Methadone
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Dolophine, Methadose, Methatab,[3] others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682134 |
| License data | |
| Pregnancy category |
|
| Addiction liability | High[4] |
| Routes of administration | By mouth, intravenous, insufflation, sublingual, rectal |
| Drug class | Opioid |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 15-20% subcutaneous[6] 100% intravenous[6] |
| Protein binding | 85–90%[6] |
| Metabolism | Liver (CYP3A4, CYP2B6 and CYP2D6-mediated)[6][8] |
| Onset of action | Rapid[7] |
| Elimination half-life | 15 to 55 hours[8] |
| Duration of action | Single dose: 4–8 h Prolonged use: • Withdrawal prevention: 1–2 days[7] • Pain relief: 8–12 hours[7][9] |
| Excretion | Urine, faeces[8] |
| Identifiers | |
| |
JSmol) | |
| Chirality | Racemic mixture |
| |
| |
| | |
Methadone, sold under the brand names Dolophine and Methadose among others, is a synthetic
Side effects are similar to those of other opioids.
Methadone was developed in Germany in the late 1930s by Gustav Ehrhart and Max Bockmühl.[19][20] It was approved for use as an analgesic in the United States in 1947, and has been used in the treatment of addiction since the 1960s.[7][21] It is on the World Health Organization's List of Essential Medicines.[22]
Medical uses
Opioid addiction
Methadone is used for the treatment of opioid use disorder.[23] It may be used as maintenance therapy or in shorter periods to manage opioid withdrawal symptoms. Its use for the treatment of addiction is usually strictly regulated. In the US, outpatient treatment programs must be certified by the federal Substance Abuse and Mental Health Services Administration (SAMHSA) and registered by the Drug Enforcement Administration (DEA) in order to prescribe methadone for opioid addiction.
A 2009
Treatment of opioid-dependent persons with methadone follows one of two routes: maintenance or withdrawal management.[25] Methadone maintenance therapy (MMT) usually takes place in outpatient settings. It is usually prescribed as a single daily dose medication for those who wish to abstain from illicit opioid use. Treatment models for MMT differ. It is not uncommon for treatment recipients to be administered methadone in a specialized clinic, where they are observed for around 15–20 minutes post-dosing, to reduce the risk of diversion of medication.[26]
The duration of methadone treatment programs ranges from a few months to years. Given opioid dependence is characteristically a chronic relapsing/remitting disorder, MMT may be lifelong. The length of time a person remains in treatment depends on a number of factors. While starting doses may be adjusted based on the amount of opioids reportedly used, most clinical guidelines suggest doses start low (e.g., at doses not exceeding 40 mg daily) and are incremented gradually.[12][27] It has been found that doses of 40 mg per day were sufficient to help control the withdrawal symptoms but not enough to curb the cravings for the drug. Doses of 80 to 100 mg per day have shown higher rates of success in patients and less illicit heroin use during the maintenance therapy.[10] However, higher doses do put a patient more at risk for overdose than a moderately low dose (e.g. 20 mg/day).[14]
Methadone maintenance has been shown to reduce the transmission of bloodborne viruses associated with opioid injection, such as hepatitis B and C, and/or HIV.[12] The principal goals of methadone maintenance are to relieve opioid cravings, suppress the abstinence syndrome, and block the euphoric effects associated with opioids.
Chronic methadone dosing will eventually lead to neuroadaptation, characterised by a syndrome of tolerance and withdrawal (dependence). However, when used correctly in treatment, maintenance therapy has been found to be medically safe, non-sedating, and can provide a slow recovery from opioid addiction.[12] Methadone has been widely used for pregnant women addicted to opioids.[12]
Pain
Methadone is used as an analgesic in chronic pain, often in rotation with other opioids.[28][29] Due to its activity at the NMDA receptor, it may be more effective against neuropathic pain; for the same reason, tolerance to the analgesic effects may be less than that of other opioids.[30][31]
Adverse effects

Adverse effects of methadone include:[33]
- Sedation
- Constipation[34][35]
- Flushing[35]
- Perspiration[35]
- Heat intolerance
- Dizziness[34][36][37] or fainting[34][36][37]
- Weakness[35]
- Chronic fatigue, sleepiness[35]and exhaustion
- Sleep problems such as drowsiness,[34]
- Constricted pupils
- Dry mouth[34][35]
- Nausea[34][35] and vomiting[34][35]
- Low blood pressure
- Headache[35]
- Heart problems such as chest pain[34][36] or fast/pounding heartbeat[34][36][37]
- Respiratory problems such as trouble breathing,[34][36] slow or shallow breathing (hypoventilation),[34][36] light-headedness,[34][36][37] or fainting[34][36]
- Weight gain[35]
- Memory loss
- Itching
- Difficulty urinating[35]
- Swelling of the hands, arms, feet, and legs[35]
- Mood changes,[35]euphoria, disorientation
- Blurred vision[35]
- Decreased
- Missed menstrual periods[35]
- Skin rash
- Central sleep apnea
Withdrawal symptoms
Methadone withdrawal symptoms are reported as being significantly more protracted than withdrawal from opioids with shorter half-lives.
When used for opioid maintenance therapy, Methadone is generally administered as an oral liquid. Methadone has been implicated in contributing to significant tooth decay. Methadone causes dry mouth, reducing the protective role of saliva in preventing decay. Other putative mechanisms of methadone-related tooth decay include craving for carbohydrates related to opioids, poor dental care, and general decrease in personal hygiene. These factors, combined with sedation, have been linked to the causation of extensive dental damage.[39][40]
Physical symptoms
- Lightheadedness[41]
- Mydriasis (dilated pupils)[41]
- Photophobia (sensitivity to light)
- Hyperventilation syndrome (breathing that is too fast/deep)
- Runny nose[42]
- Yawning
- Sneezing[42]
- Nausea,[41][42] vomiting,[41][42] and diarrhea[41]
- Fever[42]
- Sweating[41]
- Chills[42]
- Tremors[41][42]
- Akathisia (restlessness)
- Tachycardia (fast heartbeat)[42]
- Aches[41] and pains, often in the joints or legs
- Elevated pain sensitivity
- Blood pressure that is too high (hypertension, may cause a stroke)
Cognitive symptoms
- Suicidal ideation
- Susceptibility to cravings[41]
- Depression[41]
- Spontaneous orgasm
- Prolonged insomnia
- Delirium
- Auditory hallucinations
- Visual hallucinations
- Increased perception of odors (olfaction), real or imagined
- Marked increase in sex drive
- Agitation
- Anxiety[41]
- Panic disorder
- Nervousness[41]
- Paranoia
- Delusions
- Apathy
- Anorexia (symptom)
Black box warning
Methadone has the following US FDA
- Risk of addiction and abuse
- Potentially fatal respiratory depression
- Lethal overdose in accidental ingestion
- QT prolongation[44]
- Neonatal opioid withdrawal syndrome in children of pregnant women
- CYP450 drug interactions
- Risks when used with benzodiazepines and other CNS depressants, including alcohol.
- A certified opioid treatment program is required under federal law (42 CFR 8.12) when dispensing methadone for the treatment of opioid addiction.
Overdose
Most people who overdose on methadone show some of the following symptoms:
- Miosis (constricted pupils)[45]
- Vomiting[46]
- Spasms of the stomach and intestines[47]
- Hypoventilation (breathing that is too slow/shallow)[45]
- Drowsiness,[45]sleepiness, disorientation, sedation, unresponsiveness
- Skin that is cool, clammy (damp), and pale[45]
- Blue fingernails and lips[47]
- Limp muscles,[45] trouble staying awake, nausea
- Unconsciousness[45] and coma[45]
The respiratory depression of an overdose can be treated with naloxone.[42] Naloxone is preferred to the newer, longer-acting antagonist naltrexone. Despite methadone's much longer duration of action compared to either heroin and other shorter-acting agonists and the need for repeat doses of the antagonist naloxone, it is still used for overdose therapy. As naltrexone has a longer half-life, it is more difficult to titrate. If too large a dose of the opioid antagonist is given to a dependent person, it will result in withdrawal symptoms (possibly severe). When using naloxone, the naloxone will be quickly eliminated and the withdrawal will be short-lived. Doses of naltrexone take longer to be eliminated from the person's system. A common problem in treating methadone overdoses is that, given the short action of naloxone (versus the extremely longer-acting methadone), a dosage of naloxone given to a methadone-overdosed person will initially work to bring the person out of overdose, but once the naloxone wears off, if no further naloxone is administered, the person can go right back into overdose (based upon time and dosage of the methadone ingested).
Tolerance and dependence
As with other opioid medications, tolerance and dependence usually develop with repeated doses. There is some clinical evidence that tolerance to analgesia is less with methadone compared to other opioids; this may be due to its activity at the
Driving
Methadone treatment may impair driving ability.[49] Drug abusers had significantly more involvement in serious crashes than non-abusers in a study by the University of Queensland. In the study of a group of 220 drug abusers, most of them poly-drug abusers, 17 were involved in crashes killing people, compared with a control group of other people randomly selected having no involvement in fatal crashes.[50] However, there have been multiple studies verifying the ability of methadone maintenance patients to drive.[51] In the UK, persons who are prescribed oral methadone can continue to drive after they have satisfactorily completed an independent medical examination which will include a urine screen for drugs. The license will be issued for 12 months at a time and even then, only following a favourable assessment from their own doctor.[52] Individuals who are prescribed methadone for either IV or IM administration cannot drive in the UK, mainly due to the increased sedation effects that this route of use can cause.
Mortality
In the United States, deaths linked to methadone more than quadrupled in the five-year period between 1999 and 2004. According to the U.S. National Center for Health Statistics,
Although deaths from methadone are on the rise[needs update], methadone-associated deaths are not being caused primarily by methadone intended for methadone treatment programs, according to a panel of experts convened by the Substance Abuse and Mental Health Services Administration, which released a report titled "Methadone-Associated Mortality, Report of a National Assessment". The consensus report concludes that "although the data remains incomplete, National Assessment meeting participants concurred that methadone tablets or Diskets® distributed through channels other than opioid treatment programs most likely are the central factors in methadone-associated mortality."[55]
In 2006, the U.S. Food and Drug Administration issued a caution about methadone, titled "Methadone Use for Pain Control May Result in Death." The FDA also revised the drug's package insert. The change deleted previous information about the usual adult dosage. The Charleston Gazette reported, "The old language about the 'usual adult dose' was potentially deadly, according to pain specialists."[56]
Pharmacology
| Compound | Ki , in nM)
|
Ratios | ||||||
|---|---|---|---|---|---|---|---|---|
MOR
|
DOR
|
KOR
|
SERT | NET | NMDAR
|
M:D:K | SERT:NET | |
| Racemic methadone | 1.7 | 435 | 405 | 1,400 | 259 | 2,500–8,300 | 1:256:238 | 1:5 |
Dextromethadone
|
19.7 | 960 | 1,370 | 992 | 12,700 | 2,600–7,400 | 1:49:70 | 1:13 |
| Levomethadone | 0.945 | 371 | 1,860 | 14.1 | 702 | 2,800–3,400 | 1:393:1968 | 1:50 |
Methadone acts by binding to the
The metabolic half-life of methadone differs from its duration of action. The metabolic half-life is 8 to 59 hours (approximately 24 hours for opioid-tolerant people, and 55 hours in opioid-naive people), as opposed to a half-life of 1 to 5 hours for morphine.[14] The length of the half-life of methadone allows for exhibition of respiratory depressant effects for an extended duration of time in opioid-naive people.[14]
Mechanism of action
Metabolism
Methadone has a slow metabolism and very high fat solubility, making it longer lasting than morphine-based drugs. Methadone has a typical elimination half-life of 15 to 60 hours with a mean of around 22. However, metabolism rates vary greatly between individuals, up to a factor of 100,[61][62] ranging from as few as 4 hours to as many as 130 hours,[63] or even 190 hours.[64] This variability is apparently due to genetic variability in the production of the associated cytochrome enzymes CYP3A4, CYP2B6 and CYP2D6. Many substances can also induce, inhibit or compete with these enzymes further affecting (sometimes dangerously) methadone half-life. A longer half-life frequently allows for administration only once a day in opioid withdrawal management and maintenance programs. People who metabolize methadone rapidly, on the other hand, may require twice daily dosing to obtain sufficient symptom alleviation while avoiding excessive peaks and troughs in their blood concentrations and associated effects.[63] This can also allow lower total doses in some such people. The analgesic activity is shorter than the pharmacological half-life; dosing for pain control usually requires multiple doses per day normally dividing daily dosage for administration at 8 hour intervals.[65]
The main metabolic pathway involves N-demethylation by CYP3A4 in the liver and intestine to give
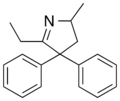
This inactive product, as well as the inactive 2-ethyl-5-methyl-3,3-diphenyl-1-pyrroline (EMDP), produced by a second N-demethylation, are detectable in the urine of those taking methadone.- Methadone and its two main metabolites
-
Methadone
-
EDDP
-
EDMP
Route of administration
The most common
Methadone is available in traditional pill,
Information leaflets included in packs of UK methadone tablets state that the tablets are for oral use only and that use by any other route can cause serious harm. In addition to this warning, additives have now been included in the tablet formulation to make the use of them by the IV route more difficult.[74]
Chemistry
Detection in biological fluids
Methadone and its major metabolite,
Conformation
The protonated form of methadone takes on an extended conformation, while the free base is more compact. In particular, it was found that there is an interaction between the tertiary amine and the carbonyl carbon of the ketone function (R3N ••• >C=O) that limits the molecule's conformation freedom, though the distance (291 pm by X-ray) is far too long to represent a true chemical bond. However, it does represent the initial trajectory of attack of an amine on a carbonyl group and was an important piece of experimental evidence for the proposal of the Bürgi–Dunitz angle for carbonyl addition reactions.[76]
History

Methadone was developed in 1937 in Germany by scientists working for
In the 1930s, pethidine (meperidine) went into production in Germany; however, production of methadone, then being developed under the designation Hoechst 10820, was not carried forward because of side effects discovered in the early research.[81] After the war, all German patents, trade names and research records were requisitioned and expropriated by the Allies. The records on the research work of the I.G. Farbenkonzern at the Farbwerke Hoechst were confiscated by the U.S. Department of Commerce Intelligence, investigated by a Technical Industrial Committee of the U.S. Department of State and then brought to the US.[77] The report published by the committee noted that while methadone itself was potentially addictive, it produced “considerably” less euphoria, sedation, and respiratory depression than morphine at equianalgesic doses and was thus interesting as a commercial drug. The same report also compared methadone to pethidine. German researchers reported that methadone was capable of producing strong morphine-like physical dependence, which is characterized by opioid withdrawal symptoms which are lesser in severity and intensity compared to morphine, but methadone was associated with a considerably prolonged or protracted withdrawal syndrome when compared to morphine.[48][77] Morphine produced higher rates of self-administration and reinforcing behaviour in both human and animal subjects when compared to both methadone and pethidine. In comparison to equianalgesic doses of pethidine (Demerol), methadone was shown to produce less euphoria, but higher rates of constipation, and roughly equal levels of respiratory depression and sedation.[77]
In the early 1950s, methadone (most times the racemic HCl salts mixture) was also investigated for use as an antitussive.[82]
Isomethadone, noracymethadol, LAAM, and normethadone were first developed in Germany, United Kingdom, Belgium, Austria, Canada, and the United States in the thirty or so years after the 1937 discovery of pethidine, the first synthetic opioid used in medicine. These synthetic opioids have increased length and depth of satiating any opiate cravings and generate very strong analgesic effects due to their long metabolic half-life and strong receptor affinity at the mu-opioid receptor sites. Therefore, they impart much of the satiating and anti-addictive effects of methadone by means of suppressing drug cravings.[83]
It was only in 1947 that the drug was given the generic name “methadone” by the Council on Pharmacy and Chemistry of the American Medical Association. Since the patent rights of the I.G. Farbenkonzern and Farbwerke Hoechst were no longer protected, each pharmaceutical company interested in the formula could buy the rights for the commercial production of methadone for just one dollar (MOLL 1990).
Methadone was introduced into the United States in 1947 by
Methadone was studied as a treatment for opioid addiction at the Addiction Research Center of the
Society and culture
Brand names
Brand names include Dolophine, Symoron, Amidone, Methadose, Physeptone, Metadon, Metadol, Metadol-D, Heptanon and Heptadon among others.
Economics
In the US, generic methadone tablets are inexpensive, with retail prices ranging from $0.25 to $2.50 per defined daily dose.[89]
Methadone maintenance clinics in the US may be covered by private insurances, Medicaid, or Medicare.[90] Medicare covers methadone under the prescription drug benefit, Medicare Part D, when it is prescribed for pain, but not when it is used for opioid dependence treatment because it cannot be dispensed in a retail pharmacy for this purpose.[91] In California methadone maintenance treatment is covered under the medical benefit. Patients' eligibility for methadone maintenance treatment is most often contingent on them being enrolled in substance abuse counseling. People on methadone maintenance in the US either have to pay cash or if covered by insurance must complete a pre-determined number of hours per month in therapeutic groups or counseling.[92] The United States Department of Veteran's Affairs (VA) Alcohol and Drug Dependence Rehabilitation Program offers methadone services to eligible veterans enrolled in the VA health care system.[93]
Regulation
United States and Canada
Methadone is a
Methadone clinics
In the United States, prescription of methadone requires intensive monitoring and must be obtained in-person from an Opioid Treatment Program—colloquially known as a 'methadone clinic'—when prescribed for opioid use disorder (OUD).[10] According to federal laws, methadone cannot be prescribed by a doctor and obtained from a pharmacy in order to treat addiction. Because of its long half-life, methadone is almost invariably prescribed to be taken in a single daily dose. At nearly all methadone clinics in the US, patients must visit a clinic to receive and take their dose under the supervision of a nurse. Both patients who are new to methadone treatment and high-risk patients—such as those who are using drugs and alcohol, including cannabis—must visit the clinic daily.[101][102]
Other countries
In
As of 2015, China had the largest methadone maintenance treatment program with over 250,000 people in over 650 clinics in 27 provinces.[105]
References
- ^ "CSD Entry METHAD01: (6R)-Dimethylamino-4,4-diphenyl-3-heptanone, L-Methadone". Cambridge Structural Database: Access Structures. Cambridge Crystallographic Data Centre. Retrieved 22 November 2020.
- .
- ^ https://www.medsafe.govt.nz/consumers/cmi/m/Methatabs.pdf
- ISBN 9781455701506.
- FDA. Retrieved 22 October 2023.
- ^ S2CID 25626479.
- ^ a b c d e f g h i j k l m n "Methadone Hydrochloride". The American Society of Health-System Pharmacists. Archived from the original on 23 December 2015. Retrieved 22 December 2015.
- ^ (PDF) from the original on 2 May 2014.
- ^ from the original on 5 September 2017.
- ^ PMID 10695444.
- S2CID 49300767.
- ^ PMID 11064485.
- ^ World Health Organization (2009). Clinical Guidelines for Withdrawal Management and Treatment of Drug Dependence in Closed Settings. Geneva: World Health Organization.
{{cite book}}: CS1 maint: date and year (link) - ^ PMID 21935293.
- ^ "Methadone". The Substance Abuse and Mental Health Services Administration. 16 June 2015. Retrieved 14 October 2020.
- ^ "Data table for Figure 1. Age-adjusted drug-poisoning and opioid-analgesic poisoning death rates: United States, 1999–2011" (PDF). CDC. Archived (PDF) from the original on 23 November 2015. Retrieved 22 December 2015.
- PMID 28033313.
- S2CID 207538295.
- ISBN 9780203633090. Archivedfrom the original on 23 December 2015.
- ISBN 9781506338248. Archivedfrom the original on 23 December 2015.
- ^ Kuehn, B. M. (2005). Methadone Treatment Marks 40 Years. JAMA: The Journal of the American Medical Association, 294(8), 887–889. doi:10.1001/jama.294.8.887
- hdl:10665/345533. WHO/MHP/HPS/EML/2021.02.
- ^ "Opioid Use Disorder". The Lecturio Medical Concept Library. Retrieved 25 June 2021.
- PMID 19588333.
- PMID 19538000.
- ISBN 9789290614302.
- PMID 17313907.
- PMID 22793972.
- PMID 26806145.
- S2CID 205875314.
- PMID 28177515.
- S2CID 5903121.
- ^ "Methadone Oral: Side Effects". WebMD. Retrieved 25 June 2021.
- ^ a b c d e f g h i j k l m n o p "Methadone". Drugs.com. Archived from the original on 29 July 2017.
- ^ a b c d e f g h i j k l m n o p q "Methadone". MedlinePlus. Archived from the original on 27 February 2008.
- ^ a b c d e f g h "Dolophine: Drug Description". RxList. Archived from the original on 3 September 2008.
- ^ a b c d e "Methadone". MedicineNet. Archived from the original on 4 March 2016.
- PMID 21253542.
- PMID 21619737.
- PMID 16262036.
- ^ a b c d e f g h i j k l m "National Highway Traffic Safety Administration. Methadone. Drugs and Human Performance Fact Sheets" (PDF). NHTSA.
- ^ a b c d e f g h i j Sadovsky R (15 July 2000). "Tips from Other Journals – Public Health Issue: Methadone Maintenance Therapy". American Family Physician. 62 (2): 428–432. Archived from the original on 4 September 2015.
- ^ "Methadone Black Box Warnings - Drugs.com". drugs.com. Retrieved 20 November 2018.
- PMID 33157550.
- ^ a b c d e f g "Methadone (meth' a done)". MedlinePlus. National Institutes of Health. 1 February 2009. Archived from the original on 17 October 2013. Retrieved 23 October 2013.
- ^ "Methadone overdose". MedlinePlus. 3 October 2017.
- ^ a b "Methadone overdose: MedlinePlus Medical Encyclopedia". medlineplus.gov. Retrieved 13 November 2021.
- ^ a b Leavitt SB (September 2003). "Methadone Dosing & Safety in the Treatment of Opioid Addiction" (PDF). Addiction Treatment Forum.
- PMID 15955021.
- PMID 18454868.
- ^ "Methadone and Driving Article Abstracts: Brief Literature Review". Institute for Metropolitan Affairs, Roosevelt University. 14 February 2008. Archived from the original (DOC) on 3 November 2011.
- ^ Ford C, Barnard J, Bury J, Carnwath T, Gerada C, Joyce A, et al. (2005). Guidance for the use of methadone for the treatment of opioid dependence in primary care (PDF) (1st ed.). London: Royal College of General Practitioners. Archived from the original (PDF) on 21 May 2012.
- ^ "Increases in Methadone-Related Deaths:1999–2004". 4 September 2018. Archived from the original on 11 April 2010.
- ^ "The Killer Cure" Archived 18 June 2006 at the Wayback Machine The Charleston Gazette 2006
- ^ "Methadone-Associated Mortality, Report of a National Assessment". Archived from the original on 1 January 2016.
- ^ Finn S, Tuckwiller T (28 November 2006). "New warning issued on methadone". Charleston Gazette. Archived from the original on 13 February 2010.
- PMID 7562497.
- PMID 9058409.
- ISBN 978-0-19-923664-0.
- PMID 11561100. Archived from the originalon 28 August 2021. Retrieved 21 June 2011.
- PMID 8018740.
- ^ Eap CB, Déglon JJ, Baumann P (1999). "Pharmacokinetics and pharmacogenetics of methadone: Clinical relevance" (PDF). Heroin Addiction and Related Clinical Problems. 1 (1): 19–34.
- ^ S2CID 1396257.
- PMID 18154194. Archived from the originalon 20 May 2007.
- ^ Medscape Methadone Dosage. [1].
- PMID 14516485.
- ^ Code of Federal Regulations, Title 42, Sec 8.
- ^ "Methadone Hydrochloride Tablets, USP" (PDF). VistaPharm. Archived from the original (PDF) on 11 May 2013.
- PMID 698886.
- S2CID 41611298.
- S2CID 298931.
- PMID 15684283.
- PMID 10615732.
- ^ Dales pharmaceuticals patients information leaflet revision 09/10[verification needed]
- ^ Baselt R (2008). Disposition of Toxic Drugs and Chemicals in Man (8th ed.). Foster City, CA: Biomedical Publications. pp. 941–5.
- PMID 4516455.
- ^ S2CID 7720401.
- .
- ^ "Polamidon: Wirkung, Legalität, Substitution, Erfolgschancen & Entzug". My Way Betty Ford Klinik (in German). Retrieved 2 March 2023.
- ^ Bockmühl M, Ehrhart G, Schaumann O (1948). Über eine neue Klasse von spasmolytisch und analgetisch wirkenden (About a new class of compounds with a spasmolytic and analgesic effect). Vol. 561. Justus Liebigs Ann. pp. 561, 52–85.
- PMID 20506765.
- PMID 41087.
- ^ Morphine & Allied Drugs, Reynolds et al 1957 Ch 8
- ^ "Methadone Briefing". Archived from the original on 20 November 2003. Retrieved 9 July 2007.
- ^ Indro-Online.de Archived 13 January 2016 at the Wayback Machine (PDF format)
- ^ Preston A, Bennett G (2003). "The History of Methadone and Methadone Prescribing.". In Tober G, Strang E (eds.). In: Methadone Matters. Evolving Community Methadone Treatment of Opiate Addiction. Taylor and Francis Group.
- ^ ISBN 978-0-275-99605-5.
- PMID 946538.
- ^ Based on:
- "Methadone Prices and Methadone Coupons » 5 mg". GoodRx, Inc. Archived from the original on 11 September 2016. Retrieved 30 August 2016.[unreliable source?]
- "Methadone Prices and Methadone Coupons » 40 mg". GoodRx, Inc. Archived from the original on 11 September 2016. Retrieved 30 August 2016.[unreliable source?]
- "WHOCC – ATC/DDD Index". WHO Collaborating Centre for Drug Statistics Methodology. Archived from the original on 19 September 2016. Retrieved 30 August 2016.
- ^ Walsh L (16 June 2015). "Insurance and Payments". www.samhsa.gov. Retrieved 2 November 2018.
- ^ "Medicare Coverage of Substance Abuse Services" (PDF).
- ^ "Medicaid Coverage of Medications for the Treatment of Opioid Use Disorder" (PDF).
- ^ "Veterans Alcohol and Drug Dependence Rehabilitation Program". 1 November 2018.
- ^ "Methadone Maintenance Treatment". Drug Policy Alliance Lindesmith Library. Archived from the original on 11 May 2003.
- ^ "Methadone Research Web Guide". NIDA. Archived from the original on 15 February 2010.
- ^ National Institute on Drug Abuse. "How Much Does Opioid Treatment Cost?". Retrieved 2 November 2018.
- ^ "Is drug addiction treatment worth its cost?". Archived from the original on 28 July 2020. Retrieved 29 December 2019.
- ^ "DEA Diversion Control Division". Archived from the original on 2 March 2016. Retrieved 28 February 2016.
- ^ "DEA Diversion Control Division". Archived from the original on 4 March 2016. Retrieved 28 February 2016.
- ISBN 978-1-58112-404-0. Archivedfrom the original on 1 January 2014. Retrieved 16 May 2012.
- ^ "Methadone". www.samhsa.gov. 16 June 2015. Retrieved 15 February 2021.
- ^ "42 CFR § 8.12 – Federal opioid treatment standards". LII / Legal Information Institute. Retrieved 15 February 2021.
- ^ Schwirtz M (22 July 2008). "Russia Scorns Methadone for Heroin Addiction". The New York Times. Archived from the original on 7 December 2016.
- ^ "Caso Robson: Campanha pede justiça a ex-funcionário de Fernando preso há 562 dias na Rússia" [Robson case: Campaign calls for justice for former Fernando employee imprisoned 562 days in Russia]. ESPN Caso Robson (in Portuguese). 30 September 2020.
- PMID 25533862.
External links
- Methadone, Substance Abuse and Mental Health Services Administration, U.S. Department of Health and Human Services
- Tapering off of methadone maintenance
- DE patent 711069, Dr Max Bockmuehl & Dr Gustav Ehrhart, "Verfahren zur Darstellung von basischen Estern", published 1941-09-25, issued 1941-09-25, assigned to IG Farbenindustrie AG