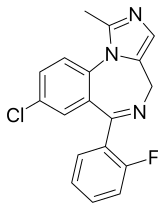
Midazolam
 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | /mɪˈdæzəlæm/ |
| Trade names | Versed, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a609003 |
| License data | |
| Pregnancy category |
|
intranasal | |
| Drug class | Benzodiazepine |
| ATC code | |
| Legal status | |
| Legal status | |
| Onset of action | Within 5 min (IV), 15 min (IM), 20 min (oral)[10] |
| Elimination half-life | 1.5–2.5 hours[11] |
| Duration of action | 1 to 6 hrs[10] |
| Excretion | Kidney |
| Identifiers | |
| |
JSmol) | |
| |
| |
| (verify) | |
Midazolam, sold under the brand name Versed among others, is a
The drug does not cause an individual to become unconscious, merely to be sedated. Effects last between one and six hours.
Side effects can include a decrease in efforts to breathe,
Midazolam was patented in 1974 and came into medical use in 1982.
Medical uses
Seizures
Midazolam is sometimes used for the acute management of prolonged
Drawbacks include a high degree of breakthrough seizures—due to the short half-life of midazolam—in over 50% of people treated, as well as treatment failure in 14–18% of people with refractory status epilepticus. Tolerance develops rapidly to the anticonvulsant effect, and the dose may need to be increased by several times to maintain anticonvulsant therapeutic effects. With prolonged use, tolerance and
Procedural sedation
Intravenous midazolam is indicated for procedural sedation (often in combination with an
Midazolam is sometimes used in neonatal intensive care units. When used, additional caution is required in
Sedation using midazolam can be used to relieve anxiety and manage behaviour in children undergoing dental treatment.[32]
Agitation
Midazolam, in combination with an antipsychotic drug, is indicated for the acute management of schizophrenia when it is associated with aggressive or out-of-control behaviour.[33]
End of life care
In the final stages of , midazolam is routinely used at low doses via subcutaneous injection to help with agitation, restlessness or anxiety in the last hours or days of life.
Administration
This section needs additional citations for verification. (March 2024) |
Routes of administration of midazolam can be oral, intranasal, buccal, intravenous, and intramuscular.
| Perioperative use | 0.15 to 0.40 mg/kg IV |
| Premedication | 0.07 to 0.10 mg/kg IM |
| Intravenous sedation | 0.05 to 0.15 mg/kg IV |
Contraindications
Benzodiazepines require special precaution if used in the elderly, during pregnancy, in children, in alcohol- or other drug-dependent individuals or those with
Side effects

Side effects of midazolam in the elderly are listed above.[13] People experiencing amnesia as a side effect of midazolam are generally unaware their memory is impaired, unless they had previously known it as a side effect.[41]
Long-term use of benzodiazepines has been associated with long-lasting deficits in memory, and show only partial recovery six months after stopping benzodiazepines.
In rare susceptible individuals, midazolam has been known to cause a paradoxical reaction, a well-documented complication with benzodiazepines. When this occurs, the individual may experience anxiety, involuntary movements, aggressive or violent behavior, uncontrollable crying or verbalization, and other similar effects. This seems to be related to the altered state of consciousness or disinhibition produced by the drug. Paradoxical behavior is often not recalled by the patient due to the amnesia-producing properties of the drug. In extreme situations, flumazenil can be administered to inhibit or reverse the effects of midazolam. Antipsychotic medications, such as haloperidol, have also been used for this purpose.[45]
Midazolam is known to cause respiratory depression. In healthy humans, 0.15 mg/kg of midazolam may cause respiratory depression, which is postulated to be a central nervous system (CNS) effect.[46] When midazolam is administered in combination with fentanyl, the incidence of hypoxemia or apnea becomes more likely.[47]
Although the incidence of respiratory depression/arrest is low (0.1–0.5%) when midazolam is administered alone at normal doses,[48][49] the concomitant use with CNS acting drugs, mainly analgesic opiates, may increase the possibility of hypotension, respiratory depression, respiratory arrest, and death, even at therapeutic doses.[47][48][50][51] Potential drug interactions involving at least one CNS depressant were observed for 84% of midazolam users who were subsequently required to receive the benzodiazepine antagonist flumazenil.[52] Therefore, efforts directed toward monitoring drug interactions and preventing injuries from midazolam administration are expected to have a substantial impact on the safe use of this drug.[52]
Pregnancy and breastfeeding
Midazolam, when taken during the
Elderly
Additional caution is required in the elderly, as they are more sensitive to the pharmacological effects of benzodiazepines, metabolise them more slowly, and are more prone to adverse effects, including drowsiness, amnesia (especially anterograde amnesia), ataxia, hangover effects, confusion, and falls.[13]
Tolerance, dependence, and withdrawal
A benzodiazepine dependence occurs in about one-third of individuals who are treated with benzodiazepines for longer than 4 weeks,
Chronic users of benzodiazepine medication who are given midazolam experience reduced therapeutic effects of midazolam, due to tolerance to benzodiazepines.
Overdose
A midazolam overdose is considered a medical emergency and generally requires the immediate attention of medical personnel. Benzodiazepine overdose in healthy individuals is rarely life-threatening with proper medical support; however, the toxicity of benzodiazepines increases when they are combined with other CNS depressants such as alcohol, opioids, or tricyclic antidepressants. The toxicity of benzodiazepine overdose and the risk of death are also increased in the elderly and those with
Symptoms of midazolam overdose can include:[58][59]
|
|
Detection in body fluids
Concentrations of midazolam or its major metabolite, 1-hydroxymidazolam glucuronide, may be measured in plasma, serum, or whole blood to monitor for safety in those receiving the drug therapeutically, to confirm a diagnosis of poisoning in hospitalized patients, or to assist in a forensic investigation of a case of fatal overdosage. Patients with renal dysfunction may exhibit prolongation of elimination half-life for both the parent drug and its active metabolite, with accumulation of these two substances in the bloodstream and the appearance of adverse depressant effects.[60]
Interactions
Pharmacology
Midazolam is a short-acting benzodiazepine in adults with an elimination half-life of 1.5–2.5 hours.
History
Midazolam is among about 35 benzodiazepines currently used medically,
Society and culture
Cost
Midazolam is available as a generic medication.[14]
Availability
Midazolam is available in the United States as a syrup or as an injectable solution.[75]
Dormicum brand midazolam is marketed by Roche as white, oval, 7.5 mg tablets in boxes of two or three blister strips of 10 tablets, and as blue, oval, 15 mg tablets in boxes of two (Dormonid 3x) blister strips of 10 tablets. The tablets are imprinted with "Roche" on one side and the dose of the tablet on the other side. Dormicum is also available as 1, 3, and 10 mL ampoules at a concentration of 5 mg/mL. Another manufacturer, Novell Pharmaceutical Laboratories, makes it available as Miloz in 3 and 5 mL ampoules. Midazolam is the only water-soluble benzodiazepine available. Another maker is Roxane Laboratories; the product in an oral solution, midazolam HCl Syrup, 2 mg/mL clear, in a red to purplish-red syrup, cherry in flavor. It becomes soluble when the injectable solution is buffered to a pH of 2.9–3.7. Midazolam is also available in liquid form.
Legal status
In the Netherlands, midazolam is a List II drug of the Opium Law. Midazolam is a Schedule IV drug under the Convention on Psychotropic Substances.[79] In the United Kingdom, midazolam is a Schedule 3/Class C controlled drug.[80] In the United States, midazolam (DEA number 2884) is on the Schedule IV list of the Controlled Substances Act as a non-narcotic agent with low potential for abuse.[81]
Marketing authorization
In 2011, the European Medicines Agency (EMA) granted a marketing authorisation for a buccal application form of midazolam, sold under the brand name Buccolam. Buccolam was initially approved for the treatment of prolonged, acute, convulsive seizures in people from three months to less than 18 years of age. This was the first application of a paediatric-use marketing authorisation.[82][83]
Use in executions

The drug has been introduced for use in executions by lethal injection in certain jurisdictions in the United States in combination with other drugs. It was introduced to replace pentobarbital after the latter's manufacturer disallowed that drug's use for executions.[84] Midazolam acts as a sedative but will fail to render the condemned prisoner unconscious, at which time vecuronium bromide and potassium chloride are administered, stopping the prisoner's breathing and heart, respectively. Since the condemned prisoner is not rendered unconscious but is merely sedated, the administration of vecuronium bromide and potassium chloride can cause extreme pain and panic in the person being executed.[85]
Midazolam has been used as part of a three-drug cocktail, with vecuronium bromide and potassium chloride, in Florida and Oklahoma prisons.[86] Midazolam has also been used along with hydromorphone in a two-drug protocol in Ohio and Arizona.[86]
Notable incidents
The state of Florida used midazolam to execute William Frederick Happ in October 2013.[85]
The state of Ohio used midazolam in the execution of Dennis McGuire in January 2014; it took McGuire 24 minutes to die after the procedure started, and he gasped and appeared to be choking during that time, leading to questions about the dosing and timing of the drug administration, as well as the choice of drugs.[87]
The usage of midazolam in executions became controversial after condemned inmate Clayton Lockett apparently regained consciousness and started speaking midway through his 2014 execution when the state of Oklahoma attempted to execute him with an untested three-drug lethal injection combination using 100 mg of midazolam. Prison officials reportedly discussed taking him to a hospital before he was pronounced dead of a heart attack 40 minutes after the execution began. An observing doctor stated that Lockett's vein had ruptured. It is not clear whether his death was caused by one or more of the drugs or by a problem in the administration procedure, nor is it clear what quantities of vecuronium bromide and potassium chloride were released to his system before the execution was cancelled.[88][89]
According to news reports, the execution of Ronald Bert Smith in the state of Alabama on 8 December 2016 went awry[clarification needed] soon after midazolam was administered,[90] again putting the effectiveness of the drug in question.[84]
In October 2016, the state of Ohio announced that it would resume executions in January 2017, using a formulation of midazolam, vecuronium bromide, and potassium chloride, but this was blocked by a federal judge.[91][92] On 26 July 2017, Ronald Phillips was executed with a three-drug cocktail including midazolam after the Supreme Court refused to grant a stay.[93] Prior to this, the last execution in Ohio had been that of Dennis McGuire.[94] Murderer Gary Otte's lawyers unsuccessfully challenged his Ohio execution, arguing that midazolam might not protect him from serious pain when the other drugs are administered. He died without incident in about 14 minutes on 13 September 2017.[95]
On 24 April 2017, the state of Arkansas carried out a double-execution, of Jack Harold Jones, 52, and Marcel Williams, 46. Arkansas attempted to execute eight people before its supply of midazolam expired on 30 April 2017. Two of them were granted a stay of execution, and another, Ledell T. Lee, 51, was executed on 20 April 2017.[96]
On 28 October 2021, the state of Oklahoma executed inmate
Legal challenges
In
The state of Nevada is also known to use midazolam in execution procedures. In July 2018, one of the manufacturers accused state officials of obtaining the medication under pretences. This incident was the first time a drug company successfully, though temporarily, halted an execution.[99] A previous attempt in 2017, to halt an execution in the state of Arizona by another drug manufacturer was not successful.[100]
References
- FDA. Retrieved 22 October 2023.
- ^ Anvisa (31 March 2023). "RDC Nº 784 - Listas de Substâncias Entorpecentes, Psicotrópicas, Precursoras e Outras sob Controle Especial" [Collegiate Board Resolution No. 784 - Lists of Narcotic, Psychotropic, Precursor, and Other Substances under Special Control] (in Brazilian Portuguese). Diário Oficial da União (published 4 April 2023). Archived from the original on 3 August 2023. Retrieved 16 August 2023.
- ^ "Product information". Health Canada. 28 June 2004. Retrieved 14 April 2024.
- ^ "Health product highlights 2021: Annexes of products approved in 2021". Health Canada. 3 August 2022. Retrieved 25 March 2024.
- ^ "Buccolam 10 mg oromucosal solution - Summary of Product Characteristics (SmPC)". (emc). 7 June 2022. Retrieved 16 June 2022.
- ^ "Hypnovel 10mg in 2ml - Summary of Product Characteristics (SmPC)". (emc). 16 February 2022. Retrieved 16 June 2022.
- ^ "Seizalam- midazolam hydrochloride injection, solution". DailyMed. Archived from the original on 12 May 2021. Retrieved 1 January 2021.
- PMID 6138080.
- PMID 12402721.
- ^ a b c d e f g h i "Midazolam Hydrochloride". The American Society of Health-System Pharmacists. Archived from the original on 5 September 2015. Retrieved 1 August 2015.
- ^ a b "Midazolam Injection" (PDF). Medsafe. New Zealand Ministry of Health. 26 October 2012. Archived from the original (PDF) on 22 February 2016. Retrieved 6 April 2016.
- ^ S2CID 33207030.
- ^ S2CID 24453988.
- ^ ISBN 9781284057560.
- ^ "Midazolam use while Breastfeeding". Archived from the original on 5 September 2015. Retrieved 29 August 2015.
- ISBN 9783527607495. Archivedfrom the original on 30 November 2021. Retrieved 24 August 2020.
- hdl:10665/345533. WHO/MHP/HPS/EML/2021.02.
- PMID 10030438.
- PMID 29320603.
- ^ PMID 16179702.
- PMID 17114841.
- S2CID 2865644.
- ^ PMID 16635708.
- S2CID 41731847.
- PMID 15663030.
- PMID 19770414.
- PMID 18440381.
- PMID 16305452.
- PMID 16305451.
- PMID 19471072.
- PMID 18254040.
- PMID 30566228.
- PMID 27885664.
- ^ Liverpool Care Pathway (January 2005). "Care of the Dying Pathway (lcp) (Hospital)" (PDF). United Kingdom. Archived from the original (PDF) on 8 October 2011.
- PMID 17298256.
- ^ Royal College of Physicians (September 2009). "National care of the dying audit 2009". United Kingdom. Archived from the original on 20 January 2010. Retrieved 10 February 2010. "[I]n their last 24 hours... 31% had low doses of medication to [control distress from agitation or restlessness]... the remaining 4% required higher doses"
- PMID 19900604.
- PMID 18176312.
- ^ PMID 18175099.
- S2CID 27888650.
- S2CID 7142863.
- ^ S2CID 7743205.
- S2CID 25592318.
- ^ PMID 17530139. Archived from the originalon 4 October 2011.
- from the original on 6 June 2011.
- S2CID 28308031.
- ^ PMID 2122773.
- ^ S2CID 42657347.
- PMID 2302291.
- S2CID 36531097.
- PMID 2955719.
- ^ S2CID 12973546.
- PMID 7881198.
- PMID 20347563.
- PMID 12145054.
- S2CID 42497090.
- S2CID 31542770. Archived from the originalon 12 January 2002.
- ^ ISBN 978-0-443-10057-4.
- ^ ISBN 978-0-7817-6154-3.
- ISBN 978-0-9626523-7-0.
- S2CID 25382546.
- S2CID 46963549.
- PMID 16380358.
- ISBN 978-0-7817-8763-5. Archivedfrom the original on 20 February 2017.
- S2CID 24319062.
- ^ PMID 36432161.
- ^ ISBN 978-81-8448-149-5.
- ^ US patent 4166185, Walser A, Fryer RI, Benjamin L, "Imidazo[1,5-α] [1,4]benzodiazepines", published 1979-08-28, issued 1979-08-28, assigned to Hoffmann La Roche Inc. Archived 17 June 2022 at the Wayback Machine
- ISBN 978-1-4160-0253-6.
- ISBN 978-0-323-01226-3.
- ISBN 978-1-84628-463-2. Archivedfrom the original on 8 September 2017.
- ISBN 978-0-7216-0258-5.
- ISBN 978-0-8138-2061-3. Archivedfrom the original on 12 November 2012.
- ^ "CIA considered potential truth serum for terror suspects after 9/11". NBC News. 13 November 2018. Archived from the original on 27 November 2018. Retrieved 27 November 2018.
- ^ FDA, ed. (2015). "Orange Book: Approved Drug Products; Midazolam". Archived from the original on 17 August 2016. Retrieved 25 July 2015.
- PMID 16632296.
- S2CID 19088163.
- S2CID 42219786.
- ^ International Narcotics Control Board (August 2003). "List of psychotropic substances under international control" (PDF). incb.org. Archived from the original (PDF) on 31 August 2012. Retrieved 17 December 2008.
- ^ Blackpool NHS Primary Care Trust (2007). "Medicines Management Update" (PDF). United Kingdom: National Health Service. Archived from the original (PDF) on 4 December 2010.
- ^ "US DEA Schedules". Archived from the original on 16 May 2013.
- ^ "Monthly Report" (PDF). Committee for Medicinal Products for Human Use (CHMP). 5 July 2011. p. 1. Archived (PDF) from the original on 23 January 2012.
- ^ "ViroPharma's Buccolam (Midazolam, Oromucosal Solution) Granted European Marketing Authorization for Treatment of Acute Seizures". PR Newswire. 6 September 2011. Archived from the original on 28 August 2021. Retrieved 6 November 2011.
- ^ a b Schulz S (10 December 2016). "Die fahrlässige Hinrichtung des Ronald Smith" [The Neglected Execution of Ronald Smith] (in German). der Spiegel. Archived from the original on 10 December 2016. Retrieved 10 December 2016.
- ^ a b Watkins M (15 October 2013). "Happ executed using new drug". The Gainesville Sun. Archived from the original on 12 December 2013.
- ^ a b "State by State Lethal Injection". Death Penalty Information Center. Archived from the original on 3 April 2015. Retrieved 10 April 2015.
- ^ Ford D, Fantz A (16 January 2014). "Controversial execution in Ohio uses new drug combination". CNN. Archived from the original on 17 January 2014.
- ^ Ekholm E (29 April 2014). "One execution botched, Oklahoma delays the next". The New York Times. Archived from the original on 13 March 2017.
- ^ Fretland K (30 April 2014). "Oklahoma execution: Clayton Lockett writhes on gurney in botched procedure". The Guardian. London. Archived from the original on 30 April 2014.
- ^ Sanburn J (9 December 2016). "The Drug Used in Alabama's Problematic Execution Has a Controversial History". Time. Archived from the original on 9 December 2016. Retrieved 10 December 2016.
- ^ Rebecca H (26 January 2017). "Federal Judge Blocks Ohio's Lethal Injection Protocol". The Two-Way (blog). NPR. Archived from the original on 16 March 2017. Retrieved 15 March 2017.
- from the original on 14 March 2017. Retrieved 15 March 2017.
- Daily News. New York. 25 July 2017. Archivedfrom the original on 29 July 2017. Retrieved 27 July 2017.
- ^ "Ohio to resume executions with new jab". BBC News. 3 October 2016. Archived from the original on 5 October 2016. Retrieved 3 October 2016.
- ^ "Ohio executes man convicted of killing two in back-to-back robberies". CBS News. Associated Press. Archived from the original on 14 September 2017. Retrieved 15 September 2017.
- ^ McCausland P (21 April 2017). "Arkansas Executes Ledell Lee, State's First Inmate Put to Death Since 2005". NBC News. Archived from the original on 28 April 2017. Retrieved 28 April 2017.
- ^ KOCO Staff (28 October 2021). "Oklahoma executes death row inmate John Grant". ABC News. Archived from the original on 28 April 2017. Retrieved 29 October 2021.
- ^ "US Supreme Court backs use of contentious execution drug". BBC News. 29 June 2015. Archived from the original on 1 July 2015. Retrieved 29 June 2015.
- ^ Porter T (6 January 2019). "Death row prisoner kills himself after execution halted". Tom Porter on Sunday. Newsweek. Archived from the original on 6 January 2019. Retrieved 6 January 2019.
- ^ Bowden J (5 January 2019). "Nevada inmate on death row whose execution was delayed commits suicide". Briefing Room (blog). The Hill. Archived from the original on 6 January 2019. Retrieved 6 January 2019.
