Misconceptions about HIV/AIDS
The spread of
The relationship between HIV and AIDS
HIV is the same as AIDS
HIV is an acronym for
Treatment
Cure
High levels of HIV-1 (often HAART-resistant) develop if treatment is stopped, if compliance with treatment is inconsistent, or if the virus spontaneously develops resistance to an individual's regimen.
Sexual intercourse with a virgin will cure AIDS
The myth that sex with a virgin will cure AIDS is prevalent in South Africa.[9][10][11] Sex with an uninfected virgin does not cure an HIV-infected person, and such contact will expose the uninfected individual to HIV, potentially further spreading the disease. This myth has gained considerable notoriety as the perceived reason for certain sexual abuse and child molestation occurrences, including the rape of infants, in South Africa.[9][10]
Sexual intercourse with an animal will avoid or cure AIDS
In 2002, the National Council of
HIV antibody testing is unreliable
Diagnosis of infection using antibody testing is a well-established technique in medicine. HIV antibody tests exceed the performance of most other infectious disease tests in both sensitivity (the ability of the screening test to give a positive finding when the person tested truly has the disease) and specificity (the ability of the test to give a negative finding when the subjects tested are free of the disease under study). Many current HIV antibody tests have sensitivity and specificity in excess of 96% and are therefore extremely reliable.[13] While most patients with HIV show an antibody response after six weeks, window periods vary and may occasionally be as long as three months.[14]
Progress in testing methodology has enabled detection of viral genetic material, antigens, and the virus itself in bodily fluids and cells. While not widely used for routine testing due to high cost and requirements in laboratory equipment, these direct testing techniques have confirmed the validity of the antibody tests.[15][16][17][18][19][20][excessive citations]
Positive HIV antibody tests are usually followed up by retests and tests for antigens, viral genetic material and the virus itself, providing confirmation of actual infection.[citation needed]
HIV infection

HIV can be spread through casual contact with an HIV infected individual
One cannot become infected with HIV through normal contact in social settings, schools, or in the workplace. Other examples of casual contact in which HIV infection will not occur include shaking someone's hand, hugging or "dry" kissing someone, using the same
Other interactions that could theoretically result in person-to-person transmission include caring for
HIV-positive individuals can be detected by their appearance
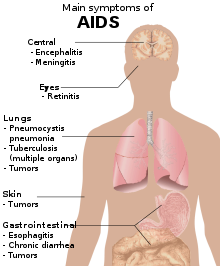
Due to media images of the effects of AIDS, many people believe that individuals infected with HIV always appear a certain way, or at least appear different from an uninfected, healthy person. In fact, disease progression can occur over a long period of time before the onset of symptoms, and as such, HIV infections cannot be detected based on appearance.[26]
HIV cannot be transmitted through oral sex
Contracting HIV through oral sex is possible, but it is much less likely than from anal sex and penile–vaginal intercourse.[27] No cases of such a transmission were observed in a sample of 8965 people performing receptive oral sex.[28]
HIV is transmitted by mosquitoes
When mosquitoes bite a person, they do not inject the blood of a previous victim into the person they bite next. Mosquitoes do, however, inject their saliva into their victims, which may carry diseases such as dengue fever, malaria, yellow fever, or West Nile virus and can infect a bitten person with these diseases. HIV is not transmitted in this manner.[29] On the other hand, a mosquito may have HIV-infected blood in its gut, and if swatted on the skin of a human who then scratches it, transmission is hypothetically possible,[30] though this risk is extremely small, and no cases have yet been identified through this route.
HIV survives for only a short time outside the body
HIV can survive at room temperature outside the body for hours if dry (provided that initial concentrations are high),[31] and for weeks if wet (in used syringes/needles).[32] However, the amounts typically present in bodily fluids do not survive nearly as long outside the body—generally no more than a few minutes if dry.[23]
HIV can infect only homosexual men and drug users
HIV can transmit from one person to another if an engaging partner is HIV positive. In the United States, the main route of infection is via homosexual anal sex, while for women transmission is primarily through heterosexual contact.[33] It is true that anal sex (regardless of the sex of the receptive partner) carries a higher risk of infection than most sex acts, but most penetrative sex acts between any individuals carry some risk. Properly used condoms can reduce this risk.[34]
An HIV-infected person cannot have children
HIV-infected women remain fertile, although in late stages of HIV disease a pregnant woman may have a higher risk of miscarriage. Normally, the risk of transmitting HIV to the unborn child is between 15 and 30%. However, this may be reduced to just 2–3% if patients carefully follow medical guidelines.[35][36]
HIV cannot be the cause of AIDS because the body develops a vigorous antibody response to the virus
This reasoning ignores numerous examples of
HIV has a well-recognized capacity to
Only a small number of CD4+ T-cells are infected by HIV, not enough to damage the immune system
Although the fraction of CD4+ T-cells that is infected with HIV at any given time is never high (only a small subset of activated cells serve as ideal targets of infection), several groups have shown that rapid cycles of death of infected cells and infection of new target cells occur throughout the course of the disease.[39] Macrophages and other cell types are also infected with HIV and serve as reservoirs for the virus.[citation needed]
Furthermore, like other viruses, HIV is able to suppress the immune system by secreting proteins that interfere with it. For example, HIV's
Infected lymphocytes express the Fas ligand, a cell-surface protein that triggers the death of neighboring uninfected T-cells expressing the Fas receptor.[40] This "bystander killing" effect shows that great harm can be caused to the immune system even with a limited number of infected cells.[citation needed]
History of HIV/AIDS

The current consensus is that HIV was introduced to North America by a Haitian immigrant who contracted it while working in the Democratic Republic of the Congo in the early 1960s, or from another person who worked there during that time.[41] In 1981 on June 5, the U.S. Centers for Disease Control and Prevention (CDC) published a Morbidity and Mortality Weekly Report (MMWR) describing cases of a rare lung infection, Pneumocystis carinii pneumonia (PCP), in five healthy gay men in Los Angeles. This edition would later become MMWR's first official reporting of the AIDS epidemic in North America.[42] By year-end, a cumulative total of 337 cases of severe immune deficiency had been reported, and 130 out of the 337 reported cases had died.[42] On September 24, 1982, the CDC used the term "AIDS" (acquired immune deficiency syndrome) for the first time, and released the first case definition of AIDS: "a disease at least moderately predictive of a defect in cell-mediated immunity, occurring in a person with no known case for diminished resistance to that disease."[42] The March 4, 1983 edition of the Morbidity and Mortality Weekly Report (MMWR) noted that most cases of AIDS had been reported among homosexual men with multiple sexual partners, injection drug users, Haitians, and hemophiliacs. The report suggested that AIDS may be caused by an infectious agent that is transmitted sexually or through exposure to blood or blood products, and issued recommendations for preventing transmission.[42] Although most cases of HIV/AIDS were discovered in gay men, on January 7, 1983, the CDC reported cases of AIDS in female sexual partners of males with AIDS.[42] In 1984, scientists identified the virus that causes AIDS, which was first named after the T-cells affected by the strain and is now called HIV or human immunodeficiency virus.[43]
Origin of AIDS through human–monkey sexual intercourse
While HIV is most likely a mutated form of
Tennessee State Senator Stacey Campfield was the subject of controversy in 2012 after stating that AIDS was the result of a human having sexual intercourse with a monkey.[48][49]
Gaëtan Dugas as "patient zero"
The Canadian flight attendant Gaëtan Dugas has been referred to as "patient zero" of the HIV/AIDS epidemic, meaning the first case of HIV/AIDS in the United States. In fact, the "patient zero" moniker originated from a misinterpretation of a 1984 study[50] that referred to Dugas as "patient O", where the O stood for "out of California".[51][52] A 2016 study published in Nature found "neither biological nor historical evidence that [Dugas] was the primary case in the US or for subtype B as a whole."[53]
AIDS denialism
There is no AIDS in Africa, as AIDS is nothing more than a new name for old diseases
The diseases that have come to be associated with
For example, in a study in
HIV is not the cause of AIDS
There is broad scientific consensus that HIV is the cause of AIDS, but some individuals reject this consensus, including biologist Peter Duesberg, biochemist David Rasnick, journalist/activist Celia Farber, conservative writer Tom Bethell, and intelligent design advocate Phillip E. Johnson. (Some one-time skeptics have since rejected AIDS denialism, including physiologist Robert Root-Bernstein, and physician and AIDS researcher Joseph Sonnabend.)[citation needed]
A great deal is known about the pathogenesis of HIV disease, even though important details remain to be elucidated. However, a complete understanding of the pathogenesis of a disease is not a prerequisite to knowing its cause. Most infectious agents have been associated with the disease they cause long before their pathogenic mechanisms have been discovered. Because research in pathogenesis is difficult when precise animal models are unavailable, the disease-causing mechanisms in many diseases, including tuberculosis and hepatitis B, are poorly understood, but the pathogens responsible are very well established.[3]
AZT and other antiretroviral drugs, not HIV, cause AIDS
The vast majority of people with AIDS never received antiretroviral drugs, including those in developed countries prior to the licensure of AZT in 1987. Even today, very few individuals in developing countries have access to these medications.[57]
In the 1980s, clinical trials enrolling patients with AIDS found that AZT given as single-drug therapy conferred a survival advantage compared to placebo, albeit modest and short-lived. Among HIV-infected patients who had not yet developed AIDS, placebo-controlled trials found that AZT given as a single-drug therapy delayed, for a year or two, the onset of AIDS-related illnesses. The lack of excess AIDS cases and death in the AZT arms of these placebo-controlled trials effectively counters the argument that AZT causes AIDS.[37]
Subsequent clinical trials found that patients receiving two-drug combinations had up to 50% increases in time to progression to AIDS and in survival when compared to people receiving single-drug therapy. In more recent years, three-drug combination therapies have produced another 50–80% improvements in progression to AIDS and in survival when compared to two-drug regimens in clinical trials.[58] Use of potent anti-HIV combination therapies has contributed to dramatic reductions in the incidence of AIDS and AIDS-related deaths in populations where these drugs are widely available, an effect which would be unlikely if antiretroviral drugs caused AIDS.[59][60][61][62][63][64][65][66][67][68][excessive citations]
Behavioral factors such as recreational drug use and multiple sexual partners—not HIV—account for AIDS
The proposed behavioral causes of AIDS, such as multiple sexual partners and long-term
Compelling evidence against the hypothesis that behavioral factors cause AIDS comes from recent studies that have followed cohorts of
Other studies show that among homosexual men and injection-drug users, the specific immune deficit that leads to AIDS—a progressive and sustained loss of
In a survey of 229 HIV-seronegative injection-drug users in
AIDS among transfusion recipients is due to underlying diseases that necessitated the transfusion, rather than to HIV
This notion is contradicted by a report by the Transfusion Safety Study Group (TSSG), which compared HIV-negative and HIV-positive blood recipients who had been given
High usage of clotting factor concentrate, not HIV, leads to CD4+ T-cell depletion and AIDS in hemophiliacs
This view is contradicted by many studies. For example, among HIV-seronegative patients with
In a cohort in the
Among HIV-infected hemophiliacs, Transfusion Safety Study investigators found that neither the purity nor the amount of factor VIII therapy had a deleterious effect on CD4+ T-cell counts.[78] Similarly, the Multicenter Hemophilia Cohort Study found no association between the cumulative dose of plasma concentrate and incidence of AIDS among HIV-infected hemophiliacs.[79]
The distribution of AIDS cases casts doubt on HIV as the cause. Viruses are not gender-specific, yet only a small proportion of AIDS cases are among women
The distribution of AIDS cases, whether in the United States or elsewhere in the world, invariably mirrors the prevalence of HIV in a population. In the United States, HIV first appeared in populations of
Women in the United States, however, are increasingly becoming HIV-infected, usually through the exchange of HIV-contaminated needles or sex with an HIV-infected male. The CDC estimates that 30 percent of new HIV infections in the United States in 1998 were in women. As the number of HIV-infected women has risen, so too has the number of female AIDS patients in the United States. Approximately 23% of U.S. adult/adolescent AIDS cases reported to the CDC in 1998 were among women. In 1998, AIDS was the fifth leading cause of death among women aged 25 to 44 in the United States, and the third leading cause of death among African-American women in that age group.[81]
In Africa, HIV was first recognized in sexually active
HIV is not the cause of AIDS because many individuals with HIV have not developed AIDS
HIV infections have a prolonged and variable course. The median period of time between infection with HIV and the onset of clinically apparent disease is approximately 10 years in
As with many diseases, a number of factors can influence the course of HIV disease. Factors such as age or genetic differences between individuals, the level of virulence of the individual strain of virus, as well as exogenous influences such as co-infection with other microbes may determine the rate and severity of HIV disease expression. Similarly, some people infected with hepatitis B, for example, show no symptoms or only jaundice and clear their infection, while others suffer disease ranging from chronic liver inflammation to cirrhosis and hepatocellular carcinoma. Co-factors probably also determine why some smokers develop lung cancer while others do not.[38][85][86]
HIV is not the cause of AIDS because some people have symptoms associated with AIDS but are not infected with HIV
Most AIDS symptoms result from the development of opportunistic infections and cancers associated with severe immunosuppression secondary to HIV.[citation needed]
However, immunosuppression has many other potential causes. Individuals who take
The diseases associated with AIDS, such as
HIV is the underlying cause of the condition named AIDS, but the additional conditions that may affect an AIDS patient are dependent upon the
AIDS can be prevented with complementary or alternative medicine
Many HIV-infected people turn to complementary and alternative medicine, such as traditional medicine, especially in areas where conventional therapies are less widespread.[88] However, the overwhelming majority of scientifically rigorous research indicates little or negative effect on patient outcomes such as HIV-symptom severity and disease duration, and mixed outcomes on psychological well-being.[89][90] It is important that patients notify their healthcare provider prior to beginning any treatment, as certain alternative therapies may interfere with conventional treatment.[91][92]
See also
References
- PMID 18205765.
- ^ "AIDS epidemic update" (PDF). World Health Organization. Retrieved 29 July 2011.
- ^ National Institute of Allergy and Infectious Disease. 4 September 2009. Retrieved 29 May 2015.
- ^ "Children and HIV and AIDS – What is the relationship between HIV and AIDS and emergencies?". UNICEF. Archived from the original on 2017-09-21. Retrieved 2018-09-30.
- PMID 12466764.
- ISBN 978-0-7637-0086-7.
- ^ "HIV Undetectable=Untransmittable (U=U), or Treatment as Prevention | NIH: National Institute of Allergy and Infectious Diseases".
- PMID 28385131.
- ^ a b Flanagan, Jane (2001-11-11). "South African men rape babies as 'cure' for Aids". Telegraph. London. Archived from the original on 2008-06-12. Retrieved 2009-03-25.
- ^ S2CID 2706882.
- S2CID 34857351.
- ^ "Bestiality new Aids myth – SPCA" Archived 2008-12-19 at the Wayback Machine, March 25, 2002; retrieved February 22, 2007
- ^ "HIV Assays: Operational Characteristics", World Health Organization, 2004
- ^ Gilbert, Mark; Krajden, Mel (July–August 2010). "Don't wait to test for HIV". BC Medical Journal. 52 (6): 308.
- PMID 2298875.
- PMID 2046708.
- PMID 7882108.
- PMID 10548127.
- PMID 10207552.
- PMID 9077430.
- S2CID 28722212.
- S2CID 30065399.
- ^ a b "Kissing and HIV"
- ^ "THT: "Ways HIV is not passed on"". Archived from the original on 2015-06-01. Retrieved 2007-10-10.
- PMID 16470132.
- ^ Piya Sorcar (March 2009). "Teaching Taboo Topics Without Talking About Them: An Epistemic Study of a New Approach to HIV/AIDS Prevention Education in India" (PDF). Stanford University, TeachAids.
- PMID 20624114.
- PMID 24809629.
- PMID 2479697.
- PMID 2889266.
- PMID 2419594.
- PMID 10932845.
- ^ "HIV Surveillance –Epidemiology of HIV Infection (through 2008)". Center for Disease Control. Archived from the original on 4 March 2011. Retrieved 1 March 2011.
- ^ "Condoms and STDs: Fact Sheet for Public Health Personnel". Centers for Disease Control and Prevention. 10 February 2010. Retrieved 5 January 2011.
- PMID 9749412.
- ^ WHO, 2005
- ^ a b c "Disease Progression Despite Antibodies", "The Relationship Between the Human Immunodeficiency Virus and the Acquired Immunodeficiency Syndrome", National Institute of Allergy and Infectious Diseases, September, 1995
- ^ PMID 8464405.
- PMID 10712427.
- PMID 10224289.
- ^ "Key HIV strain 'came from Haiti'". BBC News. 2007-10-30. Retrieved 2010-05-04.
- ^ a b c d e "A Timeline of HIV and AIDS". HIV.gov. 2016-05-11. Retrieved 2018-09-30.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ Wilson, Jacque Wilson. "Timeline: AIDS moments to remember". CNN. Retrieved 2018-10-01.
- S2CID 38760788.
- PMID 22229120.
- S2CID 4416837.
- PMID 18833279.)
{{cite journal}}: CS1 maint: numeric names: authors list (link - ^ Signorile, Michelangelo (2012-01-26). "Stacey Campfield, Tennessee Senator Behind 'Don't Say Gay' Bill, On Bullying, AIDS And Homosexual 'Glorification'". The Huffington Post. Retrieved 2012-01-30.
- ^ "Knoxville Republican says AIDS came from man having sex with a monkey then with other men". Politifact. Retrieved 16 April 2018.
- PMID 6608269.
- ^ Johnson, Brian D. (17 April 2019). "How a typo created a scapegoat for the AIDS epidemic". Maclean's. Retrieved 20 April 2019.
- ^ "Researchers Clear 'Patient Zero' From AIDS Origin Story". NPR.org.
- PMID 27783600.
- ^ a b UNAIDS, 2000
- S2CID 19384981.
- PMID 10462337.
- ^ UNAIDS, 2003 Archived 2007-06-14 at the Wayback Machine
- ^ "HHS, 2005" (PDF). Archived from the original (PDF) on 2017-10-04. Retrieved 2005-08-23.
- PMID 9516219.
- S2CID 32223916.
- S2CID 8167162.
- PMID 9952385.
- PMID 9809730.
- PMID 10889592.
- PMID 10102000.
- PMID 10909955.
- PMID 10770911.
- PMID 10509570.
- ^ "NIAID".
- S2CID 23141531.
- PMID 8093639.
- PMID 8099613.
- PMID 2240875.
- PMID 7992044.
- PMID 8353293.
- PMID 8093638.
- PMID 8563582.
- PMID 7915149.
- PMID 2477702.)
{{cite journal}}: CS1 maint: numeric names: authors list (link - ^ "U.S. Census Bureau".
- ^ "AIDS/HIV Statics".
- ^ "U.S. Bureau Census".
- ^ "UNAIDS, 2005" (PDF). Archived from the original (PDF) on 2013-12-02. Retrieved 2005-08-24.
- PMID 8174659.
- PMID 6295003.
- S2CID 4370482.
- ^ "USPHS/IDSA".
- S2CID 20186700.
- S2CID 7411052.
- PMID 18608078.
- S2CID 7339081.
- PMID 11740713.
