Nonbenzodiazepine
Nonbenzodiazepines (
Nonbenzodiazepine
Classes

Currently, the major chemical classes of nonbenzodiazepines are:
- Alpidem
- Necopidem
- Saripidem
- Zolpidem (Ambien, Ambien CR, Intermezzo, Zolpimist, Edluar, Ivadal, Sanval, Stilnox, etc.)
- Divaplon
- Fasiplon
- Indiplon
- Lorediplon
- Ocinaplon
- Panadiplon
- Taniplon
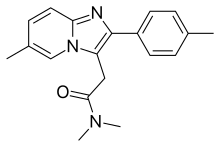
- Zaleplon (Sonata, Starnoc, Andante)
|
|
|
|
Others |
|
|
Pharmacology
The nonbenzodiazepines are
Background
Nonbenzodiazepines have demonstrated efficacy in treating
Pharmaceuticals
| Comparison of nonbenzodiazepines[10][11] | ||||
|---|---|---|---|---|
| Drug | Reduces sleep onset latency? | Encourages sleep maintenance? | Observed causing rebound insomnia ?
|
Observed causing physical dependence? |
| Zolpidem instant-release | Yes | Maybe | Maybe | Yes |
| Zolpidem extended-release | Yes | Yes | Yes | Yes |
| Sublingual zolpidem | Yes | Maybe | Maybe | Yes |
| Zolpidem oral spray | Yes | Maybe | Maybe | Yes |
| Eszopiclone | Yes | Yes | Yes | Yes |
| Zaleplon | Yes | Maybe | No | Yes |
The first three nonbenzodiazepine drugs to enter the market were the "Z-drugs", zopiclone, zolpidem and zaleplon. These three drugs are all
Long-term use is not recommended as tolerance and addiction can occur.[16] A survey of patients using nonbenzodiazepine Z-drugs and benzodiazepine hypnotic users found that there was no difference in reports of adverse effects that were reported in over 41% of users and, in fact, Z-drug users were more likely to report that they had tried to quit their hypnotic drug and were more likely to want to stop taking Z-drugs than benzodiazepine users. Efficacy also did not differ between benzodiazepine and Z-drug users.[17]
Effectiveness
A major
Side effects
The Z-drugs are not without disadvantages, and all three compounds are notable for producing side effects such as pronounced
Daytime withdrawal-related anxiety can also occur from chronic nightly nonbenzodiazepine hypnotic usage such as with zopiclone.[26]
Side effects can differ within the drug class due to differences in metabolism and pharmacology. For example, long-acting benzodiazepines have problems of drug accumulation especially in the elderly or those with liver disease, and shorter-acting benzodiazepines have a higher risk of more severe withdrawal symptoms.
Increased risk of depression
It has been claimed that insomnia causes
Other risks
Sleeping pills, including the Z-drugs, have been associated with an increased risk of death.[34]
In older people this family of medications increases the risk of
The Z-drug zaleplon may have fewer side effects compared to benzodiazepines.[36]
Dependence and withdrawal management
Nonbenzodiazepines should not be discontinued abruptly if taken for more than a few weeks due to the risk of
Elderly
Nonbenzodiazepine hypnotic drugs, similar to benzodiazepines, cause impairments in body balance and standing steadiness upon waking; falls and hip fractures are frequently reported. The combination with alcohol increases these impairments. Partial but incomplete tolerance develops to these impairments.[40] In general, nonbenzodiazepines are not recommended for older patients due to the increased risk of falls and fractures.[41] An extensive review of the medical literature regarding the management of insomnia and the elderly found that there is considerable evidence of the effectiveness and lasting benefits of non-drug treatments for insomnia in adults of all age groups and that these interventions are underused. Compared with the benzodiazepines, the nonbenzodiazepine sedative-hypnotics offer little if any advantages in efficacy or tolerability in elderly persons. It was found that newer agents such as the melatonin agonists may be more suitable and effective for the management of chronic insomnia in elderly people. Long-term use of sedative-hypnotics for insomnia lacks an evidence base and is discouraged for reasons that include concerns about such potential adverse drug effects as cognitive impairment (anterograde amnesia), daytime sedation, motor incoordination, and increased risk of motor vehicle accidents and falls. In addition, the effectiveness and safety of long-term use of these agents remain to be determined. It was concluded that further research is needed to evaluate the long-term effects of treatment and the most appropriate management strategy for elderly persons with chronic insomnia.[42]
Safety
A review of the literature regarding hypnotics including the nonbenzodiazepine Z-drugs concluded that these drugs carry a significant risk to the individual. The risks include dependence, accidents, and other adverse effects. Gradual discontinuation of hypnotics may lead to improved health without worsening of sleep. It is preferred that they should be prescribed for only a few days at the lowest effective dose and avoided wherever possible in the elderly.[43]
New compounds
More recently, a range of non-sedating anxiolytic drugs derived from the same structural families as the Z-drugs have been developed, such as alpidem (Ananxyl) and pagoclone, and approved for clinical prescription. Nonbenzodiazepine drugs are much more selective than the older benzodiazepine anxiolytics, producing effective relief of anxiety/panic with little or no sedation, anterograde amnesia, or anticonvulsant effects, and are thus potentially more precise than older, anti-anxiety drugs. However, anxiolytic nonbenzodiazepines are not widely prescribed and many have collapsed after initial clinical trials and consumption halted many projects, including but not limited to alpidem, indiplon, and suriclone.
History
Z-drugs emerged in the last years of the 1980s and early 1990s, with
References
- OxfordDictionaries.com. Archived from the originalon August 28, 2012. Retrieved 2016-01-20.
- ^ "benzodiazepine". Merriam-Webster.com Dictionary.
- S2CID 40188442.
- PMID 22981367.
- PMID 17132386.
- S2CID 34250754.
- ISBN 978-1-4557-0318-0, retrieved 2023-06-17
- PMID 15746509.
- PMID 11219327.
- ^ "Evaluating Newer Sleeping Pills Used to Treat: Insomnia: Comparing Effectiveness, Safety, and Price" (PDF). Consumer Reports. January 2012. p. 14. Retrieved 4 June 2013.
- PMID 23248080.
- S2CID 141232890.
- PMID 16750462.
- PMID 17599165. Archived from the original(PDF) on 2013-05-15. Retrieved 2007-10-07.
- PMID 26711081.
- PMID 17652991.
- PMID 18505619.
- ^ S2CID 250536370.
- PMID 17852167.
- PMID 10682233.
- PMID 17117195. Archived from the originalon 2007-10-28.
- PMID 15954071.
- PMID 15725964.
- PMID 14592194.
- PMID 15266187.
- PMID 2230061.
- PMID 17302.
- PMID 2867122.
- S2CID 45013069.
- PMID 11905433.
- S2CID 33929400.
- S2CID 22856696.
- ^ PMID 17711589.
- S2CID 7946506.
- PMID 29077902.
- S2CID 24222535.
- ^ MedlinePlus (January 8, 2001). "Eszopiclone". National Institutes of Health. Archived from the original on February 27, 2008. Retrieved 21 March 2008.
- ^ Professor Heather Ashton. "Benzodiazepines: How They Work and How to Withdraw".
- PMID 16096519.
- PMID 20171127.
- PMID 16916422.
- PMID 16860264.
- S2CID 40188442.
