Malaria
| Malaria | |
|---|---|
cerebral malaria[2] | |
| Usual onset | 10–15 days post exposure[3] |
| Causes | Plasmodium transmitted to humans by Anopheles mosquitoes[1][4] |
| Diagnostic method | Examination of the blood, antigen detection tests[1] |
| Prevention | Mosquito nets, insect repellent, mosquito control, medications[1] |
| Medication | Antimalarial medication[3] |
| Frequency | 247 million (2021)[5] |
| Deaths | 619,000 (2021)[5] |
Malaria is a
Human malaria is caused by
The risk of disease can be reduced by preventing mosquito bites through the use of
The disease is widespread in the
Signs and symptoms

Adults with malaria tend to experience chills and fever – classically in periodic intense bouts lasting around six hours, followed by a period of sweating and fever relief – as well as headache, fatigue, abdominal discomfort, and muscle pain.[25] Children tend to have more general symptoms: fever, cough, vomiting, and diarrhea.[25]
Initial manifestations of the disease—common to all malaria species—are similar to
The classic symptom of malaria is
Symptoms typically begin 10–15 days after the initial mosquito bite, but can occur as late as several months after infection with some P. vivax strains.[25] Travellers taking preventative malaria medications may develop symptoms once they stop taking the drugs.[25]
Severe malaria is usually caused by P. falciparum (often referred to as falciparum malaria). Symptoms of falciparum malaria arise 9–30 days after infection.[26] Individuals with cerebral malaria frequently exhibit neurological symptoms, including abnormal posturing, nystagmus, conjugate gaze palsy (failure of the eyes to turn together in the same direction), opisthotonus, seizures, or coma.[26]
Complications
Malaria has several serious
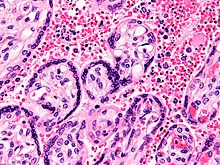
Infection with P. falciparum may result in cerebral malaria, a form of severe malaria that involves
Malaria in pregnant women is an important cause of stillbirths, infant mortality, miscarriage, and low birth weight,[33] particularly in P. falciparum infection, but also with P. vivax.[34]
Cause
Malaria is caused by infection with
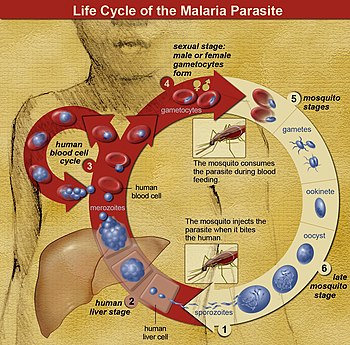
The Anopheles mosquitos initially get infected by Plasmodium by taking a blood meal from a previously Plasmodium infected person.
The liver infection causes no symptoms; all symptoms of malaria result from the infection of red blood cells.
Only female mosquitoes feed on blood; male mosquitoes feed on plant nectar and do not transmit the disease. Females of the mosquito genus Anopheles prefer to feed at night. They usually start searching for a meal at dusk, and continue through the night until they succeed.[46] However, in Africa, due to the extensive use of bed nets, they began to bite earlier, before bed-net time.[47] Malaria parasites can also be transmitted by blood transfusions, although this is rare.[48]
Recurrent malaria
Symptoms of malaria can recur after varying symptom-free periods. Depending upon the cause, recurrence can be classified as either
Pathophysiology

Malaria infection develops via two phases: one that involves the
After a potential dormant period in the liver, these organisms differentiate to yield thousands of merozoites, which, following rupture of their host cells, escape into the blood and infect red blood cells to begin the erythrocytic stage of the life cycle.[54] The parasite escapes from the liver undetected by wrapping itself in the cell membrane of the infected host liver cell.[55]
Within the red blood cells, the parasites multiply further, again asexually, periodically breaking out of their host cells to invade fresh red blood cells. Several such amplification cycles occur. Thus, classical descriptions of waves of fever arise from simultaneous waves of merozoites escaping and infecting red blood cells.[54]
Some P. vivax sporozoites do not immediately develop into exoerythrocytic-phase merozoites, but instead, produce hypnozoites that remain dormant for periods ranging from several months (7–10 months is typical) to several years.[51] After a period of dormancy, they reactivate and produce merozoites. Hypnozoites are responsible for long incubation and late relapses in P. vivax infections,[51] although their existence in P. ovale is uncertain.[56]
The parasite is relatively protected from attack by the body's immune system because for most of its human life cycle it resides within the liver and blood cells and is relatively invisible to immune surveillance. However, circulating infected blood cells are destroyed in the spleen. To avoid this fate, the P. falciparum parasite displays adhesive proteins on the surface of the infected blood cells, causing the blood cells to stick to the walls of small blood vessels, thereby sequestering the parasite from passage through the general circulation and the spleen.[57] The blockage of the microvasculature causes symptoms such as those in placental malaria.[58] Sequestered red blood cells can breach the blood–brain barrier and cause cerebral malaria.[59]
Genetic resistance
According to a 2005 review, due to the high levels of
The impact of sickle cell trait on malaria immunity illustrates some evolutionary trade-offs that have occurred because of endemic malaria. Sickle cell trait causes a change in the haemoglobin molecule in the blood. Normally, red blood cells have a very flexible, biconcave shape that allows them to move through narrow
Liver dysfunction
Liver dysfunction as a result of malaria is uncommon and usually only occurs in those with another liver condition such as viral hepatitis or chronic liver disease. The syndrome is sometimes called malarial hepatitis.[64] While it has been considered a rare occurrence, malarial hepatopathy has seen an increase, particularly in Southeast Asia and India. Liver compromise in people with malaria correlates with a greater likelihood of complications and death.[64]
Diagnosis
Due to the non-specific nature of malaria symptoms, diagnosis is typically suspected based on symptoms and travel history, then confirmed with a laboratory test to detect the presence of the parasite in the blood (parasitological test). In areas where malaria is common, the
In sub-Saharan Africa, testing is low, with only about one in four (28%) of children with a fever receiving medical advice or a rapid diagnostic test in 2021. There was a 10-percentage point gap in testing between the richest and the poorest children (33% vs 23%). Additionally, a greater proportion of children in Eastern and Southern Africa (36%) were tested than in West and Central Africa (21%).[19] According to UNICEF, 61% of children with a fever were taken for advice or treatment from a health facility or provider in 2021. Disparities are also observed by wealth, with an 18 percentage point difference in care-seeking behaviour between children in the richest (71%) and the poorest (53%) households.[19]
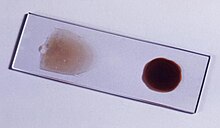
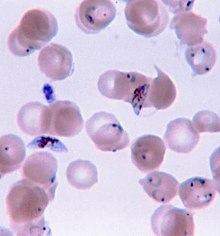
Malaria is usually confirmed by the microscopic examination of
In places where microscopy is unavailable, malaria is diagnosed with RDTs,
Classification
Malaria is classified into either "severe" or "uncomplicated" by the World Health Organization (WHO).[13] It is deemed severe when any of the following criteria are present, otherwise it is considered uncomplicated.[66]
- Decreased consciousness
- Significant weakness such that the person is unable to walk
- Inability to feed
- Two or more convulsions
- mmHgin adults and 50 mmHg in children)
- Breathing problems
- Circulatory shock
- hemoglobinin the urine
- Bleeding problems, or hemoglobin less than 50 g/L (5 g/dL)
- Pulmonary oedema
- Blood glucoseless than 2.2 mmol/L (40 mg/dL)
- Acidosis or lactate levels of greater than 5 mmol/L
- A parasite level in the blood of greater than 100,000 per microlitre(μL) in low-intensity transmission areas, or 250,000 per μL in high-intensity transmission areas
Cerebral malaria is defined as a severe P. falciparum-malaria presenting with neurological symptoms, including coma (with a
Prevention

Methods used to prevent malaria include medications, mosquito elimination and the prevention of bites. As of 2023, there are two malaria vaccines, approved for use in children by the WHO: RTS,S and R21.[14][68] The presence of malaria in an area requires a combination of high human population density, high Anopheles mosquito population density and high rates of transmission from humans to mosquitoes and from mosquitoes to humans. If any of these is lowered sufficiently, the parasite eventually disappears from that area, as happened in North America, Europe, and parts of the Middle East. However, unless the parasite is eliminated from the whole world, it could re-establish if conditions revert to a combination that favors the parasite's reproduction. Furthermore, the cost per person of eliminating anopheles mosquitoes rises with decreasing population density, making it economically unfeasible in some areas.[69]
Prevention of malaria may be more cost-effective than treatment of the disease in the long run, but the
In areas where malaria is common, children under five years old often have
Mosquito control


Insecticide-treated nets
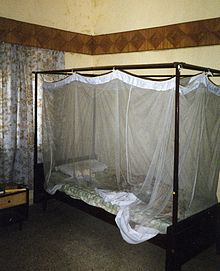
Mosquito nets help keep mosquitoes away from people and reduce infection rates and transmission of malaria. Nets are not a perfect barrier and are often treated with an insecticide designed to kill the mosquito before it has time to find a way past the net. Insecticide-treated nets (ITNs) are estimated to be twice as effective as untreated nets and offer greater than 70% protection compared with no net.[79] Between 2000 and 2008, the use of ITNs saved the lives of an estimated 250,000 infants in Sub-Saharan Africa.[80] According to UNICEF, only 36% of households had sufficient ITNs for all household members in 2019.[81] In 2000, 1.7 million (1.8%) African children living in areas of the world where malaria is common were protected by an ITN. That number increased to 20.3 million (18.5%) African children using ITNs in 2007, leaving 89.6 million children unprotected[82] and to 68% African children using mosquito nets in 2015.[83] The percentage of children sleeping under ITNs in sub-Saharan Africa increased from less than 40% in 2011 to over 50% in 2021.[19] Most nets are impregnated with pyrethroids, a class of insecticides with low toxicity. They are most effective when used from dusk to dawn.[84] It is recommended to hang a large "bed net" above the center of a bed and either tuck the edges under the mattress or make sure it is large enough such that it touches the ground.[85] ITNs are beneficial towards pregnancy outcomes in malaria-endemic regions in Africa but more data is needed in Asia and Latin America.[86]
In areas of high malaria resistance, piperonyl butoxide (PBO) combined with pyrethroids in mosquito netting is effective in reducing malaria infection rates.[87] Questions remain concerning the durability of PBO on nets as the impact on mosquito mortality was not sustained after twenty washes in experimental trials.[87]
UNICEF notes that the use of insecticide-treated nets has been increased since 2000 through accelerated production, procurement and delivery, stating that "over 2.5 billion ITNs have been distributed globally since 2004, with 87% (2.2 billion) distributed in sub-Saharan Africa. In 2021, manufacturers delivered about 220 million ITNs to malaria endemic countries, a decrease of 9 million ITNs compared with 2020 and 33 million less than were delivered in 2019".[20] As of 2021, 66% of households in sub-Saharan Africa had ITNs, with figures "ranging from 31 per cent in Angola in 2016 to approximately 97 per cent in Guinea-Bissau in 2019".[20] Slightly more than half of the households with an ITN had enough of them to protect all members of the household, however.[20]
Indoor residual spraying
Indoor residual spraying is the spraying of insecticides on the walls inside a home. After feeding, many mosquitoes rest on a nearby surface while digesting the bloodmeal, so if the walls of houses have been coated with insecticides, the resting mosquitoes can be killed before they can bite another person and transfer the malaria parasite.
Housing modifications
Housing is a risk factor for malaria and modifying the house as a prevention measure may be a sustainable strategy that does not rely on the effectiveness of insecticides such as pyrethroids.[76][93] The physical environment inside and outside the home that may improve the density of mosquitoes are considerations. Examples of potential modifications include how close the home is to mosquito breeding sites, drainage and water supply near the home, availability of mosquito resting sites (vegetation around the home), the proximity to live stock and domestic animals, and physical improvements or modifications to the design of the home to prevent mosquitoes from entering,[76] such as window screens.
Mass drug administration
Mass drug administration (MDA) involves the administration of drugs to the entire population of an area regardless of disease status.[94] A 2021 Cochrane review on the use of community administration of ivermectin found that, to date, low quality evidence shows no significant impact on reducing incidence of malaria transmission from the community administration of ivermectin.[95]
Other mosquito control methods
People have tried a number of other methods to reduce mosquito bites and slow the spread of malaria. Efforts to decrease mosquito larvae by decreasing the availability of open water where they develop, or by adding substances to decrease their development, are effective in some locations.[96] Electronic mosquito repellent devices, which make very high-frequency sounds that are supposed to keep female mosquitoes away, have no supporting evidence of effectiveness.[97] There is a low certainty evidence that fogging may have an effect on malaria transmission.[98] Larviciding by hand delivery of chemical or microbial insecticides into water bodies containing low larval distribution may reduce malarial transmission.[99] There is insufficient evidence to determine whether larvivorous fish can decrease mosquito density and transmission in the area.[100]
Medications
There are a number of medications that can help prevent or interrupt malaria in travellers to places where infection is common. Many of these medications are also used in treatment. In places where Plasmodium is resistant to one or more medications, three medications—mefloquine, doxycycline, or the combination of atovaquone/proguanil (Malarone)—are frequently used for prevention.[101] Doxycycline and the atovaquone/proguanil are better tolerated while mefloquine is taken once a week.[101] Areas of the world with chloroquine-sensitive malaria are uncommon.[102] Antimalarial mass drug administration to an entire population at the same time may reduce the risk of contracting malaria in the population, however the effectiveness of mass drug administration may vary depending on the prevalence of malaria in the area.[103] Other factors such as drug administration plus other protective measures such as mosquito control, the proportion of people treated in the area, and the risk of reinfection with malaria may play a role in the effectiveness of mass drug treatment approaches.[103]
The protective effect does not begin immediately, and people visiting areas where malaria exists usually start taking the drugs one to two weeks before they arrive, and continue taking them for four weeks after leaving (except for atovaquone/proguanil, which only needs to be started two days before and continued for seven days afterward).
Giving antimalarial drugs to infants through intermittent preventive therapy can reduce the risk of having malaria infection, hospital admission, and anaemia.[108]
Mefloquine is more effective than sulfadoxine-pyrimethamine in preventing malaria for HIV-negative pregnant women. Cotrimoxazole is effective in preventing malaria infection and reduce the risk of getting anaemia in HIV-positive women.[109] Giving sulfadoxine-pyrimethamine for three or more doses as intermittent preventive therapy is superior than two doses for HIV-positive women living in malaria-endemic areas.[110]
Prompt treatment of confirmed cases with artemisinin-based combination therapies (ACTs) may also reduce transmission.[111]
Research on malaria vaccines
Malaria vaccines have been another goal of research. The first promising studies demonstrating the potential for a malaria vaccine were performed in 1967 by immunising mice with live, radiation-attenuated sporozoites, which provided significant protection to the mice upon subsequent injection with normal, viable sporozoites. Since the 1970s, there has been considerable progress in developing similar vaccination strategies for humans.[112]
In 2013, WHO and the malaria vaccine funders group set a goal to develop vaccines designed to interrupt malaria transmission with malaria eradication's long-term goal.[113] The first vaccine, called RTS,S, was approved by European regulators in 2015.[114] As of 2023, two malaria vaccine have been licensed for use.[14] Other approaches to combat malaria may require investing more in research and greater primary health care.[115] Continuing surveillance will also be important to prevent the return of malaria in countries where the disease has been eliminated.[116]
As of 2019 it is undergoing pilot trials in 3 sub-Saharan African countries – Ghana, Kenya and Malawi – as part of the WHO's Malaria Vaccine Implementation Programme (MVIP).[117]
Immunity (or, more accurately,
As of 2020, the RTS,S vaccine has been shown to reduce the risk of malaria by about 40% in children in Africa.[68][123] A preprint study of the R21 vaccine has shown 77% vaccine efficacy.[needs update][124]
In 2021, researchers from the University of Oxford reported findings from a Phase IIb trial of a candidate malaria vaccine, R21/Matrix-M, which demonstrated efficacy of 77% over 12-months of follow-up. This vaccine is the first to meet the World Health Organization's Malaria Vaccine Technology Roadmap goal of a vaccine with at least 75% efficacy.[125]
Germany-based BioNTECH SE are developing an mRNA-based malaria vaccine BN165 [126] which has recently initiated a Phase 1 study [clinicaltrials.gov identifier: NCT05581641] in December 2022. The vaccine, based on the circumsporozite protein (CSP) is being tested in adults aged 18–55 yrs at 3 dose levels to select a safe and tolerable dose of a 3-dose schedule. Unlike GSK's RTS,S (AS01) and Serum Institute of India's R21/MatrixM, BNT-165 is being studied in adult age groups meaning it could be developed for Western travelers as well as those living in endemic countries. For the travelers profile, a recent commercial assessment forecast potential gross revenues of BNT-165 at $479m (2030) 5-yrs post launch, POS-adjusted revenues.[127]
Others
Community participation and health education strategies promoting awareness of malaria and the importance of control measures have been successfully used to reduce the incidence of malaria in some areas of the developing world.[128] Recognising the disease in the early stages can prevent it from becoming fatal. Education can also inform people to cover over areas of stagnant, still water, such as water tanks that are ideal breeding grounds for the parasite and mosquito, thus cutting down the risk of the transmission between people. This is generally used in urban areas where there are large centers of population in a confined space and transmission would be most likely in these areas.[129] Intermittent preventive therapy is another intervention that has been used successfully to control malaria in pregnant women and infants,[130] and in preschool children where transmission is seasonal.[131]
Treatment

Malaria is treated with
Uncomplicated malaria
Simple or uncomplicated malaria may be treated with oral medications. Artemisinin drugs are effective and safe in treating uncomplicated malaria.
Infection with P. vivax, P. ovale or P. malariae usually does not require hospitalisation. Treatment of P. vivax malaria requires both elimination of the parasite in the blood with chloroquine or with artemisinin-based combination therapy and clearance of parasites from the liver with an
To treat malaria during pregnancy, the WHO recommends the use of quinine plus clindamycin early in the pregnancy (1st trimester), and ACT in later stages (2nd and 3rd trimesters).[157][158] There is limited safety data on the antimalarial drugs in pregnancy.[159]
Severe and complicated malaria
Cases of severe and complicated malaria are almost always caused by infection with P. falciparum. The other species usually cause only febrile disease.[160] Severe and complicated malaria cases are medical emergencies since mortality rates are high (10% to 50%).[161]
Recommended treatment for severe malaria is the
Cerebral malaria is the form of severe and complicated malaria with the worst neurological symptoms.[171] There is insufficient data on whether osmotic agents such as mannitol or urea are effective in treating cerebral malaria.[172] Routine phenobarbitone in cerebral malaria is associated with fewer convulsions but possibly more deaths.[173] There is no evidence that steroids would bring treatment benefits for cerebral malaria.[174]
Managing Cerebral Malaria
Cerebral malaria usually makes a patient comatose. If the cause of the coma is in doubt, testing for other locally prevalent causes of encephalopathy (bacterial, viral or fungal infection) should be carried out. In areas where there is a high prevalence of malaria infection (e.g. tropical region) treatment can start without testing first.[35] To manage the cerebral malaria when confirmed the following can be done:
- Patients in coma should be given meticulous nursing care ( monitor vital signs, turn patient every 2 hours, avoid lying the patient in a wet bed etc.)
- A sterile urethral catheter should be inserted to help with urinating
- To aspirate stomach content, a sterile nasogastric tube should be inserted.
- In the occasion of convulsions, a slow intravenous injection of benzodiazepine is administered.[175]
There is insufficient evidence to show that blood transfusion is useful in either reducing deaths for children with severe anaemia or in improving their
Monoclonal antibodies
A 2022 clinical trial shows that a monoclonal antibody mAb L9LS offers protection against malaria. It binds the Plasmodium falciparum circumsporozoite protein (CSP-1), essential to disease, and makes it ineffective.[178]
Resistance
Drug resistance poses a growing problem in 21st-century malaria treatment.[179] In the 2000s (decade), malaria with partial resistance to artemisins emerged in Southeast Asia.[180][181] Resistance is now common against all classes of antimalarial drugs apart from artemisinins. Treatment of resistant strains became increasingly dependent on this class of drugs. The cost of artemisinins limits their use in the developing world.[182] Malaria strains found on the Cambodia–Thailand border are resistant to combination therapies that include artemisinins, and may, therefore, be untreatable.[183] Exposure of the parasite population to artemisinin monotherapies in subtherapeutic doses for over 30 years and the availability of substandard artemisinins likely drove the selection of the resistant phenotype.[184] Resistance to artemisinin has been detected in Cambodia, Myanmar, Thailand, and Vietnam,[185] and there has been emerging resistance in Laos.[186][187] Resistance to the combination of artemisinin and piperaquine was first detected in 2013 in Cambodia, and by 2019 had spread across Cambodia and into Laos, Thailand and Vietnam (with up to 80 percent of malaria parasites resistant in some regions).[188]
There is insufficient evidence in unit packaged antimalarial drugs in preventing treatment failures of malaria infection. However, if supported by training of healthcare providers and patient information, there is improvement in compliance of those receiving treatment.[189]
Prognosis
When properly treated, people with malaria can usually expect a complete recovery.
During childhood, malaria causes anaemia during a period of rapid brain development, and also direct brain damage resulting from cerebral malaria.[192] Some survivors of cerebral malaria have an increased risk of neurological and cognitive deficits, behavioural disorders, and epilepsy.[194] Malaria prophylaxis was shown to improve cognitive function and school performance in clinical trials when compared to placebo groups.[192]
Epidemiology
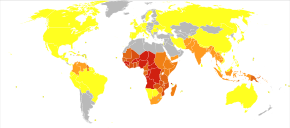


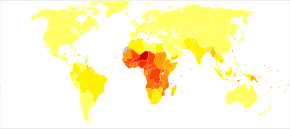
The WHO estimates that in 2021 there were 247 million new cases of malaria resulting in 619,000 deaths.[5] Children under five years old are the most affected, accounting for 67% of malaria deaths worldwide in 2019.[196] About 125 million pregnant women are at risk of infection each year; in Sub-Saharan Africa, maternal malaria is associated with up to 200,000 estimated infant deaths yearly.[33] Since 2015, the WHO European Region has been free of malaria. The last country to report an indigenous malaria case was Tajikistan in 2014.[5] There are about 1300–1500 malaria cases per year in the United States.[29] The United States eradicated malaria as a major public health concern in 1951,[197] though small outbreaks persist.[198] Locally acquired mosquito-borne malaria occurred in the United States in 2003, when eight cases of locally acquired P. vivax malaria were identified in Florida, and again in May 2023, in four cases, as well as one case in Texas,[199] and in August in one case in Maryland.[200] About 900 people died from the disease in Europe between 1993 and 2003.[74] Both the global incidence of disease and resulting mortality have declined in recent years. According to the WHO and UNICEF, deaths attributable to malaria in 2015 were reduced by 60%[83] from a 2000 estimate of 985,000, largely due to the widespread use of insecticide-treated nets and artemisinin-based combination therapies.[80] Between 2000 and 2019, malaria mortality rates among all ages halved from about 30 to 13 per 100,000 population at risk. During this period, malaria deaths among children under five also declined by nearly half (47%) from 781,000 in 2000 to 416,000 in 2019.[81]
Malaria is presently endemic in a broad band around the equator, in areas of the Americas, many parts of Asia, and much of Africa; in Sub-Saharan Africa, 85–90% of malaria fatalities occur.[201] An estimate for 2009 reported that countries with the highest death rate per 100,000 of population were Ivory Coast (86.15), Angola (56.93) and Burkina Faso (50.66).[202] A 2010 estimate indicated the deadliest countries per population were Burkina Faso, Mozambique and Mali.[203] The Malaria Atlas Project aims to map global levels of malaria, providing a way to determine the global spatial limits of the disease and to assess disease burden.[204][205] This effort led to the publication of a map of P. falciparum endemicity in 2010 and an update in 2019.[206][207][208] As of 2021, 84 countries have endemic malaria.[5]
The geographic distribution of malaria within large regions is complex, and malaria-afflicted and malaria-free areas are often found close to each other.[209] Malaria is prevalent in tropical and subtropical regions because of rainfall, consistent high temperatures and high humidity, along with stagnant waters where mosquito larvae readily mature, providing them with the environment they need for continuous breeding.[210] In drier areas, outbreaks of malaria have been predicted with reasonable accuracy by mapping rainfall.[211] Malaria is more common in rural areas than in cities. For example, several cities in the Greater Mekong Subregion of Southeast Asia are essentially malaria-free, but the disease is prevalent in many rural regions, including along international borders and forest fringes.[212] In contrast, malaria in Africa is present in both rural and urban areas, though the risk is lower in the larger cities.[213]
Climate change
Since 1900 there has been substantial change in temperature and rainfall over Africa.[216] However, factors that contribute to how rainfall results in water for mosquito breeding are complex, incorporating the extent to which it is absorbed into soil and vegetation for example, or rates of runoff and evaporation.[217] Recent research has provided a more in-depth picture of conditions across Africa, combining a malaria climatic suitability model with a continental-scale model representing real-world hydrological processes.[217]
History

Although the parasite responsible for P. falciparum malaria has been in existence for 50,000–100,000 years, the population size of the parasite did not increase until about 10,000 years ago, concurrently with advances in agriculture[218] and the development of human settlements. Close relatives of the human malaria parasites remain common in chimpanzees. Some evidence suggests that the P. falciparum malaria may have originated in gorillas.[219]
References to the unique periodic fevers of malaria are found throughout history.
The term malaria originates from Mediaeval Italian: mala aria—"bad air", a part of miasma theory; the disease was formerly called ague or marsh fever due to its association with swamps and marshland.[225] The term appeared in English at least as early as 1768.[226] Malaria was once common in most of Europe and North America,[227] where it is no longer endemic,[228] though imported cases do occur.[229]
Malaria is not referenced in the medical books of the
Scientific studies on malaria made their first significant advance in 1880, when
In April 1894, a Scottish physician,
In 1896, Amico Bignami discussed the role of mosquitoes in malaria.[241] In 1898, Bignami, Giovanni Battista Grassi and Giuseppe Bastianelli succeeded in showing experimentally the transmission of malaria in humans, using infected mosquitoes to contract malaria themselves which they presented in November 1898 to the Accademia dei Lincei.[238]

The first effective treatment for malaria came from the bark of
Quinine was the predominant malarial medication until the 1920s when other medications began to appear. In the 1940s, chloroquine replaced quinine as the treatment of both uncomplicated and severe malaria until resistance supervened, first in Southeast Asia and South America in the 1950s and then globally in the 1980s.[245]
The medicinal value of
Plasmodium vivax was used between 1917 and the 1940s for

The first pesticide used for indoor residual spraying was
Names
Various types of malaria have been called by the names below:[254]
| Name | Pathogen | Notes |
|---|---|---|
| algid malaria | Plasmodium falciparum | severe malaria affecting the circulatory shock
|
| bilious malaria | Plasmodium falciparum | severe malaria affecting the liver and causing vomiting and jaundice |
| cerebral malaria | Plasmodium falciparum | severe malaria affecting the cerebrum |
| congenital malaria | various plasmodia | Plasmodium introduced from the mother via the fetal circulation |
| pernicious malaria | Plasmodium falciparum | severe malaria leading to grave illness |
| malignant malaria | Plasmodium falciparum | severe malaria leading to death |
| falciparum malaria, Plasmodium falciparum malaria, | Plasmodium falciparum | |
| ovale malaria, Plasmodium ovale malaria | Plasmodium ovale | |
| quartan malaria, malariae malaria, Plasmodium malariae malaria | Plasmodium malariae | paroxysms every fourth day (quartan), counting the day of occurrence as the first day |
| quotidian malaria | Plasmodium falciparum, Plasmodium vivax, Plasmodium knowlesi | paroxysms daily (quotidian) |
| tertian malaria | Plasmodium falciparum, Plasmodium ovale, Plasmodium vivax | paroxysms every third day (tertian), counting the day of occurrence as the first |
| transfusion malaria | various plasmodia | Plasmodium introduced by blood transfusion, needle sharing, or needlestick injury |
| vivax malaria, Plasmodium vivax malaria | Plasmodium vivax |
Eradication efforts
Malaria has been successfully eliminated or significantly reduced in certain areas, but not globally. Malaria was once common in the United States, but the US eliminated malaria from most parts of the country in the early 20th century using vector control programs, which combined the monitoring and treatment of infected humans, draining of
In parts of the world with rising living standards, the elimination of malaria was often a collateral benefit of the introduction of window screens and improved sanitation.
Initial WHO program (1955–1969)
In 1955 the WHO launched the Global Malaria Eradication Program (GMEP).[260] The program relied largely on DDT for mosquito control and rapid diagnosis and treatment to break the transmission cycle.[261] The program eliminated the disease in "North America, Europe, the former Soviet Union",[262] and in "Taiwan, much of the Caribbean, the Balkans, parts of northern Africa, the northern region of Australia, and a large swath of the South Pacific"[258] and dramatically reduced mortality in Sri Lanka and India.[263]
However, failure to sustain the program, increasing mosquito tolerance to DDT, and increasing parasite tolerance led to a resurgence. In many areas early successes partially or completely reversed, and in some cases rates of transmission increased.[264] Experts tie malarial resurgence to multiple factors, including poor leadership, management and funding of malaria control programs; poverty; civil unrest; and increased irrigation. The evolution of resistance to first-generation drugs (e.g. chloroquine) and to insecticides exacerbated the situation.[265][266] The program succeeded in eliminating malaria only in areas with "high socio-economic status, well-organized healthcare systems, and relatively less intensive or seasonal malaria transmission".[262]
For example, in Sri Lanka, the program reduced cases from about one million per year before spraying to just 18 in 1963[267][268] and 29 in 1964. Thereafter the program was halted to save money and malaria rebounded to 600,000 cases in 1968 and the first quarter of 1969. The country resumed DDT vector control but the mosquitoes had evolved resistance in the interim, presumably because of continued agricultural use. The program switched to malathion, but despite initial successes, malaria continued its resurgence into the 1980s.[263][269]
Due to vector and parasite resistance and other factors, the feasibility of eradicating malaria with the strategy used at the time and resources available led to waning support for the program.[270] WHO suspended the program in 1969[260][270] and attention instead focused on controlling and treating the disease. Spraying programs (especially using DDT) were curtailed due to concerns over safety and environmental effects, as well as problems in administrative, managerial and financial implementation.[264] Efforts shifted from spraying to the use of bednets impregnated with insecticides and other interventions.[262][271]
Post-1969

Target 6C of the Millennium Development Goals included reversal of the global increase in malaria incidence by 2015, with specific targets for children under five years old.[272] Since 2000, support for malaria eradication increased, although some actors in the global health community (including voices within the WHO) view malaria eradication as a premature goal and suggest that the establishment of strict deadlines for malaria eradication may be counterproductive as they are likely to be missed.[273] One of the targets of Goal 3 of the UN's Sustainable Development Goals is to end the malaria epidemic in all countries by 2030.
In 2006, the organization Malaria No More set a public goal of eliminating malaria from Africa by 2015, and the organization claimed they planned to dissolve if that goal was accomplished. In 2007, World Malaria Day was established by the 60th session of the World Health Assembly. As of 2018, they are still functioning.[274]
As of 2012[update], The Global Fund to Fight AIDS, Tuberculosis, and Malaria has distributed 230 million insecticide-treated nets intended to stop mosquito-borne transmission of malaria.[275] The U.S.-based Clinton Foundation has worked to manage demand and stabilize prices in the artemisinin market.[276] Other efforts, such as the Malaria Atlas Project, focus on analysing climate and weather information required to accurately predict malaria spread based on the availability of habitat of malaria-carrying parasites.[204] The Malaria Policy Advisory Committee (MPAC) of the World Health Organization (WHO) was formed in 2012, "to provide strategic advice and technical input to WHO on all aspects of malaria control and elimination".[277]
In 2015 the WHO targeted a 90% reduction in malaria deaths by 2030,[278] and Bill Gates said in 2016 that he thought global eradication would be possible by 2040.[279] According to the WHO's World Malaria Report 2015, the global mortality rate for malaria fell by 60% between 2000 and 2015. The WHO targeted a further 90% reduction between 2015 and 2030,[280] with a 40% reduction and eradication in 10 countries by 2020.[281] However, the 2020 goal was missed with a slight increase in cases compared to 2015.[282] Additionally, UNICEF reported that the number of malaria deaths for all ages increased by 10% between 2019 and 2020, in part due to service disruptions related to the COVID-19 pandemic, before experiencing a minor decline in 2021.[19]
Before 2016, the Global Fund against HIV/AIDS, Tuberculosis and Malaria had provided 659 million ITN (insecticide treated bed nets), organise support and education to prevents malaria. The challenges are high due to the lack of funds, the fragile health structure and the remote indigenous population that could be hard to reach and educate. Most of indigenous population rely on self-diagnosis, self-treatment, healer, and traditional medicine. The WHO applied for fund to the Gates Foundation which favour the action of malaria eradication in 2007.[283] Six countries, the United Arab Emirates, Morocco, Armenia, Turkmenistan, Kyrgyzstan, and Sri Lanka managed to have no endemic cases of malaria for three consecutive years and certified malaria-free by the WHO despite the stagnation of the funding in 2010.[272] The funding is essential to finance the cost of medication and hospitalisation cannot be supported by the poor countries where the disease is widely spread. The goal of eradication has not been met; nevertheless, the decrease rate of the disease is considerable.
While 31 out of 92 endemic countries were estimated to be on track with the WHO goals for 2020, 15 countries reported an increase of 40% or more between 2015 and 2020.[282] Between 2000 and 30 June 2021, twelve countries were certified by the WHO as being malaria-free. Argentina and Algeria were declared free of malaria in 2019.[282][284] El Salvador and China were declared malaria-free in the first half of 2021.[285][286]
Regional disparities were evident: Southeast Asia was on track to meet WHO's 2020 goals, while Africa, Americas, Eastern Mediterranean and West Pacific regions were off-track.[282] The six Greater Mekong Subregion countries aim for elimination of P. falciparum transmitted malaria by 2025 and elimination of all malaria by 2030, having achieved a 97% and 90% reduction of cases respectively since 2000.[282] Ahead of World Malaria Day, 25 April 2021, WHO named 25 countries in which it is working to eliminate malaria by 2025 as part of its E-2025 initiative.[287]
A major challenge to malaria elimination is the persistence of malaria in border regions, making international cooperation crucial.[288]
In 2018, WHO announced that Paraguay was free of malaria, after a national malaria eradication effort that began in 1950.[289]
As of 2019, the eradication process is ongoing, but it will be difficult to achieve a world free of malaria with the current approaches and tools.
In March 2023, the WHO certified Azerbaijan and Tajikistan as malaria-free,[290] and Belize in June 2023.[291] Cabo Verde, the latest country to eradicate Malaria, was certified in January 2024, bringing the total number of countries and territories certified malaria-free to 44.[292]
Society and culture
Economic impact

Malaria is not just a disease commonly associated with poverty: some evidence suggests that it is also a cause of poverty and a major hindrance to economic development.[21][22] Although tropical regions are most affected, malaria's furthest influence reaches into some temperate zones that have extreme seasonal changes. The disease has been associated with major negative economic effects on regions where it is widespread. During the late 19th and early 20th centuries, it was a major factor in the slow economic development of the American southern states.[293]
A comparison of average per capita
Poverty can increase the risk of malaria since those in poverty do not have the financial capacities to prevent or treat the disease. In its entirety, the economic impact of malaria has been estimated to cost Africa US$12 billion every year. The economic impact includes costs of health care, working days lost due to sickness, days lost in education, decreased productivity due to brain damage from cerebral malaria, and loss of investment and tourism.

Cerebral malaria is one of the leading causes of neurological disabilities in African children.
Counterfeit and substandard drugs
Sophisticated
Another clinical and public health concern is the proliferation of substandard antimalarial medicines resulting from inappropriate concentration of ingredients, contamination with other drugs or toxic impurities, poor quality ingredients, poor stability and inadequate packaging.[302] A 2012 study demonstrated that roughly one-third of antimalarial medications in Southeast Asia and Sub-Saharan Africa failed chemical analysis, packaging analysis, or were falsified.[303]
War

Throughout history, the contraction of malaria has played a prominent role in the fates of government rulers, nation-states, military personnel, and military actions.
Malaria was the most significant health hazard encountered by U.S. troops in the South Pacific during World War II, where about 500,000 men were infected.[307] According to Joseph Patrick Byrne, "Sixty thousand American soldiers died of malaria during the African and South Pacific campaigns."[308]
Significant financial investments have been made to procure existing and create new antimalarial agents. During
Additionally, initiatives have been founded such as Malaria Control in War Areas (MCWA), established in 1942, and its successor, the Communicable Disease Center (now known as the Centers for Disease Control and Prevention, or CDC) established in 1946. According to the CDC, MCWA "was established to control malaria around military training bases in the southern United States and its territories, where malaria was still problematic".[310]
Research
The Malaria Eradication Research Agenda (malERA) initiative was a consultative process to identify which areas of research and development (R&D) must be addressed for worldwide eradication of malaria.[311][312]
Medications
Malaria parasites contain
With the onset of drug-resistant Plasmodium parasites, new strategies are being developed to combat the widespread disease. One such approach lies in the introduction of synthetic
- (+)-SJ733: Part of a wider class of experimental drugs called spiroindolone. It inhibits the ATP4 protein of infected red blood cells that cause the cells to shrink and become rigid like the aging cells. This triggers the immune system to eliminate the infected cells from the system as demonstrated in a mouse model. As of 2014, a Phase 1 clinical trial to assess the safety profile in human is planned by the Howard Hughes Medical Institute.[318]
- NITD246 and NITD609: Also belonged to the class of spiroindolone and target the ATP4 protein.[318]
On the basis of molecular docking outcomes, compounds 3j, 4b, 4h, 4m were exhibited selectivity towards PfLDH. The post docking analysis displayed stable dynamic behavior of all the selected compounds compared to Chloroquine. The end state thermodynamics analysis stated 3j compound as a selective and potent PfLDH inhibitor.[319]
New targets
Targeting Plasmodium liver-stage parasites selectively is emerging as an alternative strategy in the face of resistance to the latest frontline combination therapies against blood stages of the parasite.[320]
In research conducted in 2019, using experimental analysis with knockout (KO) mutants of Plasmodium berghei, the authors were able to identify genes that are potentially essential in the liver stage. Moreover, they generated a computational model to analyse pre–erytrocytic development and liver–stage metabolism. Combining both methods they identified seven metabolic subsystems that become essential compared to the blood stage. Some of these metabolic pathways are fatty acid synthesis and elongation, tricarboxylic acid, amino acid and heme metabolism among others.[320]
Specifically, they studied 3 subsystems: fatty acid synthesis and elongation, and amino sugar biosynthesis. For the first two pathways they demonstrated a clear dependence of the liver stage on its own fatty acid metabolism.[320]
They proved for the first time the critical role of amino sugar biosynthesis in the liver stage of P. berghei. The uptake of N–acetyl–glucosamine appears to be limited in the liver stage, being its synthesis needed for the parasite development.[320]
These findings and the computational model provide a basis for the design of antimalarial therapies targeting metabolic proteins.[320][321]
Other
A non-chemical vector control strategy involves genetic manipulation of malaria mosquitoes. Advances in genetic engineering technologies make it possible to introduce foreign DNA into the mosquito genome and either decrease the lifespan of the mosquito, or make it more resistant to the malaria parasite. Sterile insect technique is a genetic control method whereby large numbers of sterile male mosquitoes are reared and released. Mating with wild females reduces the wild population in the subsequent generation; repeated releases eventually eliminate the target population.[79]
In one study, a genetically modified strain of Anopheles stephensi was created that no longer supported malaria transmission, and this resistance was passed down to mosquito offspring.[324]
Gene drive is a technique for changing wild populations, for instance to combat or eliminate insects so they cannot transmit diseases (in particular mosquitoes in the cases of malaria,[325] zika,[326] dengue and yellow fever).[278]
In a study conducted in 2015, researchers observed a specific interaction between malaria and co-infection with the
Finally, a review article published in December 2020 noted a correlation between malaria-endemic regions and COVID-19 case fatality rates.[328] The study found that, on average, regions where malaria is endemic reported lower COVID-19 case fatality rates compared to regions without endemic malaria.
In 2017, a bacterial strain of the genus Serratia was genetically modified to prevent malaria in mosquitos[329][330] and in 2023, it has been reported that the bacterium Delftia tsuruhatensis naturally prevents the development of malaria by secreting a molecule called Harmane.[331][332][333]
Other animals
While none of the main four species of malaria parasite that cause human infections are known to have
References
- ^ from the original on 2016-08-01.
- ^ "Malaria". Mayo Clinic.
- ^ a b c d e f g h i j k "Malaria Fact sheet N°94". WHO. March 2014. Archived from the original on 3 September 2014. Retrieved 28 August 2014.
- ^ a b "CDC - Malaria - FAQs". 28 June 2023.
- ^ ISBN 978-92-4-006489-8.
- ^ "Vector-borne diseases". www.who.int. Retrieved 2022-04-24.
- PMID 31697788.
- S2CID 11461451.
- ^ a b c d e "Fact sheet about malaria". www.who.int. Retrieved 28 September 2023.
- S2CID 246651569.
- ^ "Fact sheet about malaria". www.who.int. Retrieved 2024-02-19.
- ^ World Health Organization. "Global Technical Strategy for Malaria 2016-2030" (PDF).
- ^ PMID 22632637.
- ^ a b c "WHO recommends R21/Matrix-M vaccine for malaria prevention in updated advice on immunization". 2 October 2023. Retrieved 8 December 2023.
- S2CID 234597200.
- ^ ISBN 978-92-4-154792-5.
- ISBN 978-0-19-185838-3.)
{{cite book}}: CS1 maint: DOI inactive as of January 2024 (link - ^ "World malaria report 2022". www.who.int. Retrieved 2024-01-30.
- ^ a b c d e f g "Malaria in Africa". UNICEF DATA. Retrieved 2023-11-02.
- ^ a b c d "Nearly every minute, a child under 5 dies of malaria". UNICEF. February 2023.
- ^ Institute for the Study of Labor. Archived(PDF) from the original on 2016-03-18.
- ^ PMID 16185240.
- ^ S2CID 208987634.
- ISBN 978-0-443-06839-3.
- ^ a b c d Despommier DD, Griffin DO, Gwadz RW, Hotez PJ, Knirsch CA (2019). "9. The Malarias". Parasitic Diseases (PDF) (7 ed.). New York: Parasites Without Borders. pp. 110–115. Retrieved November 24, 2021.
- ^ PMID 22708041.
- PMID 17123967.
- ISBN 978-1-4160-4919-7.
- ^ PMID 22871759.
- PMID 16229771.
- PMID 21449844.
- ^ Davidson's Principles and Practice of Medicine/21st/351
- ^ S2CID 25560090.
- PMID 22192132. Archived from the originalon 2020-01-23. Retrieved 2019-07-05.
- ^ a b "Malaria - About Malaria - Disease". CDC-Centers for Disease Control and Prevention. 2022-03-22. Retrieved 2022-04-28.
- ^ S2CID 208791451.
- ^ S2CID 20941166.
- PMID 23297258.
- PMID 22233585.
- ^ PMID 22149265.
- PMID 19284287.
- ^ "CDC - Malaria - FAQs". www.cdc.gov. 2023-06-28. Retrieved 2023-10-30.
Only Anopheles mosquitoes can transmit malaria and they must have been infected through a previous blood meal taken from an infected person. When a mosquito bites an infected person, a small amount of blood is taken in which contains microscopic malaria parasites. About 1 week later, when the mosquito takes its next blood meal, these parasites mix with the mosquito's saliva and are injected into the person being bitten.
- ^ "CDC - Malaria - About Malaria - Biology". www.cdc.gov. 2020-07-16. Retrieved 2023-10-30.
Thus the infected mosquito carries the disease from one human to another (acting as a "vector"), while infected humans transmit the parasite to the mosquito, In contrast to the human host, the mosquito vector does not suffer from the presence of the parasites.
- PMID 24037451.
- ^ S2CID 2524633.
- ISBN 978-0-309-09218-0.
- ^ Goldman JG. "Malaria Mosquitoes Are Biting before Bed-Net Time". Scientific American. Retrieved 2023-05-29.
- PMID 20929356.
- ^ WHO 2010, p. vi
- S2CID 1727294.
- ^ PMID 21989376.
- ^ WHO 2010, p. 17
- ^ PMID 22592005.
- ^ S2CID 30660702.
- PMID 18779047.
- S2CID 2044783.
- PMID 21458590.
- PMID 20933151.
- PMID 22460644.
- PMID 29500350.
- PMID 16001361.
- ^ PMID 21427751.
- PMID 18410566.
- ^ from the original on 2013-09-21.
- ^ a b c d e f g h i j k l "5.1 Diagnosing Malaria (2015)". WHO Guidelines for Malaria. World Health Organization. 13 July 2021. Retrieved 28 November 2021.
- ^ WHO 2010, p. 35
- ^ WHO 2010, p. v
- ^ a b "Fact sheet about Malaria". www.who.int. Retrieved 6 May 2020.
- ^ World Health Organization (1958). "Malaria" (PDF). The First Ten Years of the World Health Organization. World Health Organization. pp. 172–87. Archived (PDF) from the original on 2011-07-08.
- PMID 21035839.
- ^ "From 30 million cases to zero: China is certified malaria-free by WHO". www.who.int. Retrieved 2022-08-11.
- ^ "Countries and territories certified malaria-free by WHO". www.who.int. Retrieved 2024-01-30.
- PMID 25582096.
- ^ from the original on 2017-08-30.
- PMID 29405263.
- ^ PMID 36200610.
- PMID 30398672.
- PMID 20393950.
- ^ S2CID 1422449.
- ^ S2CID 15311210.
- ^ a b "Malaria in Africa". UNICEF DATA. Retrieved 2023-10-31.
- PMID 19019422.
- ^ ISBN 978-92-4-150944-2. Archived (PDF) from the original on 5 January 2016. Retrieved 26 December 2015.)
{{cite book}}:|website=ignored (help - ^ Schlagenhauf-Lawlor 2008, p. 215
- ^ Instructions for treatment and use of insecticide-treated mosquito nets (PDF). World Health Organization. 2002. p. 34. Archived (PDF) from the original on 2015-07-06.
- PMID 16625591.
- ^ PMID 34027998.
- PMID 19754246.
- ^ Indoor Residual Spraying: Use of Indoor Residual Spraying for Scaling Up Global Malaria Control and Elimination. WHO Position Statement (PDF) (Report). World Health Organization. 2006. Archived (PDF) from the original on 2008-10-02.
- ^ PMID 20049114.
- PMID 15355233.
- ^ PMID 35038163.
- PMID 26055986.
- PMID 24821920.
- PMID 34184757.
- PMID 36367444.
- PMID 17443590.
- PMID 30388303.
- PMID 31425624.
- PMID 29226959.
- ^ PMID 29083100.
- ^ "Malaria Worldwide – How Can Malaria Cases and Deaths Be Reduced? – Drug resistance in the Malaria Endemic World". Centers for Disease Control and Prevention. Retrieved 4 January 2018.
- ^ PMID 34585740.
- PMID 18687641.
- PMID 21771482.
- PMID 25300703.
- PMID 19200025.
- PMID 34273901.
- PMID 30480761.
- PMID 21975756.
- ^ Palmer J. "WHO gives indoor use of DDT a clean bill of health for controlling malaria". WHO. Archived from the original on 2012-10-22.
- PMID 18973784.
- ^ "World Malaria Report 2013" (PDF). World Health Organization. Retrieved 13 February 2014.
- ^ Walsh F (24 July 2015). "Malaria vaccine gets 'green light'". BBC News Online. Archived from the original on 21 December 2016.
- ^ "Malaria eradication: benefits, future scenarios and feasibility. Executive summary of the report of the WHO Strategic Advisory Group on Malaria Eradication". www.who.int. Archived from the original on August 23, 2019. Retrieved 2019-08-25.
- PMID 31485061.
- ^ World Health Organization (March 2020). "Q&A on the malaria vaccine implementation programme (MVIP)". WHO. Retrieved 6 May 2020.
- PMID 32981095.
- PMID 21893544.
- PMID 21123952.
- PMID 17054281.
- PMID 16625647.
- PMID 26829826. Archived from the original(PDF) on 2020-04-23.
- SSRN 3830681.
- ^ Malaria vaccine becomes first to achieve WHO-specified 75% efficacy goal, News Release 23 April 2021, University of Oxford
- ^ "Home".
- ^ "VacZine Analytics | Our products - MarketVIEW: Travel vaccines segment report".
- PMID 17123898.
- ISBN 978-3-540-48997-9.
- S2CID 25024561.
- PMID 22336792.
- S2CID 220502723.
- ^ Greenwood B (1 January 2004). "Treatment of malaria with antimalarial". Retrieved 26 April 2022.
- PMID 22972057.
- PMID 23728693.
- ^ "Malaria - Diagnosis and treatment - Mayo Clinic". www.mayoclinic.org. Retrieved 2022-04-25.
- PMID 10796519.
- S2CID 18043747.
- PMID 19818169.
- PMID 16625646.
- PMID 16235412.
- ^ WHO 2010, p. 21
- S2CID 209172100.
- PMID 19588433.
- PMID 25702785.
- PMID 16235367.
- PMID 33459345.
- PMID 21328286.
- PMID 16235276.
- PMID 9333058.
- PMID 15495106.
- PMID 29393511.
- PMID 16437507.
- ISBN 978-3-0346-0479-6.
- PMID 32892362.
- PMID 37235326.
- PMID 26962733.
- PMID 22548983.
- PMID 18843672.
- PMID 15705338.
- PMID 16495509.
- ^ "CDC - Malaria - Diagnosis & Treatment (United States) - Treatment (U.S.) - Artesunate dose 400 mg oral". CDC-Centers for Disease Control and Prevention. 2022-04-11. Retrieved 2022-04-25.
- PMID 22696354.
- PMID 20454480. Archived from the originalon 2016-03-04.
- PMID 10796551.
- PMID 15266481.
- PMID 19160229.
- PMID 15495107.
- PMID 24869943.
- PMID 30973639.
- PMID 20606600.
- PMID 21491391.
- PMID 12076440.
- PMID 10796562.
- ISBN 9789241548526.
- PMID 10796646.
- PMID 12804409.
- S2CID 252181345.
- PMID 25402734.
- PMID 22001944.
- PMID 22855752.
- S2CID 39014319.
- PMID 18439351.
- S2CID 39148119.
- ^ World Health Organization (2013). "Q&A on artemisinin resistance". WHO Malaria Publications. Archived from the original on 2016-07-20.
- ^ Briggs H (2014-07-30). "Call for 'radical action' on drug-resistant malaria". BBC News. Retrieved 2023-02-23.
- PMID 25075834.
- ^ Gallagher J (2019-07-23). "Resistant malaria spreading in South East Asia". Retrieved 2019-07-25.
- PMID 15846723.
- ^ "Frequently Asked Questions (FAQs): If I get malaria, will I have it for the rest of my life?". US Centers for Disease Control and Prevention. February 8, 2010. Archived from the original on May 13, 2012. Retrieved 2012-05-14.
- PMID 12930555.
- ^ PMID 21171998.
- S2CID 8763732.
- ^ PMID 20606600.
- PMID 27777030.
- ISBN 978-92-4-004049-6.
- ^ "CDC - Malaria - About Malaria - History - Elimination of Malaria in the United States (1947-1951)". CDC-Centers for Disease Control and Prevention. 28 January 2019. Retrieved 17 January 2020.
- ^ "CDC - Malaria - About Malaria - Malaria Transmission in the United States". CDC-Centers for Disease Control and Prevention. 2019-01-28. Retrieved 2021-09-03.
- ^ Health Alert Network (HAN) (2023-06-26). "Locally Acquired Malaria Cases Identified in the United States". emergency.cdc.gov. Retrieved 2023-06-27.
- ^ "Important Updates on Locally Acquired Malaria Cases Identified in Florida, Texas, and Maryland". Health Alert Network (HAN) - 00496. 2023-08-28. Retrieved 2023-08-28.
- ^ Layne SP. "Principles of Infectious Disease Epidemiology" (PDF). EPI 220. UCLA Department of Epidemiology. Archived from the original (PDF) on 2006-02-20. Retrieved 2007-06-15.
- ^ Provost C (April 25, 2011). "World Malaria Day: Which countries are the hardest hit? Get the full data". The Guardian. Archived from the original on August 1, 2013. Retrieved 2012-05-03.
- S2CID 46171431.
- ^ PMID 17306022.
- PMID 20563310.
- PMID 22185615.
- PMID 31229234.
- PMID 31229233.
- S2CID 4394237.
- ISBN 978-1-77007-353-1.
- PMID 17553244.
- PMID 21382335.
- PMID 21590665.
- ^ "Climate Change And Infectious Diseases" (PDF). Climate Change and Human Health—Risk and Responses. World Health Organization. Archived (PDF) from the original on 2016-03-04.
- ^ "Climate change and human health – risks and responses. Summary". www.who.int. Archived from the original on December 25, 2003. Retrieved 29 October 2018.
- doi:10.3354/cr017145.
- ^ PMID 32859908.
- PMID 20616997.
- PMID 21383971.
- PMID 12364371.
- ^ a b Strong RP (1944). Stitt's Diagnosis, Prevention and Treatment of Tropical Diseases (Seventh ed.). York, PA: The Blakiston Company. p. 3.
- OCLC 538284457.
- ISBN 978-0-19-924850-6.
- ISBN 978-1-85109-658-9.
- PMID 10653562.
- ^ Sharpe S (1768). A view of the customs, manners, drama, &c. of Italy, as they are described in the Frusta letteraria; and in the Account of Italy in English, written by Mr. Baretti; compared with the Letters from Italy, written by Mr. Sharp. London: W. Nicoll.
- ISBN 978-0-521-42354-0.
- ISBN 978-0-521-85447-4.
- ISBN 978-0-521-67012-8.
- PMID 29386521.
- .
- PMID 22203975.
- ^ "Malarial organisms in the blood". Scientific American. 46 (3). Munn & Company: 37–38. 21 January 1882.
- ^ "The Nobel Prize in Physiology or Medicine 1907: Alphonse Laveran". The Nobel Foundation. Archived from the original on 2012-06-23. Retrieved 2012-05-14.
- (PDF) from the original on 2008-07-23.
- PMID 6140039.
- PMID 20786.
- ^ PMID 20205846.
- ^ "Ross and the Discovery that Mosquitoes Transmit Malaria Parasites". CDC Malaria website. Archived from the original on 2007-06-02. Retrieved 2012-06-14.
- ISBN 978-0-405-10628-6.
- ^ "Amico Bignami". www.whonamedit.com. Retrieved 30 July 2019.
- PMID 15669029.
- ^ Pelletier PJ, Caventou JB (1820). "Des recherches chimiques sur les Quinquinas" [Chemical research on quinquinas]. Annales de Chimie et de Physique (in French). 15: 337–65.
- PMID 4600403.
- PMID 21609473.
- ^ WHO monograph on good agricultural and collection practices (GACP) for Artemisia annua L. (PDF). World Health Organization. 2006.
- PMID 23973523.
- PMID 16722826.
- ^ Hao C (29 September 2011). "Lasker Award Rekindles Debate Over Artemisinin's Discovery". News: ScienceInsider. Science/AAAS. Archived from the original on 4 January 2014.
- ^ "Nobel Prize announcement" (PDF). NobelPrize.org. Archived (PDF) from the original on 6 October 2015. Retrieved 5 October 2015.
- PMID 24202156.
- ^ "Eradication of Malaria in the United States (1947–1951)". US Centers for Disease Control and Prevention. February 8, 2010. Archived from the original on May 4, 2012. Retrieved 2012-05-02.
- PMID 12383612.
- ^ "Dorlands.com", dorlands.com, Elsevier, archived from the original on 2014-01-11, retrieved 2016-02-10.
- ISBN 978-1-60623-016-9.
- PMID 14000898.
- ^ "Malaria Elimination Group description and list of elimination countries". Archived from the original on 27 July 2011. Retrieved 2011-07-12.
- ^ a b Gladwell M (July 2, 2001). "The Mosquito Killer". The New Yorker. Archived from the original on April 16, 2016. Retrieved August 20, 2014.
- ^ "World Malaria Report" (PDF). World Health Organization. 2009. Archived (PDF) from the original on January 12, 2010. Retrieved December 17, 2009.
- ^ .
- S2CID 31335358.
- ^ PMID 18165500.
- ^ ISBN 978-0-525-16025-0. Archivedfrom the original on October 19, 2021. Retrieved August 29, 2022.
- ^ S2CID 4346743.
- ^ van den Berg H (October 23, 2008). "Global status of DDT and its alternatives for use in vector control to prevent disease" (PDF). Stockholm Convention on Persistent Organic Pollutants/United Nations Environment Programme. Archived from the original (PDF) on December 17, 2010. Retrieved November 22, 2008.
- PMID 17519417.
- ISBN 978-1-4299-5327-6. Archivedfrom the original on October 19, 2021. Retrieved August 29, 2022.
- ^ McNeil DG (December 27, 2010). "Malaria: A Disease Close to Eradication Grows, Aided by Political Tumult in Sri Lanka". The New York Times. Archived from the original on January 4, 2017. Retrieved February 7, 2017.
- PMID 24548783.
- ^ PMID 21311585.
- from the original on October 17, 2019. Retrieved June 13, 2019.
- ^ PMID 33413683.
- ^ Enserink M (27 August 2019). "Is setting a deadline for eradicating malaria a good idea? Scientists are divided". Science. Retrieved 2019-09-30.
- from the original on December 25, 2011. Retrieved 2012-05-09.
- ^ "Fighting AIDS, Tuberculosis and Malaria". The Global Fund. Archived from the original on 2012-05-05. Retrieved 2012-05-09.
- ^ Schoofs M (July 17, 2008). "Clinton foundation sets up malaria-drug price plan". Wall Street Journal. Archived from the original on January 19, 2016. Retrieved 2012-05-14.
- ^ "Executive summary and key points" (PDF). World Malaria Report 2013. World Health Organization. Archived (PDF) from the original on 4 March 2016. Retrieved 13 February 2014.
- ^ from the original on 2022-01-11. Retrieved 2018-08-12.
- ^ Radwick D (October 5, 2016). "Can Malaria Be Eradicated?". Council on Foreign Relations. Archived from the original on October 5, 2016.
- ^ "Fact Sheet: World Malaria Report 2015". 9 December 2015. Archived from the original on December 17, 2015.
- ^ "Malaria eradication: benefits, future scenarios & feasibility".
- ^ a b c d e "World Malaria Report 2020". www.who.int.
- S2CID 34612426.
- ^ "Algeria and Argentina certified malaria-free by WHO". www.who.int.
- Wikidata Q108595589
- Wikidata Q108595181.
- Wikidata Q108595714
- ^ Ro C (26 September 2019). "The tiny kingdom fighting an epidemic". BBC Future. Retrieved 2019-09-30.
- ^ "WHO certifies Paraguay malaria-free". World Health Organization. 11 June 2018. Retrieved 17 June 2018.
- ^ "WHO certifies Azerbaijan and Tajikistan as malaria-free". World Health Organization. 2023-03-29. Retrieved 2023-06-22.
- ^ "Belize certified malaria-free by WHO". World Health Organization. 2023-06-21. Retrieved 2023-06-22.
- ^ "Who declares Cape Verde free of malaria". World Health Organization. 2024-01-12. Retrieved 2024-01-13.
- ISBN 0-8018-6637-5.
- S2CID 618837.
- ^ Roll Back Malaria WHO partnership (2003). "Economic costs of malaria" (PDF). WHO. Archived from the original (PDF) on 2009-12-29.
- PMID 22973492.
- PMID 16765399.
- PMID 18271620.
- PMID 16931411.
- PMID 15879383.
- S2CID 35470138.
- PMID 18631318.
- PMID 22632187.
- ^ Russell PF (2009). "Communicable diseases Malaria". Medical Department of the United States Army in World War II. U.S. Army Medical Department. Office of Medical History. Archived from the original on October 9, 2012. Retrieved 2012-09-24.
- ^ Melville CH (1910). "The prevention of malaria in war". In Ross R (ed.). The Prevention of Malaria. New York: E.P. Dutton. p. 577. Archived from the original on 2016-03-12.
- ISBN 9780729539296.
- ISBN 978-0-227-17240-7.
- ]
- ^ Kakkilaya BS (April 14, 2006). "History of Malaria During Wars". Malariasite.com. Archived from the original on April 3, 2012. Retrieved 2012-05-03.
- ^ "History | CDC Malaria". US Centers for Disease Control and Prevention. February 8, 2010. Archived from the original on August 28, 2010. Retrieved 2012-05-15.
- PMID 19877843.
- ^ "WHO | A research agenda for malaria eradication". www.who.int. Archived from the original on 2016-03-07. Retrieved 2016-03-07.
- PMID 20491664.
- PMID 19939733.
- PMID 21234302.
- PMID 22362072.
- PMID 22530641.
- ^ a b John C (8 December 2014). "New malaria drug unleashes an immune system assault on infected cells". fiercebiotechresearch.com. Archived from the original on 4 April 2016. Retrieved 16 December 2014.
- S2CID 209894772.
- ^ PMID 31730853.
- S2CID 248741177.
- PMID 12364752.
- S2CID 4376984.
- PMID 26598698.
- ^ "Malarial mosquitoes suppressed in experiments that mimic natural environments". 28 July 2021. Retrieved 21 November 2021.
- ^ Flam F (4 February 2016). "Fighting Zika Virus With Genetic Engineering". Bloomberg. Archived from the original on 6 June 2016.
- ^ PMID 26477454.
- PMID 33365386.
- PMID 28963255.
- ISSN 0036-8075.
- S2CID 260440907.
- ^ Offord, Catherine (3 August 2023). "Microbe stops mosquitoes from harboring malaria parasite". Science.
- ^ "Chance discovery helps fight against malaria". BBC News. 2023-08-04. Retrieved 2023-08-04.
- ^ "Facts about malaria". European Centre for Disease Prevention and Control. 9 June 2017. Retrieved 16 July 2021.
- PMID 28867401.
- ISBN 978-0-387-28294-7.
- PMID 19747661.
- PMID 20456124.
- PMID 18806208.
- S2CID 1885904.
Sources
- WHO (2010). Guidelines for the Treatment of Malaria (PDF) (Report) (2nd ed.). World Health Organization. ISBN 978-92-4-154792-5. Archived from the original(PDF) on March 11, 2010.
- Schlagenhauf-Lawlor P (2008). Travelers' Malaria. PMPH-USA. ISBN 978-1-55009-336-0.
Further reading
- ISBN 978-90-420-0721-5.
- Guidelines for the treatment of malaria (3rd ed.). World Health Organization. 2015. ISBN 978-92-4-154912-7. Archived from the originalon April 25, 2015.
- Jarvis B (29 July 2019). "How Mosquitoes Changed Everything". The New Yorker. Retrieved 8 August 2019.
- "Tightening the handle on malaria". Nature Methods (Editorial). 16 (4): 271. 28 March 2019. PMID 30923375.
A day dedicated to raising awareness of the disease is a good opportunity to ask how far malaria research has come and which methods are needed for further breakthroughs.
External links