Mental health
The examples and perspective in this article deal primarily with the United States and do not represent a worldwide view of the subject. (July 2021) |
| Part of a series on |
| Mental health |
|---|
| Treated by |
| Studied by |
| Society |
|
| History |
|
| By country |
|
| Part of |
| Part of a series on |
| Public health |
|---|
 |
Mental health encompasses
Mental disorders
Mental health, as defined by the
Mental health is associated with a number of lifestyle factors such as diet, exercise, stress, drug abuse, social connections and interactions.[15][16] Psychiatrists, psychologists, licensed professional clinical counselors, social workers, nurse practitioners, and family physicians can help manage mental illness with treatments such as therapy, counseling, and medication.[17]
History
Early history
In the mid-19th century, William Sweetser was the first to coin the term mental hygiene, which can be seen as the precursor to contemporary approaches to work on promoting positive mental health.[18][19] Isaac Ray, the fourth president[20] of the American Psychiatric Association and one of its founders, further defined mental hygiene as "the art of preserving the mind against all incidents and influences calculated to deteriorate its qualities, impair its energies, or derange its movements".[19]
In American history, mentally ill patients were thought to be religiously punished. This response persisted through the 1700s, along with the inhumane confinement and stigmatization of such individuals.[21] Dorothea Dix (1802–1887) was an important figure in the development of the "mental hygiene" movement. Dix was a school teacher who endeavored to help people with mental disorders and to expose the sub-standard conditions into which they were put.[22] This became known as the "mental hygiene movement".[22] Before this movement, it was not uncommon that people affected by mental illness would be considerably neglected, often left alone in deplorable conditions without sufficient clothing.[22] From 1840 to 1880, she won the support of the federal government to set up over 30 state psychiatric hospitals; however, they were understaffed, under-resourced, and were accused of violating human rights.[21]
At the beginning of the 20th century,
The mental hygiene movement, similar to the
Deinstitutionalization and transinstitutionalization
When US government-run hospitals were accused of violating human rights, advocates pushed for
It has been proven that this transition was beneficial for many patients: there was an increase in overall satisfaction, a better quality of life, and more friendships between patients all at an affordable cost. This proved to be true only in the circumstance that treatment facilities that had enough funding for staff and equipment as well as proper management.[30] However, this idea is a polarizing issue. Critics of deinstitutionalization argue that poor living conditions prevailed, patients were lonely, and they did not acquire proper medical care in these treatment homes.[31] Additionally, patients that were moved from state psychiatric care to nursing and residential homes had deficits in crucial aspects of their treatment. Some cases result in the shift of care from health workers to patients' families, where they do not have the proper funding or medical expertise to give proper care.[31] On the other hand, patients that are treated in community mental health centers lack sufficient cancer testing, vaccinations, or otherwise regular medical check-ups.[31]
Other critics of state deinstitutionalization argue that this was simply a transition to "
Families of patients, advocates, and mental health professionals still call for the increase in more well-structured community facilities and treatment programs with a higher quality of long-term inpatient resources and care. With this more structured environment, the United States will continue with more access to mental health care and an increase in the overall treatment of the mentally ill.
However, there is still a lack of studies for mental health conditions (MHCs) to raise awareness, knowledge development, and attitude of seeking medical treatment for MHCs in Bangladesh. People in rural areas often seek treatment from the traditional healers and MHCs are sometimes considered a spiritual matter.[33]
Epidemiology
Mental illnesses are more common than
Evidence from the WHO suggests that nearly half of the world's population is affected by mental illness with an impact on their self-esteem, relationships and ability to function in everyday life.[39] An individual's emotional health can impact their physical health. Poor mental health can lead to problems such as the inability to make adequate decisions and substance use disorders.[40]
Good mental health can improve life quality whereas poor mental health can worsen it. According to Richards, Campania, & Muse-Burke, "There is growing evidence that is showing emotional abilities are associated with pro-social behaviors such as stress management and physical health."
Global prevalence
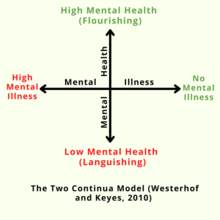
Mental health can be seen as a
A
The tripartite model of mental well-being
Demographics
Children and young adults
Mental health conditions are 16% of the global burden of disease and injury in people aged 10–19 years.[52] 8.9 million young adults are affected by mental illness. 42% of those young adults went untreated as of 2018.[2] In the United States alone in 2021, at least roughly 17.5% of the population (ages 18 and older) were recorded as having a mental illness. The comparison between reports and statistics of mental health issues in newer generations (18–25 years old to 26–49 years old) and the older generation (50 years or older) signifies an increase in mental health issues as only 15% of the older generation reported a mental health issue whereas the newer generations reported 33.7% (18-25) and 28.1% (26-49).[53] Half of all mental health conditions start by 14 years of age but most cases go undetected and untreated.[54][52] The role of caregivers for youth with mental health needs is valuable, and caregivers benefit most when they have sufficient psychoeducation and peer support.[55] Depression is one of the leading causes of illness and disability among adolescents.[52] Suicide is the fourth leading cause of death in 15-19-year-olds.[52] Exposure to childhood trauma can cause mental health disorders and poor academic achievement.[56] Ignoring mental health conditions in adolescents can impact adulthood.[57] 50% of preschool children show a natural reduction in behavioral problems. The remaining experience long-term consequences.[57] It impairs physical and mental health and limits opportunities to live fulfilling lives.[57] A result of depression during adolescence and adulthood may be substance abuse.[57][58] The average age of onset is between 11 and 14 years for depressive disorders.[58] Only approximately 25% of children with behavioral problems refer to medical services.[57] The majority of children go untreated.[57]
Homeless population
Mental illness is thought to be highly prevalent among homeless populations, though access to proper diagnoses is limited. An article written by Lisa Goodman and her colleagues summarized Smith's research into PTSD in homeless single women and mothers in St. Louis, Missouri, which found that 53% of the respondents met diagnostic criteria, and which describes homelessness as a risk factor for mental illness.[59] At least two commonly reported symptoms of psychological trauma, social disaffiliation and learned helplessness are highly prevalent among homeless individuals and families.[60]
While mental illness is prevalent, people infrequently receive appropriate care.[59] Case management linked to other services is an effective care approach for improving symptoms in people experiencing homelessness.[60] Case management reduced admission to hospitals, and it reduced substance use by those with substance abuse problems more than typical care.[60]
Immigrants and refugees
States that produce refugees are sites of social upheaval, civil war, even genocide.[61] Most refugees experience trauma. It can be in the form of torture, sexual assault, family fragmentation, and death of loved ones.[61][62]
Refugees and immigrants experience psychosocial stressors after resettlement.[63] These include discrimination, lack of economic stability, and social isolation causing emotional distress. For example, Not far into the 1900s, campaigns targeting Japanese immigrants were being formed that inhibited their ability to participate in U.S life, painting them as a threat to the American working-class. They were subject to prejudice and slandered by American media as well as anti-Japanese legislation being implemented.[64] [61][62] For refugees family reunification can be one of the primary needs to improve quality of life.[61] Post-migration trauma is a cause of depressive disorders and psychological distress for immigrants.[61][62][63]
Cultural and religious considerations
Mental health is a socially constructed concept; different societies, groups, cultures (both ethnic and national/regional), institutions, and professions have very different ways of conceptualizing its nature and causes, determining what is mentally healthy, and deciding what interventions, if any, are appropriate.[65] Thus, different professionals will have different cultural, class, political and religious backgrounds, which will impact the methodology applied during treatment. In the context of deaf mental health care, it is necessary for professionals to have cultural competency of deaf and hard of hearing people and to understand how to properly rely on trained, qualified, and certified interpreters when working with culturally Deaf clients.
Research has shown that there is stigma attached to mental illness.[66] Due to such stigma, individuals may resist labeling and may be driven to respond to mental health diagnoses with denialism.[67] Family caregivers of individuals with mental disorders may also suffer discrimination or face stigma.[68]
Addressing and eliminating the social stigma and perceived stigma attached to mental illness has been recognized as crucial to education and awareness surrounding mental health issues. In the United Kingdom, the Royal College of Psychiatrists organized the campaign Changing Minds (1998–2003) to help reduce stigma,[69] while in the United States, efforts by entities such as the Born This Way Foundation and The Manic Monologues specifically focus on removing the stigma surrounding mental illness.[70][71] The National Alliance on Mental Illness (NAMI) is a U.S. institution founded in 1979 to represent and advocate for those struggling with mental health issues. NAMI helps to educate about mental illnesses and health issues, while also working to eliminate stigma[72] attached to these disorders.
Many mental health professionals are beginning to, or already understand, the importance of competency in religious diversity and spirituality, or the lack thereof. They are also partaking in cultural training to better understand which interventions work best for these different groups of people. The American Psychological Association explicitly states that religion must be respected. Education in spiritual and religious matters is also required by the American Psychiatric Association,[73] however, far less attention is paid to the damage that more rigid, fundamentalist faiths commonly practiced in the United States can cause.[74][unreliable source?] This theme has been widely politicized in 2018 such as with the creation of the Religious Liberty Task Force in July of that year.[75] Also, many providers and practitioners in the United States are only beginning to realize that the institution of mental healthcare lacks knowledge and competence of many non-Western cultures, leaving providers in the United States ill-equipped to treat patients from different cultures.[76]
Occupations
Occupational therapy
Occupational therapy practitioners aim to improve and enable a client or group's participation in meaningful, everyday occupations.[77] In this sense, occupation is defined as any activity that "occupies one's time". Examples of those activities include daily tasks (dressing, bathing, eating, house chores, driving, etc.), sleep and rest, education, work, play, leisure (hobbies), and social interactions. The OT profession offers a vast range of services for all stages of life in a myriad of practice settings, though the foundations of OT come from mental health. Community support for mental health through expert-moderated support groups can aid those who want to recover from mental illness or otherwise improve their emotional well-being.[78]
OT services focused on mental health can be provided to persons, groups, and populations [77] across the lifespan and experiencing varying levels of mental health performance. For example, occupational therapy practitioners provide mental health services in school systems, military environments, hospitals, outpatient clinics, and inpatient mental health rehabilitation settings. Interventions or support can be provided directly through specific treatment interventions or indirectly by providing consultation to businesses, schools, or other larger groups to incorporate mental health strategies on a programmatic level. Even people who are mentally healthy can benefit from the health promotion and additional prevention strategies to reduce the impact of difficult situations.
The interventions focus on positive functioning, sensory strategies, managing emotions, interpersonal relationships, sleep, community engagement, and other cognitive skills (i.e. visual-perceptual skills, attention, memory, arousal/energy management, etc.).
Mental health in social work
Social work in mental health, also called psychiatric social work, is a process where an individual in a setting is helped to attain freedom from overlapping internal and external problems (social and economic situations, family and other relationships, the physical and organizational environment, psychiatric symptoms, etc.). It aims for harmony, quality of life, self-actualization and personal adaptation across all systems. Psychiatric social workers are mental health professionals that can assist patients and their family members in coping with both mental health issues and various economic or social problems caused by mental illness or psychiatric dysfunctions and to attain improved mental health and well-being. They are vital members of the treatment teams in Departments of Psychiatry and Behavioral Sciences in hospitals. They are employed in both outpatient and inpatient settings of a hospital, nursing homes, state and local governments, substance use clinics, correctional facilities, health care services, private practice, etc.[79]
In the United States, social workers provide most of the mental health services. According to government sources, 60 percent of mental health professionals are
Mental health social workers in Japan have professional knowledge of health and welfare and skills essential for person's well-being. Their social work training enables them as a professional to carry out Consultation assistance for mental disabilities and their social reintegration; Consultation regarding the rehabilitation of the victims; Advice and guidance for post-discharge residence and re-employment after hospitalized care, for major life events in regular life, money and self-management and other relevant matters to equip them to adapt in daily life. Social workers provide individual home visits for mentally ill and do welfare services available, with specialized training a range of procedural services are coordinated for home, workplace and school. In an administrative relationship, Psychiatric social workers provides consultation, leadership, conflict management and work direction. Psychiatric social workers who provides assessment and psychosocial interventions function as a clinician, counselor and municipal staff of the health centers.[81]
Risk factors and causes of mental health problems
There are many things that can contribute to mental health problems, including biological factors, genetic factors, life experiences (such as psychological trauma or abuse), and a family history of mental health problems.[82]
Biological factors
According to the National Institute of Health Curriculum Supplement Series book, most scientists believe that changes in neurotransmitters can cause mental illnesses. In the section "The Biology of Mental Illnesses" the issue is explained in detail, "...there may be disruptions in the neurotransmitters dopamine, glutamate, and norepinephrine in individuals who have schizophrenia". [83]
Demographic factors
Gender, age, ethnicity, life expectancy, longevity, population density, and community diversity are all demographic characteristics that can increase the risk and severity of mental disorders.[84] Existing evidence demonstrates that the female gender is connected with an elevated risk of depression at differerent phases of life, commencing in adolescence in different contexts.[85][86] Females, for example, have a higher risk of anxiety[87] and eating disorders,[88] whereas males have a higher chance of substance abuse and behavioural and developmental issues.[89] This does not imply that women are less likely to suffer from developmental disorders such autism spectrum disorder, attention deficit hyperactivity disorder, Tourette syndrome, or early-onset schizophrenia. Ethnicity and ethnic heterogeneity have also been identified as risk factors for the prevalence of mental disorders, with minority groups being at a higher risk due to discrimination and exclusion.[84]
Unemployment has been shown to hurt an individual's emotional well-being, self-esteem, and more broadly their mental health. Increasing unemployment has been shown to have a significant impact on mental health, predominantly depressive disorders.[90] This is an important consideration when reviewing the triggers for mental health disorders in any population survey.[91] According to a 2009 meta-analysis by Paul and Moser, countries with high income inequality and poor unemployment protections experience worse mental health outcomes among the unemployed.[92]
Unhappily married couples suffer 3–25 times the risk of developing clinical depression.[95][96][97]
The World Mental Health survey initiative has suggested a plan for countries to redesign their mental health care systems to best allocate resources. "A first step is documentation of services being used and the extent and nature of unmet treatment needs. A second step could be to do a cross-national comparison of service use and unmet needs in countries with different mental health care systems. Such comparisons can help to uncover optimum financing, national policies, and delivery systems for mental health care."[This quote needs a citation]
Knowledge of how to provide effective emotional mental health care has become imperative worldwide. Unfortunately, most countries have insufficient data to guide decisions, absent or competing visions for resources, and near-constant pressures to cut insurance and entitlements. WMH surveys were done in Africa (
The coordinated surveys on emotional mental health disorders, their severity, and treatments were implemented in the aforementioned countries. These surveys assessed the frequency, types, and adequacy of mental health service use in 17 countries in which WMH surveys are complete. The WMH also examined unmet needs for treatment in strata defined by the seriousness of mental disorders. Their research showed that "the number of respondents using any 12-month mental health service was generally lower in developing than in developed countries, and the proportion receiving services tended to correspond to countries' percentages of gross domestic product spent on health care". "High levels of unmet need worldwide are not surprising, since WHO Project
Stress
The Centre for Addiction and Mental Health discuss how a certain amount of stress is a normal part of daily life. Small doses of stress help people meet deadlines, be prepared for presentations, be productive and arrive on time for important events. However, long-term stress can become harmful. When stress becomes overwhelming and prolonged, the risks for mental health problems and medical problems increase."[98] Also on that note, some studies have found language to deteriorate mental health and even harm humans.[99]
Poverty
A psychological study has been conducted by four scientists during inaugural Convention of Psychological Science. The results find that people who thrive with financial stability or fall under low socioeconomic status (SES) tend to perform worse cognitively due to external pressure imposed upon them. The research found that stressors such as low income, inadequate health care, discrimination, and exposure to criminal activities all contribute to mental disorders. This study also found that children exposed to poverty-stricken environments have slower cognitive thinking.[100] It is seen that children perform better under the care of their parents and that children tend to adopt speaking language at a younger age. Since being in poverty from childhood is more harmful than it is for an adult, it is seen that children in poor households tend to fall behind in certain cognitive abilities compared to other average families.[101]
For a child to grow up emotionally healthy, the children under three need "A strong, reliable primary caregiver who provides consistent and unconditional love, guidance, and support. Safe, predictable, stable environments. Ten to 20 hours each week of harmonious, reciprocal interactions. This process, known as attunement, is most crucial during the first 6–24 months of infants' lives and helps them develop a wider range of healthy emotions, including gratitude, forgiveness, and empathy. Enrichment through personalized, increasingly complex activities".[citation needed] In one survey, 67% of children from disadvantaged inner cities said they had witnessed a serious assault, and 33% reported witnessing a homicide.[102] 51% of fifth graders from New Orleans (median income for a household: $27,133) have been found to be victims of violence, compared to 32% in Washington, DC (mean income for a household: $40,127).[103] Studies have shown that poverty changes the personalities of children who live in it. The Great Smoky Mountains Study was a ten-year study that was able to demonstrate this. During the study, about one-quarter of the families saw a dramatic and unexpected increase in income. The study showed that among these children, instances of behavioral and emotional disorders decreased, and conscientiousness and agreeableness increased.[104]Environmental factors

The
An additional aspect to consider is the detrimental impact climate change can have on green or blue natural spaces, which in themselves have been proven to have beneficial impact on mental health.[108][109] Impacts of anthropogenic climate change, such as freshwater pollution or deforestation, degrade these landscapes and reduce public access.[110] Even when the green and blue spaces are intact, access to them is not equal across society, which is an issue of environmental justice and economic inequality.[111]
Mental health outcomes have been measured in several studies. These use indicators such as psychiatric hospital admissions, mortality, self-harm and suicide rates. People with pre-existing mental illness, Indigenous peoples, migrants and refugees, and children and adolescents are all vulnerable. The emotional responses to the threat of climate change can include eco-anxiety, ecological grief and eco-anger.[112][113] Such emotions can be rational responses to the degradation of the natural world and lead to adaptive action.[114]
Assessing the exact mental health effects of climate change is difficult; increases in heat extremes pose risks to mental health which can manifest themselves in increased mental health-related hospital admissions and suicidality.[115]: 9Prevention and promotion
"The terms mental health promotion and prevention have often been confused. Promotion is defined as intervening to optimize positive mental health by addressing determinants of positive mental health (i.e.
In order to improve mental health, the root of the issue has to be resolved. "Prevention emphasizes the avoidance of risk factors; promotion aims to enhance an individual's ability to achieve a positive sense of
Mental health is conventionally defined as a hybrid of the absence of a
Prevention of a disorder at a young age may significantly decrease the chances that a child will have a disorder later in life, and shall be the most efficient and effective measure from a public health perspective.[124] Prevention may require the regular consultation of a physician for at least twice a year to detect any signs that reveal any mental health concerns.
Additionally, social media is becoming a resource for prevention. In 2004, the Mental Health Services Act[125] began to fund marketing initiatives to educate the public on mental health. This California-based project is working to combat the negative perception with mental health and reduce the stigma associated with it. While social media can benefit mental health, it can also lead to deterioration if not managed properly.[126] Limiting social media intake is beneficial.[127]
Studies report that patients in mental health care who can access and read their
Furthermore, recent studies have shown that social media is an effective way to draw attention to mental health issues. By collecting data from Twitter, researchers found that social media presence is heightened after an event relating to behavioral health occurs.[134] Researchers continue to find effective ways to use social media to bring more awareness to mental health issues through online campaigns in other sites such as Facebook and Instagram.[135]
Mental health care navigation helps to guide patients and families through the fragmented, often confusing mental health industries. Care navigators work closely with patients and families through discussion and collaboration to provide information on best therapies as well as referrals to practitioners and facilities specializing in particular forms of emotional improvement. The difference between therapy and care navigation is that the care navigation process provides information and directs patients to therapy rather than providing therapy. Still, care navigators may offer diagnosis and treatment planning. Though many care navigators are also trained therapists and doctors. Care navigation is the link between the patient and the below therapies. A clear recognition that mental health requires medical intervention was demonstrated in a study by Kessler et al. of the prevalence and treatment of mental disorders from 1990 to 2003 in the United States. Despite the prevalence of mental health disorders remaining unchanged during this period, the number of patients seeking treatment for mental disorders increased threefold.[136]
Methods
Pharmacotherapy
Pharmacotherapy is a therapy that uses pharmaceutical drugs. Pharmacotherapy is used in the treatment of mental illness through the use of antidepressants, benzodiazepines, and the use of elements such as lithium. It can only be prescribed by a medical professional trained in the field of Psychiatry.
Physical activity
Physical exercise can improve mental and physical health. Playing sports, walking, cycling, or doing any form of physical activity trigger the production of various hormones, sometimes including endorphins, which can elevate a person's mood.[137]
Studies have shown that in some cases, physical activity can have the same impact as antidepressants when treating depression and anxiety.[138]
Moreover, cessation of physical exercise may have adverse effects on some mental health conditions, such as depression and anxiety. This could lead to different negative outcomes such as obesity, skewed body image and many health risks associated with mental illnesses.[139] Exercise can improve mental health but it should not be used as an alternative to therapy.[140]
Activity therapies
Activity therapies also called recreation therapy and occupational therapy, promote healing through active engagement. An example of occupational therapy would be promoting an activity that improves daily life, such as self-care or improving hobbies.[141]
Each of these therapies have proven to improve mental health and have resulted in healthier, happier individuals. In recent years, for example, coloring has been recognized as an activity that has been proven to significantly lower the levels of depressive symptoms and anxiety in many studies.[142]
Expressive therapies
Psychotherapy
Psychotherapy is the general term for the scientific based treatment of mental health issues based on modern medicine. It includes a number of schools, such as gestalt therapy, psychoanalysis, cognitive behavioral therapy, psychedelic therapy, transpersonal psychology/psychotherapy, and dialectical behavioral therapy.
Self-compassion
According to Neff, self-compassion consists of three main positive components and their negative counterparts: Self-Kindness versus Self-Judgment, Common Humanity versus Isolation and Mindfulness versus Over-Identification.[145] Furthermore, there is evidence from a study by Shin & Lin suggesting specific components of self-compassion can predict specific dimensions of positive mental health (emotional, social, and psychological well-being).[146]
Social-emotional learning
The Collaborative for academic, social, emotional learning (CASEL) addresses five broad and interrelated areas of competence and highlights examples for each: self-awareness, self-management, social awareness, relationship skills, and responsible decision-making.
Meditation
The practice of mindfulness meditation has several potential mental health benefits, such as bringing about reductions in depression, anxiety and stress.[149][150][151][152] Mindfulness meditation may also be effective in treating substance use disorders.[153]
Lucid Dreaming
Mental fitness
Mental fitness is a mental health movement that encourages people to intentionally regulate and maintain their emotional wellbeing through friendship, regular human contact, and activities that include meditation, calming exercises, aerobic exercise, mindfulness, having a routine and maintaining adequate sleep. Mental fitness is intended to build resilience against every-day mental and potentially physical health challenges to prevent an escalation of anxiety, depression, and suicidal ideation.[156] This can help people, including older adults with health challenges, to more effectively cope with the escalation of those feelings if they occur.[157]
Spiritual counseling
Spiritual counsellors meet with people in need to offer comfort and support and to help them gain a better understanding of their issues and develop a problem-solving relation with spirituality. These types of counselors deliver care based on spiritual, psychological and theological principles.[158]
Laws and public health policies
There are many factors that influence mental health including:
- Mental illness, disability, and suicideare ultimately the result of a combination of biology, environment, and access to and utilization of mental health treatment.
- Public health policies can influence access and utilization, which subsequently may improve mental health and help to progress the negative consequences of depression and its associated disability.
United States
Emotional mental illnesses should be a particular concern in the United States since the U.S. has the highest annual prevalence rates (26 percent) for mental illnesses among a comparison of 14 developing and developed countries.[159] While approximately 80 percent of all people in the United States with a mental disorder eventually receive some form of treatment, on average persons do not access care until nearly a decade following the development of their illness, and less than one-third of people who seek help receive minimally adequate care.[160] The government offers everyone programs and services, but veterans receive the most help, there is certain eligibility criteria that has to be met.[161]
Policies
Mental health policies in the United States have experienced four major reforms: the American asylum movement led by
In 1843, Dorothea Dix submitted a Memorial to the Legislature of Massachusetts, describing the abusive treatment and horrible conditions received by the mentally ill patients in jails, cages, and almshouses. She revealed in her Memorial: "I proceed, gentlemen, briefly to call your attention to the present state of insane persons confined within this Commonwealth, in cages, closets, cellars, stalls, pens! Chained, naked, beaten with rods, and lashed into obedience...."[163] Many asylums were built in that period, with high fences or walls separating the patients from other community members and strict rules regarding the entrance and exit. In 1866, a recommendation came to the New York State Legislature to establish a separate asylum for chronic mentally ill patients. Some hospitals placed the chronic patients into separate wings or wards, or different buildings.[164]
In A Mind That Found Itself (1908) Clifford Whittingham Beers described the humiliating treatment he received and the deplorable conditions in the mental hospital.[165] One year later, the National Committee for Mental Hygiene (NCMH) was founded by a small group of reform-minded scholars and scientists—including Beers himself—which marked the beginning of the "mental hygiene" movement. The movement emphasized the importance of childhood prevention. World War I catalyzed this idea with an additional emphasis on the impact of maladjustment, which convinced the hygienists that prevention was the only practical approach to handle mental health issues.[166] However, prevention was not successful, especially for chronic illness; the condemnable conditions in the hospitals were even more prevalent, especially under the pressure of the increasing number of chronically ill and the influence of the depression.[162]
In 1961, the Joint Commission on Mental Health published a report called Action for Mental Health, whose goal was for community clinic care to take on the burden of prevention and early intervention of the mental illness, therefore to leave space in the hospitals for severe and chronic patients. The court started to rule in favor of the patients' will on whether they should be forced to treatment. By 1977, 650 community mental health centers were built to cover 43 percent of the population and serve 1.9 million individuals a year, and the lengths of treatment decreased from 6 months to only 23 days.
After realizing that simply changing the location of mental health care from the state hospitals to nursing houses was insufficient to implement the idea of
However, several critics maintain that deinstitutionalization has, from a mental health point of view, been a thoroughgoing failure. The seriously mentally ill are either homeless, or in prison; in either case (especially the latter), they are getting little or no mental health care. This failure is attributed to a number of reasons over which there is some degree of contention, although there is general agreement that community support programs have been ineffective at best, due to a lack of funding.[168]
The 2011 National Prevention Strategy included mental and emotional well-being, with recommendations including better parenting and early intervention programs, which increase the likelihood of prevention programs being included in future US mental health policies.[121][page needed] The NIMH is researching only suicide and HIV/AIDS prevention, but the National Prevention Strategy could lead to it focusing more broadly on longitudinal prevention studies.[170][failed verification]
In 2013, United States Representative
See also
- Abnormal psychology
- Emotional resilience
- Ethnopsychopharmacology
- Mental environment
- Mental health day
- Mental health during the COVID-19 pandemic
- Mental health first aid
- Mental health in education
- Mental health in the workplace
- Mental health of Asian Americans
- Self-help groups for mental health
- Social determinants of mental health
- Social stigma
- Suicide awareness
- Telemental health
- World Mental Health Day
- Well-being
References
- ^ "Health and Well-Being". World Health Organization. Retrieved 2023-08-09.
- ^ a b "About Mental Health". www.cdc.gov. 2021-11-23. Retrieved 2022-04-11.
- ^ "The world health report 2001 – Mental Health: New Understanding, New Hope" (PDF). WHO. Retrieved 4 May 2014.
- OCLC 639574840.[page needed]
- ^ "Mental Health". medlineplus.gov. Retrieved 2019-11-20.
- ^ "Mental Health". medlineplus.gov. Retrieved 2021-11-19.
- ^ Public Health Agency of Canada (2020-10-28). "Public Health Agency of Canada". www.canada.ca. Retrieved 2021-10-02.
- PMID 26038353.
- PMID 28866712.
- ^ Institute of Health Metrics and Evaluation. Global Health Data Exchange (GHDx), (https://vizhub.healthdata.org/gbd-results/, accessed 14 May 2022.
- PMID 20040234.
- PMID 16684739.
- ISBN 978-1-118-62539-2
- ^ "ICD-11". icd.who.int. Retrieved 2022-01-18.
- ^ PMID 23737408.
- PMID 31569326.
- ^ "What Is the Difference Between Psychologists, Psychiatrists and Social Workers?". www.apa.org. Retrieved 2021-11-19.
- ISBN 978-1-4411-7140-5.
- ^ a b Mandell W (1995). "Origins of Mental Health, The Realization of an Idea". Johns Hopkins Bloomberg School of Public Health. Baltimore, MD: Johns Hopkins University. Retrieved 9 June 2015.
- ^ "Isaac Ray Award". www.psychiatry.org. American Psychiatric Association. Retrieved 27 October 2017.
- ^ a b c "A Brief History of Mental Illness and the U.S. Mental Health Care System". www.uniteforsight.org. Archived from the original on 2020-06-17. Retrieved 2020-05-11.
- ^ a b c Barlow, D.H., Durand, V.M., Steward, S.H. (2009). Abnormal psychology: An integrative approach (Second Canadian Edition). Toronto: Nelson. p. 16
- PMID 20838510.
- ^ Peck A (2013). "Mental Health America – Origins". The Social Welfare History Project. Retrieved 9 June 2015.
- ^ a b "About Us". Archived from the original on 2007-04-09. Retrieved 2007-06-01.
- ^ PMID 18560478.
- ISBN 978-0-7099-1481-5.
- ^ Wilkie JS. "Hygiene". Hygiene - Evolving Ideas of Hygiene, Theories of Contagion, Public Hygiene - Encyclopedia of Children and Childhood in History and Society. Encyclopedia of Children and Childhood in History and Society.
- . ICPSR 26164.
- PMID 21143545.
- ^ S2CID 23328647.
- ^ PMID 30410452.
- S2CID 199547608.
- ^ "Mental Illness - National Institute of Mental Health (NIMH)". National Institute of Mental Health. March 2023. Retrieved January 5, 2024.
- ^ "Mental disorders". World Health Organization. June 8, 2022. Retrieved January 5, 2024.
- PMID 32644504, retrieved 2024-01-05
- ^ "Suicide prevention". World Health Organization. Retrieved January 5, 2024.
- ^ "Who". Mental illness.
- PMID 20158541.
- ^ a b c d Richards K, Campenni C, Muse-Burke J (July 2010). "Self-care and Well-being in Mental Health Professionals: The Mediating Effects of Self-awareness and Mindfulnes". Journal of Mental Health Counseling. 32 (3): 247–264. .
- S2CID 148951912.
- ^ S2CID 2961978.
- ISBN 978-1-4787-2259-5.
- .
- .
- ^ S2CID 16022037.
- PMID 25769861.
- PMID 19558444.
- S2CID 20788777.
- .
- PMID 26990960.
- ^ a b c d "Adolescent mental health". www.who.int. Retrieved 2021-07-08.
- ^ "Mental Illness". National Institute of Mental Health. Retrieved 13 September 2023.
- ^ "Mental health statistics: children and young people". Mental Health Foundation. 2015-10-26. Retrieved 2021-10-05.
- S2CID 3801878.
- S2CID 13713247.
- ^ PMID 26250791.
- ^ PMID 19432384.
- ^ PMID 1772159.
- ^ PMID 16242595.
- ^ PMID 28617002.
- ^ S2CID 52334254.
- ^ PMID 29069252.
- ^ "The U.S. Mainland: Growth and Resistance | Japanese | Immigration and Relocation in U.S. History | Classroom Materials at the Library of Congress | Library of Congress". Library of Congress, Washington, D.C. 20540 USA. Retrieved 2023-12-07.
- ISBN 978-0-415-16875-5.
- ^ Office of the Deputy Prime Minister – Social Exclusion Unit (2004). "Factsheet 1: Stigma and Discrimination on Mental Health Grounds" (PDF). Archived from the original (PDF) on 2008-12-29.
- ISBN 978-1-136-88193-0.
- PMID 25259732.
- ^ Royal College of Psychiatrists: Changing Minds.
- ^ Blakemore E (29 April 2019). "A play that hopes to smash the stigma surrounding mental illness". The Washington Post. Retrieved 23 June 2020.
- ^ Myrow R (2 May 2019). "'Manic Monologues' Seeks to Disrupt the Stigma Around Mental Illness". KQED. Retrieved 23 June 2020.
- ^ "NAMI Presents: Cure Stigma". NAMI Presents: Cure Stigma. Archived from the original on 2019-07-03. Retrieved 2018-09-15.
- ISBN 978-1-55798-624-5.
- ^ "Religious Trauma Syndrome". Recovering from Religion. Retrieved 2018-12-08.
- ^ Merelli A (August 2018). "Jeff Sessions' new task force puts freedom of religion first". Quartz. Retrieved 2018-12-08.
- ^ "How culture shapes your mind—and your mental illness - The Boston Globe". BostonGlobe.com. Retrieved 2018-12-08.
- ^ a b American Occupational Therapy Association. (2020). Occupational therapy practice framework: Domain and process (4th ed.). American Journal of Occupational Therapy, 74 (Supplement 2). doi.org/10.5014/ajot.2020.74S2001
- ^ Health A. "The Power of Community Support in Mental Health Recovery". amahahealth.com.
- ISBN 978-93-5150-116-9.[page needed]
- ^ National Association of Social Workers, 2011
- ^ "精神保健福祉士の受験資格を取得するための養成課程" [Psychiatric Social Worker Training Course]. Japan College of Social Work (in Japanese). Archived from the original on 2017-10-26. Retrieved 2016-02-10.
- ^ "What Is Mental Health? | MentalHealth.gov". www.mentalhealth.gov. Retrieved 2022-09-22.
- ^ Information about Mental Illness and the Brain. National Institutes of Health (US). 2007.
- ^ PMID 29580610.
- S2CID 1101013, retrieved 2023-09-27
- PMID 21194754.
- PMID 22781489.
- PMID 33834377.
- PMID 25678403.
- PMID 27685996.
- .
- ^ "The toll of job loss". www.apa.org. Retrieved 2023-11-26.
- ^ "The World Mental Health Survey Initiative". Harvard Medical School. Retrieved 23 January 2016.
- PMID 17826169.
- ^ Tatiana D. Gray, Matt Hawrilenko, and James V. Cordova (2019). "Randomized Controlled Trial of the Marriage Checkup: Depression Outcomes" (PDF).
{{cite web}}: CS1 maint: multiple names: authors list (link) - PMID 25032063.
- S2CID 165116052.
- ^ "20131 Stress". CAMH. Retrieved 2020-11-13.
- ^ Vey JS, Love H (2020-07-13). "Recognizing that words have the power to harm, we commit to using more just language to describe places". Brookings. Retrieved 2021-05-09.
- ^ Sleek S (31 August 2015). "How Poverty Affects the Brain and Behavior". APS Observer. 28 (7). Archived from the original on 4 December 2019. Retrieved 4 December 2019.
- PMID 18810850.
- S2CID 28660040.
- PMID 8488211.; and, Richters, J.E., & Martinez, P. (1993).
- ^ "The remarkable thing that happens to poor kids when you give their parents a little money". The Washington Post. Archived from the original on 9 October 2015. Retrieved 8 October 2015.
- PMID 21553952.
- ^ S2CID 22561555.
- ^ PMID 33922573.
 Text was copied from this source, which is available under a Creative Commons Attribution 4.0 International License
Text was copied from this source, which is available under a Creative Commons Attribution 4.0 International License - ISSN 0272-4944.
- PMID 24320055.
- S2CID 255467995.
- PMID 28809798.
- ISBN 978-0-19-762267-4.
- ISBN 978-3-031-08430-0.
- S2CID 236307729.
- S2CID 239046862.
- ^ a b "Promotion & Prevention". youth.gov. Retrieved 2020-11-17.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ Miles, J., Espiritu, R. C., Horen, N. M., Sebian, J., & Waetzig, E. (2010). Washington, DC: Georgetown University, Center for Children and Human Development, National Technical Assistance Center for Children's Mental Health
- PMID 20966366.
- ^ "The Benefits of Yoga". American Osteopathic Association. Retrieved 2022-05-02.
- ^ "Mental Health Support". healthhelpchat.com. Retrieved 2023-12-23.
- ^ a b National Prevention Council (16 June 2011), National Prevention Strategy (PDF), Washington, DC: U.S. Department of Health and Human Services, Office of the Surgeon General, archived from the original (PDF) on 4 October 2011
- PMID 25009931.
- ^ "Your Staff's Mental Health Is a Workplace Safety Issue - Humanengineers". Humanengineers. 2017-06-20. Archived from the original on 2018-01-12. Retrieved 2018-01-11.
- S2CID 23548727.
- PMID 23488486.
- ^ "Six Ways Social Media Negatively Affects Your Mental Health". 2019-10-10. Archived from the original on 2022-05-12. Retrieved 2020-04-20.
- ^ "Here's How to Look After Your Mental Health". 2020-04-20. Retrieved 2020-04-20.
- PMID 34904956.
- PMID 33760088.
- S2CID 199000133.
- S2CID 211121648.
- S2CID 232367133.
- S2CID 234499337.
- PMID 27707822.
- PMID 32642480.
- PMID 15958807.
- S2CID 51965322.
- S2CID 24320503.
- PMID 28625704.
- ISBN 978-0-357-13679-9.
- ^ "Occupational Therapy - Adults". The Interprofessional Clinic. Archived from the original on 2021-04-16. Retrieved 2021-03-16.
- S2CID 149346431.
- hdl:10344/3362.
- ^ The National Institute for Health and Care Excellence (NICE), Dramatherapy in Early Intervention in Psychosis, March 2019 https://www.nice.org.uk/sharedlearning/dramatherapy-in-early-intervention-in-psychosis
- S2CID 202569236.
- S2CID 52191018.
- ^ "SEL: What Are the Core Competence Areas and Where are they Promoted?". casel.org. Retrieved 2020-11-14.
- .
- PMID 24395196.
- S2CID 503591.
- PMID 25053754.
- PMID 23796855.
- S2CID 34990668.
- ^ Schadow, C., Schredl, M., Rieger, J., & Göritz, A. S. (2018). The relationship between lucid dream frequency and sleep quality: Two cross-sectional studies. Int. J. Dream Res, 11, 154-159.
- ^ Spoormaker, V. I., & Van Den Bout, J. (2006). Lucid dreaming treatment for nightmares: a pilot study. Psychotherapy and psychosomatics, 75(6), 389-394.
- S2CID 261694577.
- ^ Walkadean C (22 June 2020). "Mental fitness - a gamechanger". Gotcha4Life mental health and suicide prevention. Archived from the original on 4 July 2020. Retrieved 3 July 2020.
- PMID 21480226.
- PMID 15173149.
- PMID 15939838.
- PMID 28083443.
- ^ a b c U.S. Public Health Service (1999). "Overview of Mental Health Services". Mental Health: A Report of the Surgeon General. Archived from the original on 11 February 2012. Retrieved 19 February 2012.
- PMID 16551962.
- PMID 2691669.
- ^ Beers CW (8 April 2004) [1908]. A Mind That Found Itself: An Autobiography. Project Gutenberg.
- S2CID 44384151.
- ^ PMID 1743659.
- ^ ISBN 978-0-471-16161-5.
- ^ a b Koyanagi C (August 2007), Learning From History: Deinstitutionalization of People with Mental Illness As Precursor to Long-Term Care Reform (PDF), Menlo Park, CA: Kaiser Family Foundation, pp. 1–22, archived from the original (PDF) on 2018-11-29, retrieved 2016-01-24
- ^ "Prevention of Mental Disorders". National Institute of Mental Health. Archived from the original on 5 July 2015. Retrieved 7 August 2015.
- ^ Murphy T (2016-07-14). "Actions - H.R.2646 - 114th Congress (2015-2016): Helping Families in Mental Health Crisis Act of 2016". www.congress.gov. Retrieved 2021-05-06.
Further reading
External links
 Quotations related to Mental health at Wikiquote
Quotations related to Mental health at Wikiquote Media related to Mental health at Wikimedia Commons
Media related to Mental health at Wikimedia Commons- Mental Health by WHO
- The Public Health Agency of Canada
- "Mental health and substance abuse". WHO Regional Office for the Eastern Mediterranean.
- National Institute of Mental Health (United States)
- Health-EU Portal Mental Health in the EU
- Mental Health Department of Health (United Kingdom)
