Nephrology
This article needs additional citations for verification. (June 2022) |
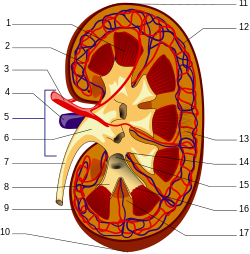 A human kidney (click on image for description). | |
| System | Urinary |
|---|---|
| Significant diseases | Hypertension, Kidney cancer |
| Significant tests | Kidney biopsy, Urinalysis |
| Specialist | Nephrologist |
| Glossary | Glossary of medicine |
| Occupation | |
|---|---|
| Names |
|
Occupation type | Specialty |
Activity sectors | Medicine |
| Description | |
Education required |
|
Fields of employment | Hospitals, Clinics |
Nephrology (from
Nephrology also studies systemic conditions that affect the kidneys, such as diabetes and autoimmune disease; and systemic diseases that occur as a result of kidney disease, such as renal osteodystrophy and hypertension. A physician who has undertaken additional training and become certified in nephrology is called a nephrologist.
The term "nephrology" was first used in about 1960, according to the French "néphrologie" proposed by Pr. Jean Hamburger in 1953, from the Greek νεφρός / nephrós (kidney). Before then, the specialty was usually referred to as "kidney medicine".[2]
Scope
Nephrology concerns the diagnosis and treatment of kidney diseases, including
Many diseases affecting the kidney are systemic disorders not limited to the organ itself, and may require special treatment. Examples include acquired conditions such as systemic vasculitides (e.g. ANCA vasculitis) and
Patients are referred to nephrology specialists after a urinalysis, for various reasons, such as
Nephrologist
A nephrologist is a
Nephrologists may further sub-specialise in
Procedures a nephrologist may perform include native kidney and transplant
Training
India
To become a nephrologist in India, one has to complete an
Australia and New Zealand
Nephrology training in Australia and New Zealand typically includes completion of a medical degree (
United Kingdom
In the United Kingdom, nephrology (often called renal medicine) is a subspecialty of general medicine. A nephrologist has completed medical school, foundation year posts (FY1 and FY2) and
United States
Nephrology training can be accomplished through one of two routes. The first path way is through an internal medicine pathway leading to an Internal Medicine/Nephrology specialty, and sometimes known as "adult nephrology". The second pathway is through
Diagnosis
Examination of the urine (
Basic blood tests can be used to check the concentration of
It is a good idea for patients with longterm kidney disease to know an up-to-date list of medications, and their latest blood tests, especially the blood creatinine level. In the United Kingdom, blood tests can monitored online by the patient, through a website called RenalPatientView.
More specialized tests can be ordered to discover or link certain systemic diseases to kidney failure such as infections (
).Structural abnormalities of the kidneys are identified with imaging tests. These may include
In certain circumstances, less invasive testing may not provide a certain diagnosis. Where definitive diagnosis is required, a
Treatment
Treatments in nephrology can include
When the kidneys are no longer able to sustain the demands of the body, end-stage kidney failure is said to have occurred. Without
Most kidney conditions are chronic conditions and so long term followup with a nephrologist is usually necessary. In the United Kingdom, care may be shared with the patient's primary care physician, called a General Practitioner (GP).
Organizations
The world's first society of nephrology was the French 'Societe de Pathologie Renale'. Its first president was Jean Hamburger, and its first meeting was in Paris in February 1949. In 1959, Hamburger also founded the 'Société de Néphrologie', as a continuation of the older society. It is now called Francophone Society of Nephrology, Dialysis and Transplantation (SFNDT). The second society of nephrologists, the UK Kidney Association (UKKA) was founded in 1950, originally named the Renal Association. Its first president was Arthur Osman and met for the first time, in London, on 30 March 1950. The Società di Nefrologia Italiana was founded in 1957 and was the first national society to incorporate the phrase nephrologia (or nephrology) into its name.
The word 'nephrology' appeared for the first time in a conference, on 1–4 September 1960 at the "Premier Congrès International de Néphrologie" in Evian and Geneva, the first meeting of the International Society of Nephrology (ISN, International Society of Nephrology). The first day (1.9.60) was in Geneva and the next three (2–4.9.60) were in Evian, France. The early history of the ISN is described by Robinson and Richet[10] in 2005 and the later history by Barsoum[11] in 2011. The ISN is the largest global society representing medical professionals engaged in advancing kidney care worldwide.[citation needed] It has an international office in Brussels, Belgium.[12]
In the US, founded in 1964, the National Kidney Foundation is a national organization representing patients and professionals who treat kidney diseases. Founded in 1966, the American Society of Nephrology (ASN) is the world's largest professional society devoted to the study of kidney disease. The American Nephrology Nurses' Association (ANNA), founded in 1969, promotes excellence in and appreciation of nephrology nursing to make a positive difference for patients with kidney disease. The American Association of Kidney Patients (AAKP) is a non-profit, patient-centric group focused on improving the health and well-being of CKD and dialysis patients. The National Renal Administrators Association (NRAA), founded in 1977, is a national organization that represents and supports the independent and community-based dialysis providers. The American Kidney Fund directly provides financial support to patients in need, as well as participating in health education and prevention efforts. ASDIN (American Society of Diagnostic and Interventional Nephrology) is the main organization of interventional nephrologists. Other organizations include CIDA, VASA etc. which deal with dialysis vascular access. The Renal Support Network (RSN) is a nonprofit, patient-focused, patient-run organization that provides non-medical services to those affected by chronic kidney disease (CKD).
In the United Kingdom, UK National Kidney Federation and Kidney Care UK (previously known as British Kidney Patient Association, BKPA)[13] represent patients, and the UK Kidney Association used to represent renal physicians and worked closely with a previous NHS policy directive called a National Service Framework for kidney disease.
References
- PMID 33713333.
- ^ Professor Priscilla Kincaid-Smith, nephrologist, Australian Academy of Science, Interview by Dr Max Blythe in 1998.
- ^ "Nephrology Specialty Description". American Medical Association.
- ^ "Nephrology". American College of Physicians.
- ^ "Dialysis". nhs.uk. 2017-10-19. Retrieved 2022-09-14.
- ^ "Kidney failure (ESRD) - Symptoms, causes and treatment options | American Kidney Fund". www.kidneyfund.org. 2021-11-17. Retrieved 2022-09-14.
- ^ "5 Reasons Why You May be Referred to a Nephrologist - Durham Nephrology Associates, PA". 2021-09-15. Retrieved 2022-09-13.
- ISSN 0085-2538.
- PMID 18417748.
- ^ "Kidney International - A Forty Year History 1960-2000". Archived from the original on 2011-08-10. Retrieved 2015-05-05.
- ^ [1] [dead link]
- ISSN 0085-2538.
- ^ "Homepage". Kidney Care UK. Retrieved 2017-12-12.
External links
- International Society of Nephrology (ISN)
- Nephromap Archived 2022-08-14 at the Wayback Machine
