Niacin
| |||
| Names | |||
|---|---|---|---|
| Pronunciation | /ˈnaɪəsɪn/ | ||
| Preferred IUPAC name
Pyridine-3-carboxylic acid[1] | |||
Other names
| |||
| Identifiers | |||
3D model (
JSmol ) |
|||
| 3DMet | |||
| 109591 | |||
| ChEBI | |||
| ChEMBL | |||
| ChemSpider | |||
| DrugBank | |||
ECHA InfoCard
|
100.000.401 | ||
| EC Number |
| ||
| 3340 | |||
IUPHAR/BPS |
|||
| KEGG | |||
| MeSH | Niacin | ||
PubChem CID
|
|||
RTECS number
|
| ||
| UNII | |||
CompTox Dashboard (EPA)
|
|||
| |||
| |||
| Properties | |||
| C6H5NO2 | |||
| Molar mass | 123.111 g·mol−1 | ||
| Appearance | White, translucent crystals | ||
| Density | 1.473 g cm−3 | ||
| Melting point | 237 °C; 458 °F; 510 K | ||
| 18 g L−1 | |||
| log P | 0.219 | ||
| Acidity (pKa) | 2.0, 4.85 | ||
| Isoelectric point | 4.75 | ||
Refractive index (nD)
|
1.4936 | ||
| 0.1271305813 D[citation needed] | |||
| Thermochemistry | |||
Std enthalpy of (ΔfH⦵298)formation |
−344.9 kJ mol−1 | ||
Std enthalpy of (ΔcH⦵298)combustion |
−2.73083 MJ mol−1 | ||
| Pharmacology | |||
| C04AC01 (WHO) C10BA01 (WHO) C10AD02 (WHO) C10AD52 (WHO) | |||
| License data |
| ||
| Intramuscular, by mouth | |||
| Pharmacokinetics: | |||
| 20–45 min | |||
| Hazards | |||
| GHS labelling: | |||

| |||
| Warning | |||
| H319 | |||
| P264, P280, P305+P351+P338, P337+P313, P501 | |||
| NFPA 704 (fire diamond) | |||
| Flash point | 193 °C (379 °F; 466 K) | ||
| 365 °C (689 °F; 638 K) | |||
Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa).
| |||
| Clinical data | |
|---|---|
| Trade names | Niacor, Niaspan, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682518 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | Intramuscular, by mouth |
| Legal status | |
| Legal status |
|
| Identifiers | |
ECHA InfoCard | 100.000.401 |
Niacin, also known as nicotinic acid, is an
The amide derivative
Niacin is also a prescription medication.
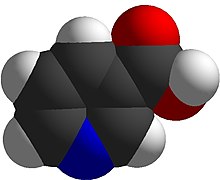
Niacin has the formula C
6H
5NO
2 and belongs to the group of the pyridinecarboxylic acids.[3] As the precursor for nicotinamide adenine dinucleotide and nicotinamide adenine dinucleotide phosphate, niacin is involved in DNA repair.[19]
Definition
Niacin is both a vitamin, i.e., an essential nutrient, marketed as a dietary supplement, and in the US, a prescription medicine. As a vitamin, it is precursor of the coenzymes nicotinamide adenine dinucleotide (NAD) and nicotinamide adenine dinucleotide phosphate (NADP). These compounds are coenzymes for many dehydrogenases, participating in many hydrogen transfer processes. NAD is important in catabolism of fat, carbohydrate, protein, and alcohol, as well as cell signaling and DNA repair, and NADP mostly in anabolism reactions such as fatty acid and cholesterol synthesis.[20] Vitamin intake recommendations made by several countries are that intakes of 14–18 mg/day are sufficient to meet the needs of healthy adults.[4][21][22] Niacin but also nicotinamide (niacinamide) are used for prevention and treatment of pellagra, a disease caused by lack of the vitamin.[6][20] When niacin is used as a medicine to treat elevated cholesterol and triglycerides, daily doses range from 500 to 3,000 mg/day.[23][24] High-dose nicotinamide does not have this medicinal effect.[20]
Vitamin deficiency

Severe deficiency of niacin in the diet causes the disease pellagra, characterized by diarrhea, sun-sensitive dermatitis involving hyperpigmentation and thickening of the skin (see image), inflammation of the mouth and tongue, delirium, dementia, and if left untreated, death.[6] Common psychiatric symptoms include irritability, poor concentration, anxiety, fatigue, loss of memory, restlessness, apathy, and depression.[20] The biochemical mechanism(s) for the observed deficiency-caused neurodegeneration are not well understood, but may rest on: A) the requirement for nicotinamide adenine dinucleotide (NAD+) to suppress the creation of neurotoxic tryptophan metabolites, B) inhibition of mitochondrial ATP generation, resulting in cell damage; C), activation of the poly (ADP-ribose) polymerase (PARP) pathway, as PARP is a nuclear enzyme involved in DNA repair, but in the absence of NAD+ can lead to cell death; D) reduced synthesis of neuro-protective brain-derived neurotrophic factor or its receptor tropomyosin receptor kinase B; or E) changes to genome expression directly due to the niacin deficiency.[25]
Niacin deficiency is rarely seen in developed countries, and it is more typically associated with poverty, malnutrition or malnutrition secondary to chronic alcoholism.[26] It also tends to occur in less developed areas where people eat maize (corn) as a staple food, as maize is the only grain low in digestible niacin. A cooking technique called nixtamalization i.e., pretreating with alkali ingredients, increases the bioavailability of niacin during maize meal/flour production.[27] For this reason, people who consume maize as tortillas or hominy are at less risk of niacin deficiency.
For treating deficiency, the World Health Organization (WHO) recommends administering niacinamide i.e., nicotinamide, instead of niacin, to avoid the flushing side effect commonly caused by the latter. Guidelines suggest using 300 mg/day for three to four weeks.[10] Dementia and dermatitis show improvement within a week. Because deficiencies of other B-vitamins may be present, the WHO recommends a multi-vitamin in addition to the niacinamide.[10]
Measuring vitamin status
Plasma concentrations of niacin and niacin metabolites are not useful markers of niacin status.[4] Urinary excretion of the methylated metabolite N1-methyl-nicotinamide is considered reliable and sensitive. The measurement requires a 24-hour urine collection. For adults, a value of less than 5.8 μmol/day represent deficient niacin status and 5.8 to 17.5 μmol/day represents low.[4] According to the World Health Organization, an alternative mean of expressing urinary N1-methyl-nicotinamide is as mg/g creatinine in a 24-hour urine collection, with deficient defined as <0.5, low 0.5-1.59, acceptable 1.6-4.29, and high >4.3[10] Niacin deficiency occurs before the signs and symptoms of pellagra appear.[4] Erythrocyte nicotinamide adenine dinucleotide (NAD) concentrations potentially provide another sensitive indicator of niacin depletion, although definitions of deficient, low and adequate have not been established. Lastly, plasma tryptophan decreases on a low niacin diet because tryptophan converts to niacin. However, low tryptophan could also be caused by a diet low in this essential amino acid, so it is not specific to confirming vitamin status.[4]
Dietary recommendations
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
The U.S. Institute of Medicine (renamed
The European Food Safety Authority (EFSA) refers to the collective set of information as Dietary Reference Values (DRV), with Population Reference Intake (PRI) instead of RDA, and Average Requirement instead of EAR. For the EU, AIs and ULs have the same definition as in the US, except that units are milligrams per megajoule (MJ) of energy consumed rather than mg/day. For women (including those pregnant or lactating), men and children the PRI is 1.6 mg per megajoule. As the conversion is 1 MJ = 239 kcal, an adult consuming 2390 kilocalories should be consuming 16 mg niacin. This is comparable to US RDAs (14 mg/day for adult women, 16 mg/day for adult men).[21]
ULs are established by identifying amounts of vitamins and minerals that cause adverse effects, and then selecting as an upper limit amounts that are the "maximum daily intake unlikely to cause adverse health effects."[31] Regulatory agencies from different countries do not always agree. For the US, 30 or 35 mg for teenagers and adults, less for children.[4] The EFSA UL for adults is set at 10 mg/day - about one-third of the US value. For all of the government ULs, the term applies to niacin as a supplement consumed as one dose, and is intended as a limit to avoid the skin flush reaction. This explains why for EFSA, the recommended daily intake can be higher than the UL.[32]
Both the DRI and DRV describe amounts needed as niacin equivalents (NE), calculated as 1 mg NE = 1 mg niacin or 60 mg of the essential amino acid tryptophan. This is because the amino acid is utilized to synthesize the vitamin.[4][21]
For U.S. food and dietary supplement labeling purposes the amount in a serving is expressed as a percent of
Sources
Niacin is found in a variety of
| Source[38] | Amount (mg / 100g) |
|---|---|
| Nutritional yeast[39] Serving = 2 Tbsp (16 g) contains 56 mg |
350 |
| Tuna, yellowfin | 22.1 |
| Peanuts | 14.3 |
| Peanut butter | 13.1 |
| Bacon | 10.4 |
| Tuna, light, canned | 10.1 |
| Salmon | 10.0 |
| Turkey depending on what part, how cooked | 7-12 |
| Chicken depending on what part, how cooked | 7-12 |
| Source[38] | Amount (mg / 100g) |
|---|---|
| Beef depending on what part, how cooked | 4-8 |
| Pork depending on what part, how cooked | 4-8 |
Sunflower seeds |
7.0 |
| Tuna, white, canned | 5.8 |
| Almonds | 3.6 |
| Mushrooms, white | 3.6 |
| Cod fish | 2.5 |
| Rice, brown | 2.5 |
| Hot dogs | 2.0 |
| Source[38] | Amount (mg / 100g) |
|---|---|
| Avocado | 1.7 |
| Potato, baked, with skin | 1.4 |
| Maize (corn) | 1.0 |
| Rice, white | 0.5 |
| Kale | 0.4 |
Eggs |
0.1 |
| Milk | 0.1 |
| Cheese | 0.1 |
| Tofu | 0.1 |
Vegetarian and vegan diets can provide adequate amounts if products such as nutritional yeast, peanuts, peanut butter, tahini, brown rice, mushrooms, avocado and sunflower seeds are included. Fortified foods and dietary supplements can also be consumed to ensure adequate intake.[5][40]
Food preparation
Niacin naturally found in food is susceptible to destruction from high heat cooking, especially in the presence of acidic foods and sauces. It is soluble in water, and so may also be lost from foods boiled in water.[41]
Food fortification
Countries fortify foods with nutrients to address known deficiencies.[7] As of 2020, 54 countries required food fortification of wheat flour with niacin or niacinamide; 14 also mandate fortification of maize flour, and 6 mandate fortification of rice.[42] From country to country, niacin fortification ranges from 1.3 to 6.0 mg/100 g.[42]
As a dietary supplement
In the United States, niacin is sold as a non-prescription dietary supplement with a range of 100 to 1000 mg per serving. These products often have a Structure/Function health claim[43] allowed by the US Food & Drug Administration (FDA). An example would be "Supports a healthy blood lipid profile." The American Heart Association strongly advises against the substitution of dietary supplement niacin for prescription niacin because of potentially serious side effects, which means that niacin should only be used under the supervision of a health care professional, and because manufacture of dietary supplement niacin is not as well-regulated by the FDA as prescription niacin.[44] More than 30 mg niacin consumed as a dietary supplement can cause skin flushing. Face, arms and chest skin turns a reddish color because of vasodilation of small subcutaneous blood vessels, accompanied by sensations of heat, tingling and itching. These signs and symptoms are typically transient, lasting minutes to hours; they are considered unpleasant rather than toxic.[5]
As lipid-modifying medication
In the United States, prescription niacin, in immediate-release and slow-release forms, is used to treat primary hyperlipidemia and hypertriglyceridemia.[23][24] It is used either as a monotherapy or in combination with other lipid-modifying drugs. Dosages start at 500 mg/day and are often gradually increased to as high as 3000 mg/day for immediate release or 2000 mg/day for slow release (also referred to as sustained release) to achieve the targeted lipid changes (lower LDL-C and triglycerides, and higher HDL-C).[23][24] Prescriptions in the US peaked in 2009, at 9.4 million[citation needed] and had declined to 800 thousand by 2020.[18]
Systematic reviews found no effect of prescription niacin on all-cause mortality, cardiovascular mortality, myocardial infarctions, nor fatal or non-fatal strokes despite raising HDL cholesterol.[12][45] Reported side effects include an increased risk of new-onset type 2 diabetes.[14][16][17][46]
Mechanisms
Niacin reduces synthesis of low-density lipoprotein cholesterol (LDL-C), very low-density lipoprotein cholesterol (VLDL-C),
The mechanism behind niacin increasing HDL-C is not totally understood, but seems to occur in various ways. Niacin increases
Combined with statins
Extended release niacin was combined with lovastatin (Advicor), and with simvastatin (Simcor), as prescription drug combinations. The combination niacin/lovastatin was approved by the U.S. Food and Drug Administration (FDA) in 2001.[57] The combination niacin/simvastatin was approved by the FDA in 2008.[58][59] Subsequently, large outcome trials using these niacin and statin therapies were unable to demonstrate incremental benefit of niacin beyond statin therapy alone.[60] The FDA withdrew approval of both drugs in 2016. The reason given: "Based on the collective evidence from several large cardiovascular outcome trials, the Agency has concluded that the totality of the scientific evidence no longer supports the conclusion that a drug-induced reduction in triglyceride levels and/or increase in HDL-cholesterol levels in statin-treated patients results in a reduction in the risk of cardiovascular events." The drug company discontinued the drugs.[61]
Contraindications
Prescription immediate release (Niacor) and extended release (Niaspan) niacin are
Adverse effects
The most common adverse effects of medicinal niacin (500–3000 mg) are flushing (e.g., warmth, redness, itching or tingling) of the face, neck and chest, headache, abdominal pain, diarrhea,
The acute adverse effects of high-dose niacin therapy (1–3 grams per day) – which is commonly used in the treatment of
Flushing
Prevention of flushing requires altering or blocking the prostaglandin-mediated pathway.[5][67] Aspirin taken half an hour before the niacin prevents flushing, as does ibuprofen. Taking niacin with meals also helps reduce this side effect.[5] Acquired tolerance will also help reduce flushing; after several weeks of a consistent dose, most people no longer experience flushing.[5] Slow- or "sustained"-release forms of niacin have been developed to lessen these side effects.[68][69]
Liver damage
Niacin in medicinal doses can cause modest elevations in serum transaminase and unconjugated bilirubin, both biomarkers of liver injury. The increases usually resolve even when drug intake is continued.[15][70][71] However, less commonly, the sustained release form of the drug can lead to serious hepatotoxicity, with onset in days to weeks. Early symptoms of serious liver damage include nausea, vomiting and abdominal pain, followed by jaundice and pruritus. The mechanism is thought to be a direct toxicity of elevated serum niacin. Lowering dose or switching to the immediate release form can resolve symptoms. In rare instances the injury is severe, and progresses to liver failure.[15]
Diabetes
The high doses of niacin used to treat
Other adverse effects
High doses of niacin can also cause niacin maculopathy, a thickening of the macula and retina, which leads to blurred vision and blindness. This maculopathy is reversible after niacin intake ceases.[72] Niaspan, the slow-release product, has been associated with a reduction in platelet content and a modest increase in prothrombin time.[24]
Pharmacology
Pharmacodynamics
Activating HCA2 has effects other than lowering serum cholesterol and triglyceride concentrations: antioxidative, anti-inflammatory, antithrombotic, improved endothelial function and plaque stability, all of which counter development and progression of atherosclerosis.[73][74]
Niacin
Pharmacokinetics
Both niacin and niacinamide are rapidly absorbed from the stomach and small intestine.[77] Absorption is facilitated by sodium-dependent diffusion, and at higher intakes, via passive diffusion. Unlike some other vitamins, the percent absorbed does not decrease with increasing dose, so that even at amounts of 3-4 grams, absorption is nearly complete.[20] With a one gram dose, peak plasma concentrations of 15 to 30 μg/mL are reached within 30 to 60 minutes. Approximately 88% of an oral pharmacologic dose is eliminated by the kidneys as unchanged niacin or nicotinuric acid, its primary metabolite. The plasma elimination half-life of niacin ranges from 20 to 45 minutes.[23]
Niacin and nicotinamide are both converted into the

Production
Biosynthesis
In addition to absorbing niacin from diet, niacin can be synthesized from the essential amino acid tryptophan, a five-step process with the penultimate compound being quinolinic acid (see figure). Some bacteria and plants utilize aspartic acid in a pathway that also goes to quinolinic acid.[80] For humans, the efficiency of conversion is estimated as requiring 60 mg of tryptophan to make 1 mg of niacin. Riboflavin, vitamin B6 and iron are required for the process.[20] Pellagra is a consequence of a corn-dominant diet because the niacin in corn is poorly bioavailable and corn proteins are low in tryptophan compared to wheat and rice proteins.[81]
Industrial synthesis
Nicotinic acid was first synthesized in 1867 by oxidative degradation of
The demand for commercial production includes for animal feed and for food fortification meant for human consumption. According to Ullmann's Encyclopedia of Industrial Chemistry, worldwide 31,000 tons of nicotinamide were sold in 2014.[82]
Climate Impact
The production of niacin creates nitrous oxide as a by-product, which is a potent greenhouse gas. In 2018, it was discovered that a niacin factory in Visp, Switzerland, was responsible for around one percent of the country's greenhouse gas emissions. Eventually, catalytic scrubbing technology that avoids most of the emissions was installed in 2021.[87]
Chemistry
This colorless, water-soluble solid is a derivative of
2).[20]
Preparations
Niacin is incorporated into multi-vitamin and sold as a single-ingredient dietary supplement. The latter can be immediate or slow release.[88]
Nicotinamide (niacinamide) is used to treat niacin deficiency because it does not cause the flushing adverse reaction seen with niacin. Nicotinamide may be toxic to the liver at doses exceeding 3 g/day for adults.[89]
Prescription products can be immediate release (Niacor, 500 mg tablets) or
Prescription niacin preparations in combination with statin drugs (discontinued) are described above. A combination of niacin and laropiprant had been approved for use in Europe and marketed as Tredaptive. Laropiprant is a prostaglandin D2 binding drug shown to reduce niacin-induced vasodilation and flushing side effects.[47][92][93] A clinical trial showed no additional efficacy of Tredaptive in lowering cholesterol when used together with other statin drugs, but did show an increase in other side effects.[94] The study resulted in the withdrawal of Tredaptive from the international market.[95][96]

One form of dietary supplement sold in the US is inositol hexanicotinate (IHN), also called inositol nicotinate. This is inositol that has been esterified with niacin on all six of inositol's alcohol groups.[97] IHN is usually sold as "flush-free" or "no-flush" niacin in units of 250, 500, or 1000 mg/tablets or capsules. In the US, it is sold as an over-the-counter formulation, and often is marketed and labeled as niacin, thus misleading consumers into thinking they are getting an active form of the medication. While this form of niacin does not cause the flushing associated with the immediate-release products, there is not enough evidence to recommend IHN to treat hyperlipidemia.[98]
History
Niacin as a chemical compound was first described by chemist Hugo Weidel in 1873 in his studies of nicotine,[99] but that predated by many years the concept of food components other than protein, fat and carbohydrates that were essential for life. Vitamin nomenclature was initially alphabetical, with Elmer McCollum calling these fat-soluble A and water-soluble B.[100] Over time, eight chemically distinct, water-soluble B vitamins were isolated and numbered, with niacin as vitamin B3.[100]
Corn (maize) became a staple food in the southeast United States and in parts of Europe. A disease that was characterized by dermatitis of sunlight-exposed skin was described in Spain in 1735 by Gaspar Casal. He attributed the cause to poor diet.[101] In northern Italy it was named "pellagra" from the Lombard language (agra = holly-like or serum-like; pell = skin).[102][103] In time, the disease was more closely linked specifically to corn.[104] In the US, Joseph Goldberger was assigned to study pellagra by the Surgeon General of the United States. His studies confirmed a corn-based diet as the culprit, but he did not identify the root cause.[105][106]
Nicotinic acid was extracted from liver by biochemist Conrad Elvehjem in 1937. He later identified the active ingredient, referring to it as "pellagra-preventing factor" and the "anti-blacktongue factor."[107] It was also referred to as "vitamin PP", "vitamin P-P" and "PP-factor", all derived from the term "pellagra-preventive factor".[10] In the late 1930s, studies by Tom Douglas Spies, Marion Blankenhorn, and Clark Cooper confirmed that niacin cured pellagra in humans. The prevalence of the disease was greatly reduced as a result.[108]
Nicotinic acid was initially synthesized by oxidizing
Carpenter found in 1951, that niacin in corn is biologically unavailable, and can be released only in very alkaline lime water of pH 11. This explains why a Latin-American culture that used alkali-treated cornmeal to make tortilla was not at risk for niacin deficiency.[110]
In 1955, Altschul and colleagues described large amounts of niacin as having a lipid-lowering property.[111] As such, niacin is the oldest known lipid-lowering drug.[112] Lovastatin, the first 'statin' drug, was first marketed in 1987.[113]
Research
In
References
- ISBN 978-0-85404-182-4.
- ^ "Niacin Use During Pregnancy". Drugs.com. 29 July 2019. Archived from the original on 5 August 2020. Retrieved 4 May 2020.
- ^ a b c d e f g h i j k "Niacin". Micronutrient Information Center, Linus Pauling Institute, Oregon State University, Corvallis, OR. 8 October 2018. Archived from the original on 12 September 2019. Retrieved 16 September 2019.
- ^ ISBN 978-0-309-06554-2. Archivedfrom the original on 1 September 2018. Retrieved 29 August 2018.
- ^ a b c d e f g h i j k l m n "Niacin Fact Sheet for Health Professionals". Office of Dietary Supplements, US National Institutes of Health. 3 June 2020. Archived from the original on 23 June 2020. Retrieved 29 June 2020.
- ^ S2CID 33877664.
- ^ a b "Why fortify?". Food Fortification Initiative. 2017. Archived from the original on 4 April 2017. Retrieved 4 April 2017.
- PMID 1393911.
- from the original on 4 August 2020. Retrieved 3 July 2019.
- ^ hdl:10665/66704. WHO/NHD/00.10.
- ^ a b "Niacin". Drugs.com. 16 March 2019. Archived from the original on 9 June 2020. Retrieved 27 April 2020.
- ^ PMID 25038074.
- PMID 20079494.
- ^ PMID 28616955.
- ^ PMID 31643504.
- ^ from the original on 28 June 2020. Retrieved 27 June 2020.
- ^ PMID 26370223.
- ^ a b "Niacin - Drug Usage Statistics". ClinCalc. Archived from the original on 8 July 2020. Retrieved 7 October 2022.
- PMID 26828517.
- ^ ISBN 978-0-323-66162-1.
- ^ a b c "Overview on Dietary Reference Values for the EU population as derived by the EFSA Panel on Dietetic Products, Nutrition and Allergies" (PDF). 2017. Archived (PDF) from the original on 28 August 2017. Retrieved 31 August 2017.
- ^ a b c "Nutrient reference values for Australia and New Zealand" (PDF). National Health and Medical Research Council. 9 September 2005. Archived from the original (PDF) on 21 January 2017. Retrieved 19 June 2018.
- ^ a b c d e f "NIACOR-niacin tablet". DAILYMED, US National Library of Medicine. March 2020. Archived from the original on 9 August 2020. Retrieved 9 May 2020.
- ^ a b c d e f g "Niaspan Patient Package and Product Information (PPPI)" (PDF). December 2018. Archived (PDF) from the original on 9 October 2022. Retrieved 9 May 2020.
- PMID 25317166.
- S2CID 29070525. Archived from the originalon 10 July 2012. Retrieved 27 November 2009.
- ^ Bressani R, Gomez-Brenes R, Scrimshaw NS (1961). "Effect of processing on distribution and in vitro availability of niacin of corn (Zea mays)". Food Technol. 15: 450–4.
- ^ a b LaRosa CJ (January 2020). "Hartnup Disease". Archived from the original on 8 July 2020. Retrieved 6 July 2020.
- ^ a b Health Canada (20 July 2005). "Dietary Reference Intakes". Government of Canada. Archived from the original on 14 June 2018. Retrieved 20 June 2018.
- ^ a b c "Tolerable Upper Intake Levels for Vitamins and Minerals" (PDF). European Food Safety Authority. February 2006. Archived (PDF) from the original on 16 March 2016. Retrieved 18 June 2018.
- ^ a b "Nutrient Recommendations: Dietary Reference Intakes (DRI)". National Institutes of Health, Office of Dietary Supplements. Archived from the original on 2 July 2020. Retrieved 30 June 2020.
- ^ "Tolerable Upper Intake Levels For Vitamins And Minerals" (PDF). European Food Safety Authority. 2006. Archived (PDF) from the original on 16 March 2016. Retrieved 9 March 2016.
- ^ "Federal Register May 27, 2016 Food Labeling: Revision of the Nutrition and Supplement Facts Labels" (PDF). Archived (PDF) from the original on 9 October 2022.
- ^ "Daily Value Reference of the Dietary Supplement Label Database (DSLD)". Dietary Supplement Label Database (DSLD). Archived from the original on 7 April 2020. Retrieved 16 May 2020.
- ^ "Changes to the Nutrition Facts Label". U.S. Food and Drug Administration (FDA). 27 May 2016. Archived from the original on 6 May 2018. Retrieved 16 May 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ "Industry Resources on the Changes to the Nutrition Facts Label". U.S. Food and Drug Administration (FDA). 21 December 2018. Archived from the original on 25 December 2020. Retrieved 16 May 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ "Niacin content per 100 grams; select food subset, abridged list by food groups". United States Department of Agriculture, Agricultural Research Service, USDA Branded Food Products Database v.3.6.4.1. 17 January 2017. Archived from the original on 2 February 2017. Retrieved 23 January 2017.
- ^ a b c "USDA National Nutrient Database for Standard Reference Legacy: Niacin" (PDF). U.S. Department of Agriculture, Agricultural Research Service. 2018. Archived (PDF) from the original on 9 October 2022. Retrieved 12 May 2020.
- ^ "Nutritional Yeast Flakes (two tablespoons = 16 grams". NutritionData.Self.com. Archived from the original on 11 April 2020. Retrieved 13 May 2020.
- ^ "Vitamin B3 (Niacin)". VivaHealth.org. 2000. Archived from the original on 4 August 2020. Retrieved 12 May 2020.
- ^ "Effects of Cooking on Vitamins (Table)". Beyondveg. Archived from the original on 16 October 2012. Retrieved 30 April 2019.
- ^ a b "Map: Count of Nutrients In Fortification Standards". Global Fortification Data Exchange. Archived from the original on 11 April 2019. Retrieved 4 July 2020.
- ^ "Structure/Function Claims". U.S. Food & Drug Administration. December 2017. Archived from the original on 10 June 2020. Retrieved 30 June 2020.
- ^ "Cholesterol Medications". American Heart Association. 10 November 2018. Archived from the original on 5 April 2020. Retrieved 8 May 2020.
- PMID 26048725.
- PMID 27793642.
- ^ S2CID 27925461.
- PMID 12646212.
- PMID 12522134.
- PMID 17705685.
- S2CID 205536280.
- ^ PMID 20227438.
- PMID 20889132.
- S2CID 27918392.
- S2CID 22526314.
- PMID 15037193.
- ^ "Drug Approval Package: Advicor (Niacin Extended-Release & Lovastatin) NDA #21-249". U.S. Food and Drug Administration (FDA). 13 September 2002. Archived from the original on 4 August 2020. Retrieved 17 May 2020.
- ^ "Drug Approval Package: Simcor (Niacin/Simvastatin) NDA #022078". U.S. Food and Drug Administration (FDA). 31 July 2008. Archived from the original on 14 November 2022. Retrieved 14 November 2022.
- ^ "Drugs.com, Abbott Receives FDA Approval for Simcor (Niaspan / simvastatin), a Novel Combination Medicine for Comprehensive Cholesterol Management" (Press release). Archived from the original on 5 August 2020. Retrieved 15 March 2008.
- PMID 26073392.
- ^ "AbbVie Inc.; Withdrawal of Approval of New Drug Applications for Advicor and Simcor". U.S. Federal Register. 18 April 2016. Archived from the original on 5 August 2020. Retrieved 17 May 2020.
- ^ a b c d e "Niaspan- niacin tablet, film coated, extended release". DailyMed. 20 August 2013. Archived from the original on 14 November 2022. Retrieved 14 November 2022.
- ^ S2CID 5609632.
- PMID 16322797.
- S2CID 30199951.
- PMID 17008871.
- PMID 18375237.
- ISBN 978-0-07-145153-6.
- .
- ^ PMID 1853497.
- ^ PMID 7286783.
- PMID 26060832.
- PMID 26210594.
- PMID 20167660.
- PMID 15081432.
- ISBN 9781416034308.
- PMID 21749321.
- ISBN 978-1-57259-153-0.
- PMID 7229643.
- PMID 6997723.
- PMID 6357846.
- ^ ISBN 978-3-527-30385-4.
- ^ .
- ISBN 978-3527306732.
- S2CID 100485418.
- ISSN 0009-2347.
- ^ Lenz, Christoph (2021), "The climate disgrace of Visp", European Press Prize, archived from the original on 8 September 2023, retrieved 8 September 2023
- PMID 22385545.
- PMID 11126400.
- PMID 21414665.
- PMID 20562093.
- S2CID 2126240.
- PMID 19031552.
- S2CID 23548060.
- ^ Nainggolan L (11 January 2013). "Niacin/Laropiprant Products to Be Suspended Worldwide". Medscape. Archived from the original on 26 April 2015. Retrieved 20 February 2017.
- ^ "Merck begins overseas recall of HDL cholesterol drug". Reuters. 11 January 2013. Archived from the original on 21 April 2023. Retrieved 6 July 2021.
- ^ Aguilar F, Charrondiere UR, Dusemund B, Galtier PM, Gilbert J, et al. (January 2009). "Inositol hexanicotinate (inositol hexaniacinate) as a source of niacin (vitamin B3) added for nutritional purposes in food supplements". The EFSA Journal. 949: 1–20. Archived from the original on 5 March 2017. Retrieved 4 March 2017.
- ^ Taheri (15 January 2003). "No-Flush Niacin for the Treatment of Hyperlipidemia". Medscape. Archived from the original on 5 December 2008. Retrieved 31 March 2008.
- from the original on 4 August 2020. Retrieved 3 July 2019.
- ^ ISBN 978-0-080-56130-1. Archivedfrom the original on 13 January 2023. Retrieved 30 June 2020.
- ^ Casal G (1945). "The natural and medical history of the principality of the Asturias". In Major RH (ed.). Classic Descriptions of Disease (3rd ed.). Springfield: Charles C Thomas. pp. 607–12.
- ^ F. Cherubini, Vocabolario Milanese-Italiano, Imp. Regia Stamperia, 1840-43, vol. I, III.
- ^ "Definition of Pellagra". MedicineNet.com. Archived from the original on 30 September 2007. Retrieved 18 June 2007.
- ^ Cesare Lombroso, Studi clinici ed esperimentali sulla natura, causa e terapia delle pellagra (Bologna: Fava e Garagnani, 1869)
- S2CID 13226008.
- ^ Kraut A. "Dr. Joseph Goldberger and the War on Pellagra | Ashes on the Potomac". history.nih.gov. Archived from the original on 9 May 2020. Retrieved 20 February 2017.
- (PDF) from the original on 9 October 2022.
- ISBN 978-0-9710541-9-6"Men of the Year, outstanding in comprehensive science were three medical researchers who discovered that nicotinic acid was a cure for human pellagra: Drs. Tom Douglas Spies of Cincinnati General Hospital, Marion Arthur Blankenhorn of the University of Cincinnati, Clark Niel Cooper of Waterloo, Iowa."
- .
- PMID 14880960.
- PMID 14350806.
- PMID 30782960.
- PMID 12602122.
- PMID 25766751.
- PMID 23526298.
- PMID 26773933.
- S2CID 29760853.
- PMID 24662263.



