Melanocyte
| Melanocyte | |
|---|---|
 Melanocyte and melanin | |
| Details | |
| Pronunciation | /məˈlænəˌsaɪt, -noʊ-/ ⓘ or /ˈmɛlənəˌsaɪt, -noʊ-/[1][2] |
| Precursor | Neural crest |
| Location | Human skin |
| Function | Melanin production |
| Identifiers | |
| Latin | melanocytus |
| MeSH | D008544 |
| TH | H2.00.03.0.01016 |
| FMA | 70545 |
| Anatomical terms of microanatomy | |
Melanocytes are
Function

Through a process called melanogenesis, melanocytes produce melanin, which is a pigment found in the skin, eyes, hair, nasal cavity, and inner ear. This melanogenesis leads to a long-lasting pigmentation, which is in contrast to the pigmentation that originates from oxidation of already-existing melanin.
There are both basal and activated levels of melanogenesis; in general, lighter-skinned people have low basal levels of melanogenesis. Exposure to UV-B radiation causes increased melanogenesis. The purpose of melanogenesis is to protect the hypodermis, the layer under the skin, from damage by UV radiation. The color of the melanin is black, allowing it to absorb a majority of the UV light and block it from passing through the epidermis.[10]
Since the action spectrum of
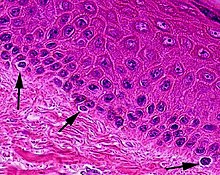
Typically, between 1000 and 2000 melanocytes are found per square millimeter of skin or approximately 5% to 10% of the cells in the basal layer of epidermis. Although their size can vary, melanocytes are typically 7 μm in length.
Both lightly and darkly pigmented skin contain similar numbers of melanocytes, and ACTH peptides that are produced from the precursor proopiomelanocortin.
Vitiligo is a skin disease where people lack melanin in certain areas in the skin.
People with oculocutaneous albinism typically have a very low level of melanin production. Albinism is often but not always related to the TYR gene coding the tyrosinase enzyme. Tyrosinase is required for melanocytes to produce melanin from the amino acid tyrosine.[14] Albinism may be caused by a number of other genes as well, like OCA2,[15] SLC45A2,[16] TYRP1,[17] and HPS1[18] to name some. In all, already 17 types of oculocutaneous albinism have been recognized.[19] Each gene is related to different protein having a role in pigment production.
People with
Role in the immune system
In addition to their role as UV radical scavengers, melanocytes are also part of the immune system, and are considered to be immune cells.[20] Although the full role of melanocytes in immune response is not fully understood, melanocytes share many characteristics with dendritic cells: branched morphology; phagocytic capabilities; presentation of antigens to T-cells; and production and release of cytokines.[20][21][22] Although melanocytes are dendritic in form and share many characteristics with dendritic cells, they derive from different cell lineages. Dendritic cells are derived from hematopoietic stem cells in the bone marrow. Melanocytes on the other hand originate from neural crest cells. As such, although morphologically and functionally similar, melanocytes and dendritic cells are not the same.
Melanocytes are capable of expressing MHC Class II,[21] a type of MHC expressed only by certain antigen presenting cells of the immune system, when stimulated by interactions with antigen or cytokines. All cells in any given vertebrate express MHC, but most cells only express MHC class I. The other class of MHC, Class II, is found only on "professional" antigen presenting cells such as dendritic cells, macrophages, B cells, and melanocytes. Importantly, melanocytes stimulated by cytokines express surface proteins such as CD40 and ICAM1 in addition to MHC class II, allowing for co-stimulation of T cells.[20]
In addition to presenting antigen, one of the roles of melanocytes in the immune response is cytokine production.
Melanocytes are ideally positioned in the epidermis to be sentinels against harmful pathogens. Melanocytes reside in the stratum basale,[23] the lowest layer of the epidermis, but they use their dendrites to interact with cells in other layers,[24] and to capture pathogens that enter the epidermis.[21] Melanocytes likely work in concert with both keratinocytes and Langerhans cells,[20][21] both of which are also actively phagocytic,[23] to contribute to the immune response.
Melanogenesis
Tyrosine is the non-essential amino acid precursor of melanin. Tyrosine is converted to dihydroxyphenylalanine (DOPA) via the enzyme tyrosinase. Then DOPA is polymerized into melanin. The copper-ion based enzyme-catalyzed oxidative transformation of catechol derivative dopa to light absorbing dopaquinone to indole-5,6-quinone is clearly seen following the polymerization to melanin, the color of the pigment ranges from red to dark brown.
Stimulation
Numerous stimuli are able to alter melanogenesis, or the production of melanin by cultured melanocytes, although the method by which it works is not fully understood. Increased melanin production is seen in conditions where
Melanosomes are
Stem cells
The precursor of the melanocyte is the melanoblast. In adults, stem cells are contained in the bulge area of the outer root sheath of hair follicles. When a hair is lost and the hair follicle regenerates, the stem cells are activated. These stem cells develop into both keratinocyte precursors and melanoblasts - and these melanoblasts supply both hair and skin (moving into the basal layer of the epidermis). There is additionally evidence that melanocyte stem cells are present in cutaneous nerves, with nerve signals causing these cells to differentiate into melanocytes for the skin.[27]
Clinical significance
- Melanoma - Cancer affecting melanocytes
- Melanocytic tumors
- Melanocytic tumors of uncertain malignant potential
- Vitiligo - Decreased number of melanocytes due to autoimmune destruction causing decreased melanin
- Albinism - Normal number of melanocytes, but decreased melanin production due to decreased tyrosinase activity or defective tyrosine transport
- Melasma (Chloasma) - Patchy hyperpigmentation of the skin Normal number of melanocytes with increased melanin production causing hyperpigmentation. Associated with pregnancy or oral contraceptive pill use.
- Addison disease
- Nevus depigmentosus
See also
- Chromatophore (the pigment cell type found in poikilotherm animals)
- Eye color
- Mole (skin marking)
- Tanning activator
- List of distinct cell types in the adult human body
- List of human cell types derived from the germ layers
References
- ^ "Melanocyte". Lexico UK English Dictionary. Oxford University Press. Archived from the original on 2020-03-22.
- ^ "Melanocyte". Merriam-Webster.com Dictionary.
- PMID 1992974.
- ^
Barden H, Levine S (June 1983). "Histochemical observations on rodent brain melanin". Brain Research Bulletin. 10 (6): 847–51. S2CID 4783099.
- ^
Markert CL, Silvers WK (May 1956). "The Effects of Genotype and Cell Environment on Melanoblast Differentiation in the House Mouse". Genetics. 41 (3): 429–50. PMID 17247639.
- ISBN 9781451153835.
- ^
Mintz B (1971). "Clonal basis of mammalian differentiation". Symposia of the Society for Experimental Biology. 25: 345–70. PMID 4940552.
- ^
Nichols SE, Reams WM (March 1960). "The occurrence and morphogenesis of melanocytes in the connective tissues of the PET/MCV mouse strain". Journal of Embryology and Experimental Morphology. 8: 24–32. PMID 14426921.
- ^
Theriault LL, Hurley LS (October 1970). "Ultrastructure of developing melanosomes in C57 black and pallid mice". Developmental Biology. 23 (2): 261–75. PMID 5476812.
- ^
Agar N, Young AR (April 2005). "Melanogenesis: a photoprotective response to DNA damage?". Mutation Research. 571 (1–2): 121–32. PMID 15748643.
- ^
Parrish JA, Jaenicke KF, Anderson RR (August 1982). "Erythema and melanogenesis action spectra of normal human skin". Photochemistry and Photobiology. 36 (2): 187–91. S2CID 38940583.
- PMID 15955111.
- ^ PMID 24573849.
- ^ "TYR". National Institutes of Health. Retrieved 23 June 2013.
- ^ "OCA2". National Institutes of Health. Retrieved 25 March 2016.
- ^ "SLC45A2". National Institutes of Health. Retrieved 25 March 2016.
- ^ "TYRP1". National Institutes of Health. Retrieved 25 March 2016.
- ^ "HPS1". National Institutes of Health. Retrieved 25 March 2016.
- S2CID 7305884.
- ^ PMID 26092350.
- ^ PMID 19659579.
- PMID 11419954.
- ^ PMID 29180836.
- PMID 24934806.
- PMID 11041375.
- ^
Eller MS, Maeda T, Magnoni C, Atwal D, Gilchrest BA (November 1997). "Enhancement of DNA repair in human skin cells by thymidine dinucleotides: evidence for a p53-mediated mammalian SOS response". Proceedings of the National Academy of Sciences of the United States of America. 94 (23): 12627–32. PMID 9356500.
- PMID 24278043.
Further reading
- Ito S (June 2003). "The IFPCS presidential lecture: a chemist's view of melanogenesis". Pigment Cell Research. 16 (3): 230–6. PMID 12753395.
- Millington GW (May 2006). "Proopiomelanocortin (POMC): the cutaneous roles of its melanocortin products and receptors". Clinical and Experimental Dermatology. 31 (3): 407–12. S2CID 25213876.
External links
- Histology image: 07903loa – Histology Learning System at Boston University - "Eye: fovea, RPE"
- Histology image: 08103loa – Histology Learning System at Boston University - "Integument: pigmented skin"
