Magnetic resonance imaging
| Magnetic resonance imaging | |
|---|---|
Para-sagittal MRI of the head, with aliasing artifacts (nose and forehead appear at the back of the head) | |
| Synonyms | Nuclear magnetic resonance imaging (NMRI), magnetic resonance tomography (MRT) |
| ICD-9-CM | 88.91 |
| MeSH | D008279 |
| MedlinePlus | 003335 |
Magnetic resonance imaging (MRI) is a
MRI is widely used in hospitals and clinics for medical diagnosis, staging and follow-up of disease. Compared to CT, MRI provides better contrast in images of soft tissues, e.g. in the brain or abdomen. However, it may be perceived as less comfortable by patients, due to the usually longer and louder measurements with the subject in a long, confining tube, although "open" MRI designs mostly relieve this. Additionally, implants and other non-removable metal in the body can pose a risk and may exclude some patients from undergoing an MRI examination safely.
MRI was originally called NMRI (nuclear magnetic resonance imaging), but "nuclear" was dropped to avoid negative associations.[2] Certain atomic nuclei are able to absorb radio frequency (RF) energy when placed in an external magnetic field; the resultant evolving spin polarization can induce a RF signal in a radio frequency coil and thereby be detected.[3] In clinical and research MRI, hydrogen atoms are most often used to generate a macroscopic polarization that is detected by antennas close to the subject being examined.[3] Hydrogen atoms are naturally abundant in humans and other biological organisms, particularly in water and fat. For this reason, most MRI scans essentially map the location of water and fat in the body. Pulses of radio waves excite the nuclear spin energy transition, and magnetic field gradients localize the polarization in space. By varying the parameters of the pulse sequence, different contrasts may be generated between tissues based on the relaxation properties of the hydrogen atoms therein.
Since its development in the 1970s and 1980s, MRI has proven to be a versatile imaging technique. While MRI is most prominently used in diagnostic medicine and biomedical research, it also may be used to form images of non-living objects, such as mummies. Diffusion MRI and functional MRI extend the utility of MRI to capture neuronal tracts and blood flow respectively in the nervous system, in addition to detailed spatial images. The sustained increase in demand for MRI within health systems has led to concerns about cost effectiveness and overdiagnosis.[4][5][dubious ]
Mechanism
Construction and physics

In most medical applications, hydrogen nuclei, which consist solely of a proton, that are in tissues create a signal that is processed to form an image of the body in terms of the density of those nuclei in a specific region. Given that the protons are affected by fields from other atoms to which they are bonded, it is possible to separate responses from hydrogen in specific compounds. To perform a study, the person is positioned within an MRI scanner that forms a strong magnetic field around the area to be imaged. First, energy from an oscillating magnetic field is temporarily applied to the patient at the appropriate resonance frequency. Scanning with X and Y gradient coils causes a selected region of the patient to experience the exact magnetic field required for the energy to be absorbed. The atoms are excited by a RF pulse and the resultant signal is measured by a receiving coil. The RF signal may be processed to deduce position information by looking at the changes in RF level and phase caused by varying the local magnetic field using gradient coils. As these coils are rapidly switched during the excitation and response to perform a moving line scan, they create the characteristic repetitive noise of an MRI scan as the windings move slightly due to magnetostriction. The contrast between different tissues is determined by the rate at which excited atoms return to the equilibrium state. Exogenous contrast agents may be given to the person to make the image clearer.[6]
The major components of an MRI scanner are the main magnet, which polarizes the sample, the shim coils for correcting shifts in the homogeneity of the main magnetic field, the gradient system which is used to localize the region to be scanned and the RF system, which excites the sample and detects the resulting NMR signal. The whole system is controlled by one or more computers.

MRI requires a magnetic field that is both strong and uniform to a few parts per million across the scan volume. The field strength of the magnet is measured in teslas – and while the majority of systems operate at 1.5 T, commercial systems are available between 0.2 and 7 T. Whole-body MRI systems for research applications operate in e.g. 9.4T,[7][8] 10.5T,[9] 11.7T.[10] Even higher field whole-body MRI systems e.g. 14 T and beyond are in conceptual proposal[11] or in engineering design.[12] Most clinical magnets are superconducting magnets, which require liquid helium to keep them at low temperatures. Lower field strengths can be achieved with permanent magnets, which are often used in "open" MRI scanners for claustrophobic patients.[13] Lower field strengths are also used in a portable MRI scanner approved by the FDA in 2020.[14] Recently, MRI has been demonstrated also at ultra-low fields, i.e., in the microtesla-to-millitesla range, where sufficient signal quality is made possible by prepolarization (on the order of 10–100 mT) and by measuring the Larmor precession fields at about 100 microtesla with highly sensitive superconducting quantum interference devices (SQUIDs).[15][16][17]
T1 and T2
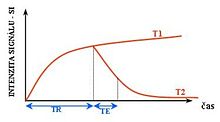
Each tissue returns to its equilibrium state after excitation by the independent relaxation processes of T1 (
The information from MRI scans comes in the form of image contrasts based on differences in the rate of relaxation of nuclear spins following their perturbation by an oscillating magnetic field (in the form of radiofrequency pulses through the sample).[18] The relaxation rates are a measure of the time it takes for a signal to decay back to an equilibrium state from either the longitudinal or transverse plane.
Magnetization builds up along the z-axis in the presence of a magnetic field, B0, such that the magnetic dipoles in the sample will, on average, align with the z-axis summing to a total magnetization Mz. This magnetization along z is defined as the equilibrium magnetization; magnetization is defined as the sum of all magnetic dipoles in a sample. Following the equilibrium magnetization, a 90° radiofrequency (RF) pulse flips the direction of the magnetization vector in the xy-plane, and is then switched off. The initial magnetic field B0, however, is still applied. Thus, the spin magnetization vector will slowly return from the xy-plane back to the equilibrium state. The time it takes for the magnetization vector to return to its equilibrium value, Mz, is referred to as the longitudinal relaxation time, T1.[19] Subsequently, the rate at which this happens is simply the reciprocal of the relaxation time: . Similarly, the time in which it takes for Mxy to return to zero is T2, with the rate .[20] Magnetization as a function of time is defined by the Bloch equations.

T1 and T2 values are dependent on the chemical environment of the sample; hence their utility in MRI. Soft tissue and muscle tissue relax at different rates, yielding the image contrast in a typical scan.
The standard display of MR images is to represent fluid characteristics in black-and-white images, where different tissues turn out as follows:
| Signal | T1-weighted | T2-weighted |
|---|---|---|
| High |
|
|
| Intermediate | Gray matter darker than white matter[23]
|
White matter darker than grey matter[23] |
| Low |
Diagnostics
Usage by organ or system

MRI has a wide range of applications in medical diagnosis and more than 25,000 scanners are estimated to be in use worldwide.[24] MRI affects diagnosis and treatment in many specialties although the effect on improved health outcomes is disputed in certain cases.[25][26]

MRI is the investigation of choice in the preoperative staging of rectal and prostate cancer and has a role in the diagnosis, staging, and follow-up of other tumors,[27] as well as for determining areas of tissue for sampling in biobanking.[28][29]
Neuroimaging

MRI is the investigative tool of choice for neurological cancers over CT, as it offers better visualization of the
The record for the highest spatial resolution of a whole intact brain (postmortem) is 100 microns, from Massachusetts General Hospital. The data was published in NATURE on 30 October 2019.[38][39]
Cardiovascular
Cardiac MRI is complementary to other imaging techniques, such as
Musculoskeletal
Applications in the musculoskeletal system include spinal imaging, assessment of joint disease, and soft tissue tumors.[42] Also, MRI techniques can be used for diagnostic imaging of systemic muscle diseases including genetic muscle diseases.[43][44]
Swallowing movement of throat and oesophagus can cause motion artifact over the imaged spine. Therefore, a saturation pulse[clarification needed] applied over this region the throat and oesophagus can help to avoid this artifact. Motion artifact arising due to pumping of the heart can be reduced by timing the MRI pulse according to heart cycles.[45] Blood vessels flow artifacts can be reduced by applying saturation pulses above and below the region of interest.[46]
Liver and gastrointestinal
Angiography
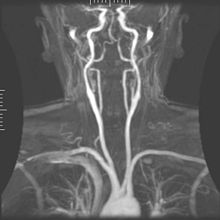
Magnetic resonance
Techniques involving phase accumulation (known as phase contrast angiography) can also be used to generate flow velocity maps easily and accurately. Magnetic resonance venography (MRV) is a similar procedure that is used to image veins. In this method, the tissue is now excited inferiorly, while the signal is gathered in the plane immediately superior to the excitation plane—thus imaging the venous blood that recently moved from the excited plane.[52]
Contrast agents
MRI for imaging anatomical structures or blood flow do not require contrast agents since the varying properties of the tissues or blood provide natural contrasts. However, for more specific types of imaging,
Gadolinium-based contrast reagents are typically
In December 2017, the Food and Drug Administration (FDA) in the United States announced in a drug safety communication that new warnings were to be included on all gadolinium-based contrast agents (GBCAs). The FDA also called for increased patient education and requiring gadolinium contrast vendors to conduct additional animal and clinical studies to assess the safety of these agents.[57] Although gadolinium agents have proved useful for patients with kidney impairment, in patients with severe kidney failure requiring dialysis there is a risk of a rare but serious illness, nephrogenic systemic fibrosis, which may be linked to the use of certain gadolinium-containing agents. The most frequently linked is gadodiamide, but other agents have been linked too.[58] Although a causal link has not been definitively established, current guidelines in the United States are that dialysis patients should only receive gadolinium agents where essential and that dialysis should be performed as soon as possible after the scan to remove the agent from the body promptly.[59][60]
In Europe, where more gadolinium-containing agents are available, a classification of agents according to potential risks has been released.[61][62] In 2008, a new contrast agent named gadoxetate, brand name Eovist (US) or Primovist (EU), was approved for diagnostic use: This has the theoretical benefit of a dual excretion path.[63]
Sequences
An
Overview table
This table does not include
| Group | Sequence | Abbr. | Physics | Main clinical distinctions | Example |
|---|---|---|---|---|---|
| Spin echo | T1 weighted | T1 | Measuring echo time (TE).
|
Standard foundation and comparison for other sequences |

|
| T2 weighted | T2 | Measuring spin–spin relaxation by using long TR and TE times |
Standard foundation and comparison for other sequences |

| |
Proton density weighted |
PD | Long TE (to minimize T2).[68]
|
Joint disease and injury.[69]
|

| |
| Gradient echo (GRE) | Steady-state free precession | SSFP | Maintenance of a steady, residual transverse magnetisation over successive cycles.[71] | Creation of cardiac MRI videos (pictured).[71] | 
|
| Effective T2 or "T2-star" |
T2* | Spoiled gradient recalled echo (GRE) with a long echo time and small flip angle[72] | Low signal from hemosiderin deposits (pictured) and hemorrhages.[72] | 
| |
| Susceptibility-weighted | SWI | Spoiled gradient recalled echo (GRE), fully flow compensated, long echo time, combines phase image with magnitude image[73] | Detecting small amounts of hemorrhage (diffuse axonal injury pictured) or calcium.[73] | 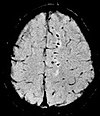
| |
| Inversion recovery | Short tau inversion recovery | STIR | Fat suppression by setting an inversion time where the signal of fat is zero.[74]
|
High signal in edema, such as in more severe stress fracture.[75] Shin splints pictured: | 
|
| Fluid-attenuated inversion recovery | FLAIR | Fluid suppression by setting an inversion time that nulls fluids | High signal in lacunar infarction, multiple sclerosis (MS) plaques, subarachnoid haemorrhage and meningitis (pictured).[76] | 
| |
| Double inversion recovery | DIR | Simultaneous suppression of cerebrospinal fluid and white matter by two inversion times.[77] | High signal of multiple sclerosis plaques (pictured).[77] | 
| |
Diffusion weighted (DWI) |
Conventional | DWI | Measure of Brownian motion of water molecules.[78] | High signal within minutes of cerebral infarction (pictured).[79] | 
|
Apparent diffusion coefficient |
ADC | Reduced T2 weighting by taking multiple conventional DWI images with different DWI weighting, and the change corresponds to diffusion.[80] | Low signal minutes after cerebral infarction (pictured).[81] | 
| |
| Diffusion tensor | DTI | Mainly tractography (pictured) by an overall greater Brownian motion of water molecules in the directions of nerve fibers.[82] |
|

| |
| Perfusion weighted (PWI) | Dynamic susceptibility contrast |
DSC | Measures changes over time in susceptibility-induced signal loss due to gadolinium contrast injection.[84]
|
|

|
| Arterial spin labelling | ASL | Magnetic labeling of arterial blood below the imaging slab, which subsequently enters the region of interest.[86] It does not need gadolinium contrast.[87] | |||
Dynamic contrast enhanced |
DCE | Measures changes over time in the shortening of the gadolinium contrast bolus.[88]
|
Faster Gd contrast uptake along with other features is suggestive of malignancy (pictured).[89] | 
| |
| Functional MRI (fMRI) | Blood-oxygen-level dependent imaging |
BOLD | Changes in oxygen saturation-dependent magnetism of hemoglobin reflects tissue activity.[90] | Localizing brain activity from performing an assigned task (e.g. talking, moving fingers) before surgery, also used in research of cognition.[91] | 
|
| Magnetic resonance angiography (MRA) and venography | Time-of-flight | TOF | Blood entering the imaged area is not yet magnetically saturated, giving it a much higher signal when using short echo time and flow compensation. | Detection of dissection[92]
|

|
| Phase-contrast magnetic resonance imaging | PC-MRA | Two gradients with equal magnitude, but opposite direction, are used to encode a phase shift, which is proportional to the velocity of spins.[93]
|
Detection of dissection (pictured).[92]
|
VIPR )
|
Other specialized configurations
Magnetic resonance spectroscopy
Magnetic resonance spectroscopic imaging (MRSI) combines both spectroscopic and imaging methods to produce spatially localized spectra from within the sample or patient. The spatial resolution is much lower (limited by the available SNR), but the spectra in each voxel contains information about many metabolites. Because the available signal is used to encode spatial and spectral information, MRSI requires high SNR achievable only at higher field strengths (3 T and above).[97] The high procurement and maintenance costs of MRI with extremely high field strengths[98] inhibit their popularity. However, recent compressed sensing-based software algorithms (e.g., SAMV[99]) have been proposed to achieve super-resolution without requiring such high field strengths.
Real-time MRI
Interventional MRI
The lack of harmful effects on the patient and the operator make MRI well-suited for
A specialized growing subset of interventional MRI is intraoperative MRI, in which an MRI is used in surgery. Some specialized MRI systems allow imaging concurrent with the surgical procedure. More typically, the surgical procedure is temporarily interrupted so that MRI can assess the success of the procedure or guide subsequent surgical work.[103]
Magnetic resonance guided focused ultrasound
In guided therapy,
Multinuclear imaging
Hydrogen has the most frequently imaged
Moreover, the nucleus of any atom that has a net nuclear spin and that is bonded to a hydrogen atom could potentially be imaged via heteronuclear magnetization transfer MRI that would image the high-gyromagnetic-ratio hydrogen nucleus instead of the low-gyromagnetic-ratio nucleus that is bonded to the hydrogen atom.[107] In principle, heteronuclear magnetization transfer MRI could be used to detect the presence or absence of specific chemical bonds.[108][109]
Multinuclear imaging is primarily a research technique at present. However, potential applications include functional imaging and imaging of organs poorly seen on 1H MRI (e.g., lungs and bones) or as alternative contrast agents. Inhaled hyperpolarized 3He can be used to image the distribution of air spaces within the lungs. Injectable solutions containing 13C or stabilized bubbles of hyperpolarized 129Xe have been studied as contrast agents for angiography and perfusion imaging. 31P can potentially provide information on bone density and structure, as well as functional imaging of the brain. Multinuclear imaging holds the potential to chart the distribution of lithium in the human brain, this element finding use as an important drug for those with conditions such as bipolar disorder.[110]
Molecular imaging by MRI
MRI has the advantages of having very high spatial resolution and is very adept at morphological imaging and functional imaging. MRI does have several disadvantages though. First, MRI has a sensitivity of around 10−3 mol/L to 10−5 mol/L, which, compared to other types of imaging, can be very limiting. This problem stems from the fact that the population difference between the nuclear spin states is very small at room temperature. For example, at 1.5 teslas, a typical field strength for clinical MRI, the difference between high and low energy states is approximately 9 molecules per 2 million. Improvements to increase MR sensitivity include increasing magnetic field strength and hyperpolarization via optical pumping or dynamic nuclear polarization. There are also a variety of signal amplification schemes based on chemical exchange that increase sensitivity.[111]
To achieve molecular imaging of disease biomarkers using MRI, targeted MRI contrast agents with high specificity and high relaxivity (sensitivity) are required. To date, many studies have been devoted to developing targeted-MRI contrast agents to achieve molecular imaging by MRI. Commonly, peptides, antibodies, or small ligands, and small protein domains, such as HER-2 affibodies, have been applied to achieve targeting. To enhance the sensitivity of the contrast agents, these targeting moieties are usually linked to high payload MRI contrast agents or MRI contrast agents with high relaxivities.[112] A new class of gene targeting MR contrast agents has been introduced to show gene action of unique mRNA and gene transcription factor proteins.[113][114] These new contrast agents can trace cells with unique mRNA, microRNA and virus; tissue response to inflammation in living brains.[115] The MR reports change in gene expression with positive correlation to TaqMan analysis, optical and electron microscopy.[116]
Parallel MRI
It takes time to gather MRI data using sequential applications of magnetic field gradients. Even for the most streamlined of
After a number of early suggestions for using arrays of detectors to accelerate imaging went largely unremarked in the MRI field, parallel imaging saw widespread development and application following the introduction of the SiMultaneous Acquisition of Spatial Harmonics (SMASH) technique in 1996–7.[117] The SENSitivity Encoding (SENSE)[118] and Generalized Autocalibrating Partially Parallel Acquisitions (GRAPPA)[119] techniques are the parallel imaging methods in most common use today. The advent of parallel MRI resulted in extensive research and development in image reconstruction and RF coil design, as well as in a rapid expansion of the number of receiver channels available on commercial MR systems. Parallel MRI is now used routinely for MRI examinations in a wide range of body areas and clinical or research applications.
Quantitative MRI
Most MRI focuses on qualitative interpretation of MR data by acquiring spatial maps of relative variations in signal strength which are "weighted" by certain parameters.[120] Quantitative methods instead attempt to determine spatial maps of accurate tissue relaxometry parameter values or magnetic field, or to measure the size of certain spatial features.
Examples of quantitative MRI methods are:
- T1-mapping (notably used in cardiac magnetic resonance imaging[121])
- T2-mapping[122]
- Quantitative susceptibility mapping (QSM)
- Quantitative fluid flow MRI (i.e. some cerebrospinal fluid flow MRI[123])
- Magnetic resonance elastography (MRE)[124]
Quantitative MRI aims to increase the reproducibility of MR images and interpretations, but has historically require longer scan times.[120]
Quantitative MRI (or qMRI) sometimes more specifically refers to multi-parametric quantitative MRI, the mapping of multiple tissue relaxometry parameters in a single imaging session.[125] Efforts to make multi-parametric quantitative MRI faster have produced sequences which map multiple parameters simultaneously, either by building separate encoding methods for each parameter into the sequence,[126] or by fitting MR signal evolution to a multi-parameter model.[127][128]
Hyperpolarized gas MRI
Traditional MRI generates poor images of lung tissue because there are fewer water molecules with protons that can be excited by the magnetic field. Using hyperpolarized gas an MRI scan can identify ventilation defects in the lungs. Before the scan, a patient is asked to inhale hyperpolarized xenon mixed with a buffer gas of helium or nitrogen. The resulting lung images are much higher quality than with traditional MRI.
Safety
MRI is, in general, a safe technique, although injuries may occur as a result of failed safety procedures or human error.
MRI uses powerful magnets and can therefore cause magnetic materials to move at great speeds, posing a projectile risk, and may cause fatal accidents.[135] However, as millions of MRIs are performed globally each year,[136] fatalities are extremely rare.[137]
MRI machines can produce loud noise, up to 120
Overuse
Medical societies issue guidelines for when physicians should use MRI on patients and recommend against overuse. MRI can detect health problems or confirm a diagnosis, but medical societies often recommend that MRI not be the first procedure for creating a plan to diagnose or manage a patient's complaint. A common case is to use MRI to seek a cause of low back pain; the American College of Physicians, for example, recommends against imaging (including MRI) as unlikely to result in a positive outcome for the patient.[25][26]
Artifacts

An MRI artifact is a visual artifact, that is, an anomaly during visual representation. Many different artifacts can occur during magnetic resonance imaging (MRI), some affecting the diagnostic quality, while others may be confused with pathology. Artifacts can be classified as patient-related, signal processing-dependent and hardware (machine)-related.[139]
Non-medical use
MRI is used industrially mainly for routine analysis of chemicals. The nuclear magnetic resonance technique is also used, for example, to measure the ratio between water and fat in foods, monitoring of flow of corrosive fluids in pipes, or to study molecular structures such as catalysts.[1]
Being non-invasive and non-damaging, MRI can be used to study the anatomy of plants, their water transportation processes and water balance.[140] It is also applied to veterinary radiology for diagnostic purposes. Outside this, its use in zoology is limited due to the high cost; but it can be used on many species.[141]
In palaeontology it is used to examine the structure of fossils.[142]
Forensic imaging provides graphic documentation of an autopsy, which manual autopsy does not. CT scanning provides quick whole-body imaging of skeletal and parenchymal alterations, whereas MR imaging gives better representation of soft tissue pathology.[143] All that being said, MRI is more expensive, and more time-consuming to utilize.[143] Moreover, the quality of MR imaging deteriorates below 10 °C.[144]
History
In 1971 at
Raymond Damadian’s work into nuclear magnetic resonance (NMR) has been incorporated into MRI, having built one of the first scanners.[147]
Advances in
See also
- Amplified magnetic resonance imaging
- Cerebrospinal fluid flow MRI
- Electron paramagnetic resonance
- High-definition fiber tracking
- High-resolution computed tomography
- History of neuroimaging
- International Society for Magnetic Resonance in Medicine
- Jemris
- List of neuroimaging software
- Magnetic immunoassay
- Magnetic particle imaging
- Magnetic resonance elastography
- Magnetic Resonance Imaging (journal)
- Magnetic resonance microscopy
- Nobel Prize controversies – Physiology or medicine
- Rabi cycle
- Robinson oscillator
- Sodium MRI
- Virtopsy
References
- ^ a b c Rinck, Peter A. (2024). Magnetic Resonance in Medicine. A critical introduction. e-Textbook (14th ed.). TRTF – The Round Table Foundation: TwinTree Media. "Magnetic Resonance in Medicine". www.magnetic-resonance.org.
- ISBN 978-1-139-45719-4.
- ^ .
- PMID 22692172.
- ISBN 978-92-64-07555-9.
- ^ ISBN 978-0-521-68384-5.
- ^ "Tesla Engineering Ltd - Magnet Division - MRI Supercon". www.tesla.co.uk. Retrieved 2022-08-16.
- ^ Qiuliang, Wang (January 2022). "Successful Development of a 9.4T/800mm Whole-body MRI Superconducting Magnet at IEE CAS" (PDF). snf.ieeecsc.org. Archived (PDF) from the original on Mar 22, 2023.
- S2CID 53153608.
- ^ CEA (2021-10-07). "The most powerful MRI scanner in the world delivers its first images!". CEA/English Portal. Retrieved 2022-08-16.
- S2CID 4054160.
- S2CID 242194782.
- PMID 2107675.
- ^ "Guildford company gets FDA approval for bedside MRI". New Haven Register. 12 February 2020. Archived from the original on 3 April 2020. Retrieved 15 April 2020.
- PMID 15141077.
- S2CID 119160258.
- S2CID 40026232.
- PMID 25975847.
- ^ http://imserc.northwestern.edu/downloads/nmr-t1.pdf.
{{cite web}}: Missing or empty|title=(help) - ^ McHale, J. (2017). Molecular Spectroscopy. CRC Press/Taylor and Francis Group. pp. 73–80.
- ^ University of Wisconsin. Archived from the originalon 2017-05-10. Retrieved 2016-03-14.
- ^ a b c d e f g h i j k l m n Johnson KA. "Basic proton MR imaging. Tissue Signal Characteristics".[unreliable medical source?]
- ^ a b Patil T (2013-01-18). "MRI sequences". Retrieved 2016-03-14.
- ^ "Magnetic Resonance, a critical peer-reviewed introduction". European Magnetic Resonance Forum. Retrieved 17 November 2014.
- ^ ABIM Foundation. Archived from the original(PDF) on June 24, 2012. Retrieved August 14, 2012.
- ^ a b Consumer Reports; American College of Physicians (April 2012). "Imaging tests for lower-back pain: Why you probably don't need them" (PDF). High Value Care. Archived from the original (PDF) on 15 January 2013. Retrieved August 14, 2012.
- ISBN 978-1-905034-13-0. Archived from the original(PDF) on 2012-09-07. Retrieved 2014-05-29.
- PMID 30807665.
- PMID 31657791.
- ^ American Society of Neuroradiology (2013). "ACR-ASNR Practice Guideline for the Performance and Interpretation of Magnetic Resonance Imaging (MRI) of the Brain" (PDF). Archived from the original (PDF) on 2017-07-12. Retrieved 2013-11-10.
- ^ Rowayda AS (May 2012). "An improved MRI segmentation for atrophy assessment". International Journal of Computer Science Issues (IJCSI). 9 (3).
- ^ Rowayda AS (February 2013). "Regional atrophy analysis of MRI for early detection of alzheimer's disease". International Journal of Signal Processing, Image Processing and Pattern Recognition. 6 (1): 49–53.
- ^ Nolen-Hoeksema S (2014). Abnormal Psychology (Sixth ed.). New York: McGraw-Hill Education. p. 67.
- PMID 27462476.
- ^
Leksell L, Leksell D, Schwebel J (January 1985). "Stereotaxis and nuclear magnetic resonance". Journal of Neurology, Neurosurgery, and Psychiatry. 48 (1): 14–8. PMID 3882889.
- PMID 3329837.
- S2CID 244907903.
- ^ "100-Hour-Long MRI of Human Brain Produces Most Detailed 3D Images Yet". 10 July 2019.
- ^ "Team publishes on highest resolution brain MRI scan".
- PMID 28178995.
- PMID 17412166.
- ISBN 978-1-4160-5534-1.
- S2CID 233314102.
- PMID 17554538.
- PMID 28611728.
- PMID 9821197.
- PMID 22334493.
- PMID 20566796.
- PMID 22821694.
- PMID 19936754.
- S2CID 24048799.
- ISBN 978-0-471-35128-3.[page needed]
- ^ Rinck PA (2014). "Chapter 13: Contrast Agents". Magnetic Resonance in Medicine.
- PMID 8819369.
- ^ "ACR guideline". guideline.gov. 2005. Archived from the original on 2006-09-29. Retrieved 2006-11-22.
- ^ Sergey Shugaev and Peter Caravan, Chapter 1: "Metal Ions in Bio-imaging Techniques: A Short Overview", pp 1-37 in "Metal Ions in Bio-Imaging Techniques" (2021). Editors: Astrid Sigel, Eva Freisinger and Roland K.O. Sigel. Publisher: Walter de Gruyter, Berlin.
de Gruyter.com/document/doi/10.1515/9783110685701-007 DOI 10.1515/9783110685701-007 - FDA. 2018-05-16.
- PMID 17018301.
- ^ "FDA Drug Safety Communication: New warnings for using gadolinium-based contrast agents in patients with kidney dysfunction". Information on Gadolinium-Based Contrast Agents. U.S. Food and Drug Administration. 23 December 2010. Retrieved 12 March 2011.
- ^ "FDA Public Health Advisory: Gadolinium-containing Contrast Agents for Magnetic Resonance Imaging". fda.gov. Archived from the original on 2006-09-28.
- ^ "Gadolinium-containing contrast agents: new advice to minimise the risk of nephrogenic systemic fibrosis". Drug Safety Update. 3 (6): 3. January 2010.
- ^ "MRI Questions and Answers" (PDF). Concord, CA: International Society for Magnetic Resonance in Medicine. Retrieved 2010-08-02.
- ^ "Response to the FDA's May 23, 2007, Nephrogenic Systemic Fibrosis Update1 — Radiology". Radiological Society of North America. 2007-09-12. Archived from the original on 2012-07-19. Retrieved 2010-08-02.
- ^ Jones J, Gaillard F. "MRI sequences (overview)". Radiopaedia. Retrieved 2017-10-15.
- ^ University of Wisconsin. Archived from the originalon 2017-05-10. Retrieved 2016-03-14.
- ^ a b c d Johnson KA. "Basic proton MR imaging. Tissue Signal Characteristics". Harvard Medical School. Archived from the original on 2016-03-05. Retrieved 2016-03-14.
- ^ "MRI Questions, Fast Spin Echo". MRIQuestions.com. Retrieved 2021-05-18.
- ISBN 978-0-7020-4614-8.}
- ^ du Plessis V, Jones J. "MRI sequences (overview)". Radiopaedia. Retrieved 2017-01-13.
- PMID 27057352.
- ^ a b Luijkx T, Weerakkody Y. "Steady-state free precession MRI". Radiopaedia. Retrieved 2017-10-13.
- ^ PMID 19755604.
- ^ a b Di Muzio B, Gaillard F. "Susceptibility weighted imaging". Retrieved 2017-10-15.
- ^ Sharma R, Taghi Niknejad M. "Short tau inversion recovery". Radiopaedia. Retrieved 2017-10-13.
- ^ Berger F, de Jonge M, Smithuis R, Maas M. "Stress fractures". Radiology Assistant. Radiology Society of the Netherlands. Retrieved 2017-10-13.
- ^ Hacking C, Taghi Niknejad M, et al. "Fluid attenuation inversion recoveryg". radiopaedia.org. Retrieved 2015-12-03.
- ^ a b Di Muzio B, Abd Rabou A. "Double inversion recovery sequence". Radiopaedia. Retrieved 2017-10-13.
- ^ Lee M, Bashir U. "Diffusion weighted imaging". Radiopaedia. Retrieved 2017-10-13.
- ^ Weerakkody Y, Gaillard F. "Ischaemic stroke". Radiopaedia. Retrieved 2017-10-15.
- ^ Hammer M. "MRI Physics: Diffusion-Weighted Imaging". XRayPhysics. Retrieved 2017-10-15.
- PMID 21454821.
- ^ a b Smith D, Bashir U. "Diffusion tensor imaging". Radiopaedia. Retrieved 2017-10-13.
- S2CID 24731783.
- ^ Gaillard F. "Dynamic susceptibility contrast (DSC) MR perfusion". Radiopaedia. Retrieved 2017-10-14.
- PMID 22468186.
- ^ "Arterial spin labeling". University of Michigan. Retrieved 2017-10-27.
- ^ Gaillard F. "Arterial spin labelling (ASL) MR perfusion". Radiopaedia. Retrieved 2017-10-15.
- ^ Gaillard F. "Dynamic contrast enhanced (DCE) MR perfusion". Radiopaedia. Retrieved 2017-10-15.
- S2CID 5305422.
- ^ Chou Ih. "Milestone 19: (1990) Functional MRI". Nature. Retrieved 9 August 2013.
- ^ Luijkx T, Gaillard F. "Functional MRI". Radiopaedia. Retrieved 2017-10-16.
- ^ a b "Magnetic Resonance Angiography (MRA)". Johns Hopkins Hospital. Retrieved 2017-10-15.
- ^ Keshavamurthy J, Ballinger R et al. "Phase contrast imaging". Radiopaedia. Retrieved 2017-10-15.
- S2CID 195806833.
- PMID 17599700.
- S2CID 20644834.
- S2CID 32536398.
- ^ "MRI-scanner van 7 miljoen in gebruik" [MRI scanner of €7 million in use] (in Dutch). Medisch Contact. December 5, 2007.
- S2CID 16276001.
- S2CID 8268489.
- S2CID 16840737.
- PMID 10369339.
- ISBN 9781414498881– via Credo Reference.
- S2CID 11944489.
- PMID 19443583.
- ^ "Hyperpolarized Noble Gas MRI Laboratory: Hyperpolarized Xenon MR Imaging of the Brain". Harvard Medical School. Archived from the original on 2018-09-20. Retrieved 2017-07-26.
- .
- .
- S2CID 14022996.
- PMID 31054448.
- PMID 20541655.
- PMID 23335551.
- PMID 17234603.
- PMID 24115049.
- PMID 19295156.
- PMID 23150521.
- S2CID 17505246.
- S2CID 16046989.
- S2CID 14724155.
- ^ S2CID 234995365.
- S2CID 23647168.
- PMID 34008045.
- . Retrieved 2021-11-24.
- ISBN 9783527696017. Archived from the originalon 2022-03-05. Retrieved 2022-03-06.
- PMID 33763021.)
{{cite journal}}: CS1 maint: multiple names: authors list (link - S2CID 11617224.)
{{cite journal}}: CS1 maint: multiple names: authors list (link - S2CID 24244167.)
{{cite journal}}: CS1 maint: multiple names: authors list (link - PMID 23486058.)
{{cite journal}}: CS1 maint: multiple names: authors list (link - S2CID 57880401.
- S2CID 73412175.
- ^ "iRefer". Royal College of Radiologists. Archived from the original on 3 February 2014. Retrieved 10 November 2013.
- PMID 9084025.
- PMID 34415199.
- PMID 32812280.
- ^ Agence France-Presse (30 January 2018). "Man dies after being sucked into MRI scanner at Indian hospital". The Guardian.
- ^ "Magnetic Resonance Imaging (MRI) Exams per 1,000 Population, 2014". OECD. 2016.
- S2CID 25245904.
- S2CID 20684100.
- ^ .
- PMID 17175554.
- S2CID 43555012.
- PMID 26979538.
- ^ S2CID 59304740.
- PMID 24191122.
- S2CID 4176060.
- .
- ^ Sandomir, Richard (August 17, 2022). "Raymond Damadian, Creator of the First M.R.I. Scanner, Dies at 86". The New York Times – via NYTimes.com.
- ISBN 9780199792955.
- ^ "The Nobel Prize in Physiology or Medicine 2003". Nobel Foundation. Archived from the original on 18 July 2007. Retrieved 28 July 2007.
Further reading
- Blümer P (1998). Blümler P, Blümich B, Botto RE, Fukushima E (eds.). Spatially Resolved Magnetic Resonance: Methods, Materials, Medicine, Biology, Rheology, Geology, Ecology, Hardware. Wiley-VCH. ISBN 978-3-527-29637-8.
- Blümich B, Kuhn W (1992). Magnetic Resonance Microscopy: Methods and Applications in Materials Science, Agriculture and Biomedicine. Wiley. ISBN 978-3-527-28403-0.
- Blümich B (2000). NMR Imaging of Materials. Clarendon Press. ISBN 978-0-19-850683-6.
- Eustace SJ, Nelson E (June 2004). "Whole body magnetic resonance imaging". BMJ. 328 (7453): 1387–8. PMID 15191954.
- Farhat IA, Belton P, Webb GA (2007). Magnetic Resonance in Food Science: From Molecules to Man. Royal Society of Chemistry. ISBN 978-0-85404-340-8.
- Fukushima E (1989). NMR in Biomedicine: The Physical Basis. Springer Science & Business Media. ISBN 978-0-88318-609-1.
- Haacke EM, Brown RF, Thompson M, Venkatesan R (1999). Magnetic resonance imaging: Physical principles and sequence design. New York: J. Wiley & Sons. ISBN 978-0-471-35128-3.
- Jin (1998). Electromagnetic Analysis and Design in Magnetic Resonance Imaging. CRC Press. ISBN 978-0-8493-9693-9.
- Kuperman V (2000). Magnetic Resonance Imaging: Physical Principles and Applications. Academic Press. ISBN 978-0-08-053570-8.
- Lee SC, Kim K, Kim J, Lee S, Han Yi J, Kim SW, et al. (June 2001). "One micrometer resolution NMR microscopy". Journal of Magnetic Resonance. 150 (2): 207–13. PMID 11384182.
- Liang ZP, Lauterbur PC (1999). Principles of Magnetic Resonance Imaging: A Signal Processing Perspective. Wiley. ISBN 978-0-7803-4723-6.
- Mansfield P (1982). NMR Imaging in Biomedicine: Supplement 2 Advances in Magnetic Resonance. Elsevier. ISBN 978-0-323-15406-2.
- Pykett IL (May 1982). "NMR imaging in medicine". Scientific American. 246 (5): 78–88. PMID 7079720.
- Rinck PA (ed.). "The history of MRI". TRTF/EMRF.
- Sakr, HM; Fahmy, N; Elsayed, NS; Abdulhady, H; El-Sobky, TA; Saadawy, AM; Beroud, C; Udd, B (1 July 2021). "Whole-body muscle MRI characteristics of LAMA2-related congenital muscular dystrophy children: An emerging pattern". Neuromuscular Disorders. 31 (9): 814–823. S2CID 235691786.
- Schmitt F, Stehling MK, Turner R (1998). Echo-Planar Imaging: Theory, Technique and Application. Springer Berlin Heidelberg. ISBN 978-3-540-63194-1.
- Simon M, Mattson JS (1996). The pioneers of NMR and magnetic resonance in medicine: The story of MRI. Ramat Gan, Israel: Bar-Ilan University Press. ISBN 978-0-9619243-1-7.
- Sprawls P (2000). Magnetic Resonance Imaging: Principles, Methods, and Techniques. Medical Physics Publishing. ISBN 978-0-944838-97-6.
External links
- Rinck PA (ed.). "MRI: A Peer-Reviewed, Critical Introduction". European Magnetic Resonance Forum (EMRF)/The Round Table Foundation (TRTF).
- A Guided Tour of MRI: An introduction for laypeople National High Magnetic Field Laboratory
- The Basics of MRI. Underlying physics and technical aspects.
- Video: What to Expect During Your MRI Exam from the Institute for Magnetic Resonance Safety, Education, and Research (IMRSER)
- Royal Institution Lecture – MRI: A Window on the Human Body
- A Short History of Magnetic Resonance Imaging from a European Point of View
- How MRI works explained simply using diagrams
- Real-time MRI videos: Biomedizinische NMR Forschungs GmbH.
- Paul C. Lauterbur, Genesis of the MRI (Magnetic Resonance Imaging) notebook, September 1971 (all pages freely available for download in variety of formats from Science History Institute Digital Collections at digital.sciencehistory.org)



