Opipramol
This article needs additional citations for verification. (August 2017) |
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Insidon, Pramolan, others |
| Other names | G-33040; RP-8307[1] |
| AHFS/Drugs.com | International Drug Names |
| Routes of administration | Oral |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 94%[3] |
| Protein binding | 91%[3] |
| Metabolism | CYP2D6-mediated[3] |
| Elimination half-life | 6–11 hours[3] |
| Excretion | Urine (70%), feces (10%)[3] |
| Identifiers | |
| |
JSmol) | |
| |
| |
| | |
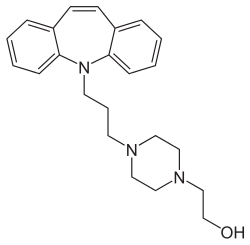
Opipramol, sold under the brand name Insidon among others, is an
Medical uses
Opipramol is typically used in the treatment of
Contraindications
- In patients with hypersensitivityto opipramol or another component of the formulation
- Acute intoxications
- Acute urinary retention
- Acute delirium
- Untreated narrow-angle glaucoma
- Benign prostatic hyperplasia with residual urinary retention
- Paralytic ileus
- Pre-existing higher-grade ventricular stimulusconduction disturbances
- Combination with monoamine oxidase inhibitor (MAOI)
Pregnancy and lactation
Experimental animal studies did not indicate injurious effects of opipramol on the
Side effects
Frequently (≥1% to <10%) reported adverse reactions with opipramol, especially at the beginning of the treatment, include
Adverse reactions reported occasionally (≥0.1% to <1%) include
Rarely (≥0.01% to <0.1%) reported adverse reactions include excitation, headache,
Very rarely (<0.01%) reported adverse reactions include
It could also cause headache.
Overdose
Symptoms of intoxication from
Since no
Interactions
Opipramol can be co-prescribed with other psychiatric drugs, such as antidepressants, anxiolytics and antipsychotics, in which case it can interact with them. Most problematic interactions are generally additive or synergistic, such that, when drugs are combined, their effects intensify, which usually manifests as an increase in side effects, but can also be dangerous, depending on the drugs involved.
While opipramol is not a monoamine reuptake inhibitor, any irreversible MAOIs should still be discontinued at least 14 days before treatment. Opipramol can compete with other TCAs, beta blockers, antiarrhythmics (of class 1c) and other drugs for microsomal enzymes, which can lead to slower metabolism and higher plasma concentrations of these drugs. Co-administration of antipsychotics (e.g., haloperidol, risperidone) can increase the plasma concentration of opipramol. Barbiturates and anticonvulsants, on the other hand, can reduce the plasma concentration of opipramol and thereby weaken its therapeutic effect.[3]
Pharmacology
Pharmacodynamics
| Site | Ki (nM) | Species | Ref |
|---|---|---|---|
| σ1 | 0.2–50 | Rodent | [17][18][19] |
| σ2 | 110 | ND | [20] |
| SERT | ≥2,200 | Rat/? | [21][22][23] |
| NET | ≥700 | Rat/? | [21][22][23] |
| DAT | ≥3,000 | Rat/? | [21][22][23] |
| 5-HT1A | >10,000 | ? | [23] |
| 5-HT2A | 120 | ? | [23] |
| 5-HT2C | ND | ND | ND |
| α1 | 200 | ? | [23] |
| α2 | 6,100 | ? | [23] |
D1 |
900 | Rat | [19] |
D2 |
120–300 | Rat | [23][19] |
| H1 | 6.03 | Human | [24] |
| H2 | 4,470 | Human | [24] |
| H3 | 61,700 | Human | [24] |
| H4 | >100,000 | Human | [24] |
| mACh | 3,300 | ? | [23] |
| NMDA/PCP | >30,000 | Rat | [19] |
| Values are Ki (nM). The smaller the value, the more strongly the drug binds to the site. | |||
Opipramol acts as a high
Unlike other TCAs, opipramol does not
Sigma receptors are a set of
Pharmacokinetics
Opipramol is rapidly and completely
History
Opipramol was developed by
Society and culture
Generic names
Opipramol is the
Brand names
Opipramol is marketed under the brand names Deprenil, Dinsidon, Ensidon, Insidon, Insomin, Inzeton, Nisidana, Opipram, Opramol, Oprimol, Pramolan, and Sympramol among others.[1][4][5]
References
- ^ ISBN 978-1-4757-2085-3.
- ^ Anvisa (2023-03-31). "RDC Nº 784 - Listas de Substâncias Entorpecentes, Psicotrópicas, Precursoras e Outras sob Controle Especial" [Collegiate Board Resolution No. 784 - Lists of Narcotic, Psychotropic, Precursor, and Other Substances under Special Control] (in Brazilian Portuguese). Diário Oficial da União (published 2023-04-04). Archived from the original on 2023-08-03. Retrieved 2023-08-16.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae Mohapatra S, Rath NM, Agrawal A, Verma J (October 2013). "Opipramol: A Novel Drug" (PDF). Delhi Psychiatry Journal. 16 (2): 409–411. Archived from the original (PDF) on 2020-07-11. Retrieved 2014-03-25.
- ^ ISBN 978-3-88763-075-1.
- ^ a b c d "Opipramol".
- ^ S2CID 27014778.
- ^ S2CID 260238755.
- S2CID 40241272.
- PMID 33499332.
- PMID 32151075.
- S2CID 74130809.
- S2CID 39368370.
- ^ PMID 28320023.
- PMID 26417811. Retrieved 2 April 2022.
- S2CID 260242120.
- ^ Roth BL, Driscol J. "PDSP Ki Database". Psychoactive Drug Screening Program (PDSP). University of North Carolina at Chapel Hill and the United States National Institute of Mental Health. Retrieved 14 August 2017.
- ^ PMID 8755605.
- PMID 2477524.
- ^ S2CID 23110359.
- PMID 2568580.
- ^ S2CID 36424574.
- ^ ISBN 978-0-89603-121-0.
- ^ S2CID 5832198.
- ^ S2CID 14274150.
- ISBN 978-1-118-18552-0.
- S2CID 24448788.
- ^ PMID 19557250.
- ISBN 978-94-011-4439-1.


