Neurostimulation
| Neurostimulation | |
|---|---|
| OPS-301 code | 8-631 |
Neurostimulation is the purposeful modulation of the
Neurostimulation technology can improve the life quality of those who are severely paralyzed or have profound losses to various sense organs, as well as for permanent reduction of severe, chronic pain which would otherwise require constant (around-the-clock), high-dose opioid therapy (such as neuropathic pain and spinal-cord injury). It serves as the key part of
Brain stimulation
Brain stimulation has potentials to treat some disorders such as
Deep brain stimulation
Deep brain stimulation (DBS) has shown benefits for movement disorders such as
A DBS system consists of three components: the implanted pulse generator (IPG), the lead, and an extension. The implantable
The application and effects of DBS, on both normal and diseased brains, involves many parameters. These include the physiological properties of the brain tissue, which may change with disease state. Also important are the stimulation parameters, such as amplitude and temporal characteristics, and the geometric configuration of the electrode and the tissue that surrounds it.
In spite of a huge number of studies on DBS, its mechanism of action is still not well understood. Developing DBS microelectrodes is still challenging.[7]
Non-invasive of brain stimulation
Transcranial magnetic stimulation
Compared to electrical stimulation that utilizes brief, high-voltage electric shock to activate neurons, which can potentially activate pain fibers,

Transcranial electrical stimulation
This section needs expansion. You can help by adding to it. (April 2017) |
- Transcranial direct current stimulation(tDCS)
- Transcranial alternating current stimulation(tACS)
- Transcranial pulsed current stimulation (tPCS)
- Transcranial random noise stimulation (tRNS)
Spinal cord stimulation
Spinal cord stimulation for movement disorders
Spinal cord stimulation has shown promising results in spinal cord injury[12][13] and other movement disorders, such as multiple sclerosis.[14] The stimulation, applied over the lumbar spinal cord, works by activating large diameter afferent fibers entering the spinal cord,[15][16] which then transsynaptically activate and engage spinal neuronal networks.[17] The same target structures can also be activated by transcutaneous electrodes placed over the lower thoracic spine and abdomen.[18] Transcutaneous spinal cord stimulation is completely non-invasive and, as it uses TENS electrodes and stimulators, can be applied at low cost. Yet, in comparison to the implanted epidural variant, the efficacy of transcutaneous spinal cord stimulation depends on the body position and spinal alignment,[19][20] which could lead to inconsistent result if the body position and posture isn't controlled during the application.
Transcutaneous supraorbital nerve stimulation
Tentative evidence supports transcutaneous supraorbital nerve stimulation.[21] Side effects are few.[22]
Cochlear implants

Visual prosthesis

Theoretical and experimental clinical evidences suggest that direct electrical stimulation of the retina might be able to provide some vision to subjects who have lost the photoreceptive elements of their

LGN, which is located in the midbrain to relay signals from the retina to the visual cortex, is another potential area that can be used for stimulation. But this area has limited access due to surgical difficulty. The recent success of deep brain stimulation techniques targeting the midbrain has encouraged research to pursue the approach of LGN stimulation for a visual prosthesis.[33]
Cardiac electrostimulation devices
Stimulation microelectrode technologies

Microelectrodes are one of the key components of the neurostimulation, which deliver the current to neurons. Typical microelectrodes have three main components: a substrate (the carrier), a conductive metal layer, and an insulation material. In cochlear implants, microelectrodes are formed from
History
The primary findings about neurostimulation originated from the idea to stimulate nerves for therapeutic purposes. The 1st recorded use of electrical stimulation for pain relief goes back to 46 AD, when Scribonius Largus used torpedo fish (electric ray) for relieving headaches.[38] In the late 18th century, Luigi Galvani discovered that the muscles of dead frog legs twitched when struck by direct current on the nervous system.[39] The modulation of the brain activity by electrical stimulation of the motor cortex in dogs was shown in 1870 that resulted in limb movement.[40] From the late 18th century to today many milestones have been developed. Nowadays, sensory prosthetic devices, such as visual implants, cochlear implants, auditory midbrain implants, and spinal cord stimulators and also motor prosthetic devices, such as deep brain stimulators, Bion microstimulators, the brain control and sensing interface, and cardiac electro-stimulation devices are widely used.[11]
In 2013 the British pharmaceutical company
Research
In addition to the enormous usage of neurostimulation for clinical applications, it is also used widely in laboratories started dates back to 1920s by people like Delgado who used stimulation as an experimental manipulation to study basics of how the brain works. The primary works were on the reward center of the brain in which stimulation of those structures led to pleasure that requested more stimulation. Another most recent example is the electrical stimulation of the MT area of primary visual cortex to bias perception. In particular, the directionality of motion is represented in a regular way in the MT area. They presented monkeys with moving images on screen and monkey throughput was to determine what the direction is. They found that by systematically introducing some errors to the monkey's responses, by stimulating the MT area which is responsible for perceiving the motion in another direction, the monkey responded to somewhere in between the actual motion and the stimulated one. This was an elegant use of stimulation to show that MT area is essential in the actual perception of motion. Within the memory field, stimulation is used very frequently to test the strength of the connection between one bundle of cells to another by applying a small current in one cell which results in the release of neurotransmitters and measuring the postsynaptic potential.
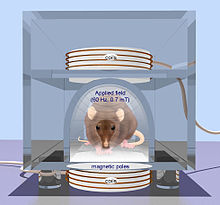
Generally, a short but high-frequency current in the range of 100 Hz helps strengthening the connection known as long-term potentiation. However, longer but low-frequency current tends to weaken the connections known as long-term depression.[45]
See also
References
- ^ S2CID 4413567.
- ^ Nitsche, Michael A.; Cohen, Leonardo G.; Wassermann, Eric M.; Priori, Alberto; Lang, Nicolas; Antal, Andrea; Paulus, Walter; Hummel, Friedhelm; Boggio, Paulo S.; Fregni, Felipe; Pascual-Leone, Alvaro (2008). "Transcranial direct current stimulation: State of the art 2008". Brain Stimulation 1 (3): 206–223.
- ^ Medtronic, Minneapolis, MN, U.S.A.
- PMID 20618409.
- S2CID 205683727.
- S2CID 14212180. Explained by Mohan, Geoffrey (September 4, 2013). "A window to the brain? It's here, says UC Riverside team". Los Angeles Times.
- S2CID 147427108.
- S2CID 41662030– via PubMed.
- S2CID 8035147.
- PMID 5320816.
- ^ ISBN 978-0387772608.
- S2CID 53148162.
- S2CID 198172141.
- PMID 33917893.
- S2CID 20180127.
- PMID 21401670.
- PMID 25582580.
- S2CID 26116191.
- PMID 26797502.
- PMID 34884249.
- S2CID 42537455.
- S2CID 6812366.
- S2CID 19339967.
- S2CID 7979564.
- S2CID 89621750.
- ^ P. Crosby, C. Daly, D. Money, and et al., Aug. 1985, " Cochlear implant system for an auditory prosthesis," United States Patent 4532930.
- S2CID 7525679.
- PMID 13258326.
- S2CID 21649550.
- S2CID 29334227.
- S2CID 22119389.
- ^ Sawan, Mohamad. "Curriculum Vitae".
- PMID 17452646.
- ^ Elmvquist R.; Senning A. (1960). "Implantable pacemaker for the heart". In Smyth CN (ed.). Medical electronics. Paris: Iliffe & Sons.
- ^ Warren J., Nelson J. (2000). "Pacemakers and ICD pulse generator circuitry". In Ellenbogen KA, Kay GN, Wilkoff BL (eds.). Clinical cardiac pacing and defibrillation (2nd ed.). Philadelphia: WB Saunders. pp. 194–216.
- ^ "Microelectrodes".
- ISBN 978-0123859068.
- S2CID 19217534.
- ^ Weisstein, Eric W. (2002). "Galvani, Luigi (1737–1798)". Eric Weisstein's World of Scientific Biography. Wolfram Research.
- ^ Fritsch G.; Hitzig E. (1870). "Uber die elektrische Erregbarkeit des Grosshirns". Arch. Anat. Physiol. 37: 300–332.
- ^ a b Moore, Samuel (29 May 2015). "The Vagus Nerve: A Back Door for Brain Hacking". IEEE Spectrum. Retrieved 4 June 2015.
- PMID 23579662.
- ^ Solon, Olivia (28 May 2013). "Electroceuticals: swapping drugs for devices". Wired UK.
- PMID 27542331.
- ^ Interview with Dr. J. Manns, Emory University, Oct. 2010
