Macula densa
This article needs additional citations for verification. (May 2015) |
| Macula densa | |
|---|---|
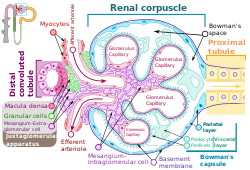 Renal corpuscle showing the macula densa. | |
| Identifiers | |
| FMA | 86333 |
| Anatomical terminology | |
In the
The cells of the macula densa are sensitive to the concentration of sodium chloride in the thick ascending loop of henle. A decrease in sodium chloride concentration initiates a signal from the macula densa that has two effects: (1) it decreases resistance to blood flow in the afferent arterioles, which raises
As such, an increase in sodium chloride concentration would result in vasoconstriction of afferent arterioles, and reduced paracrine stimulation of juxtaglomerular cells. This demonstrates the macula densa feedback, where compensatory mechanisms act in order to return GFR to normal.
The release of renin is an essential component of the
Histology
The cells of the macula densa are taller and have more prominent nuclei than surrounding cells of the distal straight tubule (cortical thick ascending limb).
The close proximity and prominence of the nuclei cause this segment of the distal tubule wall to appear darker in microscopic preparations,[5] hence the name macula densa.
Function

Macula densa cells sense changes in sodium chloride level, and will trigger an autoregulatory response to increase or decrease reabsorption of ions and water to the blood (as needed) in order to alter blood volume and return blood pressure to normal.
A decrease in afferent arteriole diameter causes a decrease in the GFR (glomerular filtration rate), resulting in a decreased concentration of sodium and chloride ions in the filtrate and/or decreased filtrate flow rate. Reduced blood pressure means decreased venous pressure and, hence, a decreased
Hence, a decrease in blood pressure results in less sodium chloride present at the
Thus, a drop in blood pressure results in preferential vasodilation of the
The process triggered by the macula densa helps keep the GFR fairly steady in response to varying artery pressure.
Damage to the macula densa would impact blood flow to the kidneys because the afferent arterioles would not dilate in response to a decrease in filtrate osmolarity and pressure at the glomerulus would not be increased. As part of the body's blood pressure regulation, the macula densa monitors filtrate osmolarity; if it falls too far, the macula densa causes the efferent arterioles of the kidney to contract, thus increasing the pressure at the glomerulus and increasing the glomerular filtration rate.
See also
References
- PMID 30354966.
- ^ "Tubuloglomerular Feedback - an overview | ScienceDirect Topics".
- PMID 25318757.
- ^ Guyton & Hall Textbook Of Physiology, 11th Edition 2006, p. 324
- ISBN 978-0195151732.
- PMID 20360309.
External links
- Anatomy photo: Urinary/mammal/cortex1/cortex5 - Comparative Organology at University of California, Davis - "Mammal, kidney cortex (LM, Medium)"
- Nosek, Thomas M. "Section 7/7ch03/7ch03p17". Essentials of Human Physiology. Archived from the original on 2016-03-24. - "The Nephron: Juxtaglomerular Apparatus"
