Megakaryocyte
| Megakaryocyte | |
|---|---|
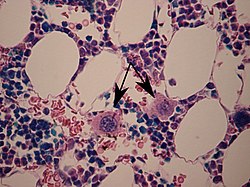 Two megakaryocytes in bone marrow, marked with arrows. | |
| Details | |
| Location | Bone marrow |
| Function | Platelet production |
| Identifiers | |
| Latin | megakaryocytus |
| MeSH | D008533 |
| TH | H2.00.04.3.05003 |
| FMA | 83555 |
| Anatomical terms of microanatomy | |
A megakaryocyte (
Structure
In general, megakaryocytes are 10 to 15 times larger than a typical red blood cell, averaging 50–100 μm in diameter. During its maturation, the megakaryocyte grows in size and replicates its DNA without cytokinesis in a process called endomitosis. As a result, the nucleus of the megakaryocyte can become very large and lobulated, which, under a light microscope, can give the false impression that there are several nuclei. In some cases, the nucleus may contain up to 64N DNA, or 32 copies of the normal complement of DNA in a human cell.
The cytoplasm, just as the platelets that bud off from it, contains α-granules and dense bodies.
Development

Megakaryocytes are derived from
The megakaryocyte develops through the following lineage:CFU-Me (
The cell eventually reaches megakaryocyte stage and loses its ability to divide. However, it is still able to replicate its DNA and continue development, becoming
Function
Platelet release
Once the cell has completed differentiation and become a mature megakaryocyte, it begins the process of producing platelets. The maturation process occurs via endomitotic synchronous replication whereby the cytoplasmic volume enlarges as the number of chromosomes multiplies without cellular division. The cell ceases its growth at 4N, 8N or 16N, becomes granular, and begins to produce platelets.[6] Thrombopoietin plays a role in inducing the megakaryocyte to form small proto-platelet processes. Platelets are held within these internal membranes within the cytoplasm of megakaryocytes. There are two proposed mechanisms for platelet release. In one scenario, these proto-platelet processes break up explosively to become platelets.[7] It is possible to visualize the spontaneous release of platelets using holotomographic live-cell imaging. Alternatively, the cell may form platelet ribbons into blood vessels. The ribbons are formed via pseudopodia and they are able to continuously emit platelets into circulation. In either scenario, each of these proto-platelet processes can give rise to 2000–5000 new platelets upon breakup. Overall, 2/3 of these newly produced platelets will remain in circulation while 1/3 will be sequestered by the spleen.[medical citation needed]
Thrombopoietin (TPO) is a 353-amino acid protein encoded on chromosome 3p27. TPO is primarily synthesized in the liver[8] but can be made by kidneys, testes, brain, and even bone marrow stromal cells. It has high homology with erythropoietin. It is essential for the formation of an adequate quantity of platelets.
After budding off platelets, what remains is mainly the cell nucleus. This crosses the
Effects of cytokines
Clinical significance
Megakaryocytes are directly responsible for producing platelets, which are needed for the formation of a thrombus, or blood clot. There are several diseases that are directly attributable to abnormal megakaryocyte function or abnormal platelet function.[11]
Essential thrombocythemia
Congenital amegakaryocytic thrombocytopenia
Bone marrow/stem cell transplant is the only remedy for this genetic disease. Frequent platelet transfusions are required to keep the patient from bleeding to death until transplant has been completed, although this is not always the case.
There appears to be no generic resource for CAMT patients on the web and this is potentially due to the rarity of the disease.
History
This section needs expansion. You can help by adding to it. (March 2018) |
In 1906, James Homer Wright provided evidence that megakaryocytes give rise to blood platelets.[17]
Kelemen first coined the term "thrombopoietin" to describe the humoral substance responsible for the production of platelets.[18]
See also
References
- PMID 1060175.
- PMID 9345025.
- S2CID 21760081.
- ^ S2CID 23424418.
- PMID 21309084.
- ISBN 978-0-323-04453-0. Archived from the originalon 6 June 2013.
- PMID 7529062.
- PMID 11474308.
- PMID 1627792.
- PMID 16322777.
- S2CID 22268111.
- S2CID 218867974.
- PMID 15858187.
- S2CID 23164119.
- ^ PMID 10077649.
- PMID 11133753.
- .
- PMID 13616931.
External links
- Megakaryocytes: Mature Many microscopic images of mature megakaryocytes including in disease settings.
- Megakaryocytes
- Cell size comparison
- CAMT Specific Infant Bone Marrow Transplant Journal
