
- ^ "Lyme Disease". Parliamentary Debates (Hansard). 3 February 1997. Archived from the original on 15 June 2013.
- ^ Fox W (2010). "Tick-Borne Disease, Risk and Realit" (PDF). BADA-UK. Archived from the original (PDF) on 20 November 2012.
- ^ "Lyme borreliosis epidemiology and surveillance: May 2013". HPA. Archived from the original on 25 November 2015. Retrieved 24 November 2015.
- ^ "Zoonoses report UK 2009" (PDF). DEFRA. 24 January 2011. Archived (PDF) from the original on 3 November 2012.
- ^ "Overview Tick Bite Prevention Week". Archived from the original on 10 April 2012.
- PMID 8037992.
- S2CID 39557628.
- (Press release). University of Bristol. 25 January 2012.
- ^ Roberts M (24 January 2012). "Lyme disease risk from dogs 'higher than thought'". BBC News. Archived from the original on 31 January 2012.
- ^ "The London climate change adaptation strategy - Draft report" (PDF). Greater London Authority. August 2008. Archived from the original (PDF) on 17 August 2012.
- PMID 19008966.
- ^ (PDF) from the original on 8 September 2015.
- ^ BC Ministry of Agriculture. "Ticks and Humans in British Columbia". Agf.gov.bc.ca. Archived from the original on 3 January 2013. Retrieved 15 December 2012.
- ^ "Lyme Disease Fact Sheet". Phac-aspc.gc.ca. 4 July 2012. Archived from the original on 27 December 2012. Retrieved 15 December 2012.
- PMID 19506281.
- S2CID 16921155.
- PMID 18258006.
- ^ CDC (4 January 2012). "Reported Lyme disease cases by state, 2000-2010". Centers for Disease Control and Prevention (CDC). Archived from the original on 4 May 2012. Retrieved 29 April 2012.
- from the original on 19 November 2012.
- from the original on 10 November 2012.
- ^ "Lyme Disease Data". Centers for Disease Control and Prevention (CDC). Archived from the original on 30 April 2012.
- ^ a b Robbins J (20 May 2003). "Montana Lab Tries to Identify Tick-Borne Disease". The New York Times. Archived from the original on 3 September 2017.
- ^ "National Notifiable Diseases Surveillance System (NNDSS) - Lyme Disease". Centers for Disease Control and Prevention. 7 September 2021. Retrieved 11 January 2023.
- ^ "Lyme Disease (Borrelia burgdorferi) 2022 Case Definition". Centers for Disease Control and Prevention. 12 August 2022. Retrieved 11 January 2023.
- ^ "Lyme disease surveillance and available data". Centers for Disease Control and Prevention. 15 November 2022. Retrieved 11 January 2023.
- ^ "STARI or Lyme?". Centers for Disease Control and Prevention. 19 November 2018. Archived from the original on 12 November 2019.
- PMID 17401487.
- PMID 8284588.
- ISBN 978-0-312-14068-7.
- . YaleNews. 10 August 2009.
- ^ Josselyn J (1670). An Account of Two Voyages to New-England Made during the Years 1638, 1663. Archived from the original on 25 June 2013.page 92
- ^ ISBN 978-0-615-20061-3.
- S2CID 70661702.
- National Geographic. Archived from the originalon 19 October 2011. Retrieved 17 October 2011.
- ^ S2CID 46704791.
- ^ Burckhardt JL (1911). "Zur Frage der Follikel- und Keimzentrenbildung in der Haut". Frankf. Z. Pathol. (in German). 6: 352–59.
- ISBN 978-0-300-09867-9. page 191.
- ^ Hellerström S (1930). "Erythema chronicum migrans Afzelii". Acta Derm. Venerol. (in German). 11: 315–21.
- PMID 18891989.
- PMID 18140373.
- PMID 15421023.
- PMID 13190934.
- PMID 5497158.
- PMID 25451629.
- ^ Weir W (19 September 2013). "Lyme Disease Pioneer Stephen Malawista Dies". Hartford Courant. Archived from the original on 14 October 2013. Retrieved 14 October 2013.
- PMID 8933327.
- ISBN 978-1-4160-2999-1.[page needed]
- PMID 989847.
- S2CID 43397837.
- ^ "Factsheet about Borreliosis". European Centre for Disease Prevention and Control. 17 June 2017. Archived from the original on 27 September 2019. Retrieved 30 January 2020.
- ^ "WHO | Lyme Borreliosis (Lyme disease)". WHO. Archived from the original on 29 November 2019. Retrieved 30 January 2020.
- PMID 6407378.
- PMID 6516454.
- from the original on 30 January 2020. Retrieved 4 September 2018.
- S2CID 25939418.
- S2CID 7314488.
- PMID 3585913.
- ^ PMID 12525705.
- PMID 15238283.
- PMID 16216650.
- S2CID 13746169.
- S2CID 35285261.
- ^ ""Chronic Lyme Disease" Fact Sheet". National Institute of Allergy and Infectious Diseases. 17 April 2009. Archived from the original on 15 December 2012.
- PMID 18452806.
- ^ MacBeth B (8 April 2019). "A Review of Under Our Skin, A Cult Classic". Science-Based Medicine. Retrieved 10 September 2021.
- ^ PMID 20207198.
- ^ PMID 20933139.
- ^ Hahn J. "Ticks and Their Control". Regents of the University of Minnesota. Archived from the original on 25 February 2012. Retrieved 19 February 2012.
- ^ "Glomerular Disease". The Merck Veterinary Manual. Archived from the original on 26 June 2017. Retrieved 19 May 2017.
- ^ Staubinger R (31 May 2000). "Lyme Disease". Sirius Dog. Archived from the original on 23 June 2012. Retrieved 10 February 2012.
- ^ Fatal cases of Lyme disease reported in the medical literature include:
- Kirsch M, Ruben FL, Steere AC, Duray PH, Norden CW, Winkelstein A (May 1988). "Fatal adult respiratory distress syndrome in a patient with Lyme disease". JAMA. 259 (18): 2737–2739. PMID 3357244.
- Oksi J, Kalimo H, Marttila RJ, Marjamäki M, Sonninen P, Nikoskelainen J, et al. (December 1996). "Inflammatory brain changes in Lyme borreliosis. A report on three patients and review of literature". Brain. 119 (Pt 6): 2143–2154. PMID 9010017.
- Waniek C, Prohovnik I, Kaufman MA, Dwork AJ (1995). "Rapidly progressive frontal-type dementia associated with Lyme disease". The Journal of Neuropsychiatry and Clinical Neurosciences. 7 (3): 345–347. PMID 7580195.
- Cary NR, Fox B, Wright DJ, Cutler SJ, Shapiro LM, Grace AA (February 1990). "Fatal Lyme carditis and endodermal heterotopia of the atrioventricular node". Postgraduate Medical Journal. 66 (772): 134–136. PMID 2349186.
- Kirsch M, Ruben FL, Steere AC, Duray PH, Norden CW, Winkelstein A (May 1988). "Fatal adult respiratory distress syndrome in a patient with Lyme disease". JAMA. 259 (18): 2737–2739.
- ^ a b c "Lyme Disease (Lyme Borreliosis) in Cats - Cat Owners". Merck Veterinary Manual. Retrieved 26 October 2023.
- ^ PMID 31949917.
- PMID 29469222.
- PMID 37370494.
![]() This article incorporates public domain material from Post-Treatment Lyme Disease Syndrome. Centers for Disease Control and Prevention.
This article incorporates public domain material from Post-Treatment Lyme Disease Syndrome. Centers for Disease Control and Prevention.
Further reading
- Ostfeld R (2012). Lyme Disease: The Ecology of a Complex System. New York: ISBN 978-0-19-992847-7.
- Barbour AG (2015). Lyme disease: why it's spreading, how it makes you sick, and what to do about it. Baltimore: Johns Hopkins University Press. ISBN 978-1-4214-1721-9.
- Halperin JJ, ed. (2018). Lyme disease: an evidence-based approach (2nd ed.). Wallingford, Oxfordshire, UK: CABI. ISBN 978-1-78639-207-7.
- Radolf JD, Samuels DS, eds. (2021). Lyme disease and relapsing fever spirochetes: genomics, molecular biology, host interactions and disease pathogenesis. Poole, UK: Caister. ISBN 978-1-913652-61-6.
- Oaklander M (17 June 2021). "We Used to Have a Lyme Disease Vaccine. Are We Ready to Bring One Back?". Time.
External links
- CDC - Lyme Disease
- Association for Public Health Laboratories guide – Suggested Reporting Language, Interpretation and Guidance Regarding Lyme Disease Serologic Test Results
- NIH – Lyme Disease
- NICE Guidelines – Lyme Disease

![20% of Lyme rashes in the United States show a "bull's eye" or "target-like" appearance.[27][28][29]](http://upload.wikimedia.org/wikipedia/commons/thumb/0/01/Erythema_migrans_-_erythematous_rash_in_Lyme_disease_-_PHIL_9875.jpg/150px-Erythema_migrans_-_erythematous_rash_in_Lyme_disease_-_PHIL_9875.jpg)
![Erythema migrans ("redness migrating") on a woman's neck.[30] Rashes from non-Lyme causes may look similar.[31][32]](http://upload.wikimedia.org/wikipedia/commons/thumb/0/03/Solid_erythema_migrans_rash_on_the_neck_of_a_woman_with_Lyme_disease.jpg/150px-Solid_erythema_migrans_rash_on_the_neck_of_a_woman_with_Lyme_disease.jpg)