Oral and maxillofacial pathology
| Oral and maxillofacial pathology | |
|---|---|
| Other names | Oral pathology, stomatognathic disease, dental disease, mouth disease |
| Specialty | Dentistry |
Oral and maxillofacial pathology refers to the diseases of the mouth ("oral cavity" or "stoma"), jaws ("maxillae" or "gnath") and related structures such as salivary glands, temporomandibular joints, facial muscles and perioral skin (the skin around the mouth).[1][2] The mouth is an important organ with many different functions. It is also prone to a variety of medical and dental disorders.[3]
The specialty oral and maxillofacial pathology is concerned with diagnosis and study of the causes and effects of diseases affecting the oral and maxillofacial region. It is sometimes considered to be a specialty of
Diagnosis
The key to any diagnosis is thorough medical, dental, social and psychological history as well as assessing certain lifestyle risk factors that may be involved in disease processes. This is followed by a thorough clinical investigation including extra-oral and intra-oral hard and soft tissues.[5]
It is sometimes the case that a diagnosis and treatment regime are possible to determine from history and examination, however it is good practice to compile a list of differential diagnoses. Differential diagnosis allows for decisions on what further investigations are needed in each case.[5]
There are many types of investigations in diagnosis of oral and maxillofacial diseases, including screening tests, imaging (radiographs, CBCT, CT, MRI, ultrasound) and histopathology (biopsy).[5]
Biopsy
A biopsy is indicated when the patient's clinical presentation, past history or imaging studies do not allow a definitive diagnosis. A biopsy is a surgical procedure that involves the removal of a piece of tissue sample from the living organism for the purpose of microscopic examination. In most cases, biopsies are carried out under local anaesthesia. Some biopsies are carried out endoscopically, others under image guidance, for instance ultrasound, computed tomography (CT) or magnetic resonance imaging (MRI) in the radiology suite. Examples of the most common tissues examined by means of a biopsy include oral and sinus mucosa, bone, soft tissue, skin and lymph nodes.[6]
Types of biopsies typically used for diagnosing oral and maxillofacial pathology are:
Excisional biopsy: A small lesion is totally excised. This method is preferred if the lesions are approximately 1 cm or less in diameter, clinically and seemingly benign and surgically accessible. Large lesions which are more diffused and dispersed in nature or those which are seemed to be more clinically malignant are not conducive to total removal.[7]
Incisional biopsy: A small portion of the tissue is removed from an abnormal-looking area for examination. This method is useful in dealing with large lesions. If the abnormal region is easily accessed, the sample may be taken at the doctor's office. If the tumour is deeper inside the mouth or throat, the biopsy may need to be performed in an operating room. General anaesthesia is administered to eliminate any pain.[7]
Exfoliative cytology: A suspected area is gently scraped to collect a sample of cells for examination. These cells are placed on a glass slide and stained with dye, so that they can be viewed under a microscope. If any cells appear abnormal, a deeper biopsy will be performed.[7]
Diseases
Oral and maxillofacial pathology can involve many different types of tissues of the head. Different disease processes affect different tissues within this region with various outcomes. A great many diseases involve the mouth, jaws and orofacial skin. The following list is a general outline of pathologies that can affect oral and maxillofacial region; some are more common than others. This list is by no means exhaustive.
Congenital
Cleft lip and palate
People with cleft lip and palate malformation tend to be less social and report lower self-esteem, anxiety and depression related to their facial malformation.[12][13] One of the major goals in the treatment of patients with cleft is to enhance social acceptance by surgical reconstruction.
A cleft lip is an opening of the upper lip, mainly due to the failure of fusion of the medial nasal processes with the palatal processes; a cleft palate is the opening of the soft and hard palate in the mouth, which is due to the failure of the palatal shelves to fuse together.[10]
The palate's main function is to demarcate the nasal and oral cavity, without which the patient will have problems with swallowing, eating and speech, thus affecting the quality of life and in some cases certain functions.[10]
Some examples include food going up into the nasal cavity during swallowing as the soft palate is not present to close the cavity during the process. Speech is also affected as the nasal cavity is a source of resonance during speech and failure to manipulate spaces in the cavities will result in the lack of ability to produce certain consonants in audible language.[10]
Macroglossia
Macroglossia is a rare condition, categorised by tongue enlargement which will eventually create a crenated border in relation to the embrasures between the teeth.[14]
Hereditary causes include vascular malformations, Down syndrome, Beckwith–Wiedemann syndrome, Duchenne muscular dystrophy, and Neurofibromatosis type I.[14]
Acquired causes include
Consequences may include noisy breaths – airway obstruction in severe cases, drooling, difficulty eating, lisping speech, open bite, and protruding tongue, which may ulcerate and undergo necrosis.[14]
For mild cases, surgical treatment is not mandatory but if speech is affected, speech therapy may be useful. Reduction glossectomy may be required for severe cases.[14]
Ankyloglossia
Stafne defect
Torus palatinus
Torus palatinus is a bony protrusion on the palate, usually present on the midline of the hard palate.[citation needed]
Torus mandibularis
Torus mandibularis is a bony growth in the mandible along the surface nearest to the tongue. Mandibular tori usually are present near the premolars and above the location on the mandible of the mylohyoid muscle attachment.[17]
Eagle syndrome
Eagle syndrome is a condition where there is an abnormal ossification of the stylohyoid ligament. This leads to an increase in the thickness and the length of the stylohyoid process and the ligament. Pain is felt due to the pressure applied to the internal jugular vein. Eagle syndrome occurs due to elongation of the styloid process or calcification of the stylohyoid ligament. However, the cause of the elongation has not been known clearly. It could occur spontaneously or could arise since birth. Usually normal stylohyoid process is 2.5–3 cm in length, if the length is longer than 3 cm, it is classified as an elongated stylohyoid process.[18]
Acquired
Infective

Bacterial
- (tartar that brushing does not clean. Smoking is a major risk factor.[19] Treatment of gingivitis is dependent on how severe and how far the disease has progressed. If the disease is not too severe it is possible to treat it with chlorhexidine rinse and brushing with fluoride toothpaste to kill the bacteria and remove the plaque, but once the infection has progressed antibiotics may be needed to kill the bacteria.[20]
- Periodontitis—When gingivitis is not treated it can advance to periodontitis, when the gums pull away from the teeth and form pockets that harbor the bacteria. Bacterial toxins and the body's natural defenses start to break down the bone and connective tissues. The tooth may eventually become loose and have to be removed.
- tonsilitis and pharyngitis before involving the soft palate and the tongue. It usually occurs in children where a fever occurs and an erythematous rash develops on the face and spreads to most part of the body. If not treated, late stages of this condition may include a furred, raw, red tongue.[21] Treatment options include penicillin and the prognosis is generally excellent.[4]
Viral
- herpes labialis). HSV infections tend to recur periodically. Although many people get infected with the virus, only 10% actually develop the sores. The sores may last anywhere from 3–10 days and are very infectious. Some people have recurrences either in the same location or at a nearby site. Unless the individual has an impaired immune system, e.g., owing to HIV or cancer-related immune suppression,[22] recurrent infections tend to be mild in nature and may be brought on by stress, sun, menstrual periods, trauma or physical stress.[23]
- inflammation of the brain, pancreatitis, testicular swelling or hearing loss.[24]
Fungal

Traumatic
- Chemical, thermal, mechanical or electrical trauma to the oral soft tissues can cause traumatic oral ulceration.
Autoimmune
This article may benefit from being shortened by the use of summary style. |
- Erythema and lobulation of the tongue
- Oral discomfort
- Difficulty in swallowing and talking
- Altered taste
- Poor retention of dentures (if worn)
- Oral fungal and bacterial infections
- Salivary glands swelling
- Dryness of skin; nose; throat; vagina
- Peripheral neuropathies
- Pulmonary; thyroid; and renal disorders;
- Arthralgias and myalgias;
Tests used to diagnose Sjögren syndrome include:
- tear break-up time and Schirmer's tests
- a minor salivary gland biopsy taken from the lip
- blood tests
- salivary flow rate
There is no cure for Sjögren syndrome; however, there are treatments used to help with the associated symptoms.
- Eye care: artificial tears, moisture chamber spectacles, punctal plugs, pilocarpine medication
- Mouth care: increase oral intake, practice good oral hygiene, use sugar free gum (to increase saliva flow), regular use of mouth rinses, pilocarpine medication, reduce alcohol intake and smoking cessation. Saliva substitutes are also available as a spray, gel, gum or in the form of a medicated sweet
- Dry skin: creams, moisturising soaps
- Vaginal dryness: lubricant, oestrogen creams, hormonal replacement therapy
- Muscle and joint pains: Non-steroidal anti-inflammatory drugs
Complications of Sjögren syndrome include ulcers that can develop on the surface of the eyes if the dryness is not treated. These ulcers can then cause more worrying issues such as loss of eyesight and life-long damage. Individuals with Sjögren syndrome have a slightly increased risk of developing non-Hodgkin lymphoma, a type of cancer. Other conditions such as peripheral neuropathy, Raynaud's phenomenon, kidney problems, underactive thyroid gland and irritable bowel syndrome have been linked to Sjögren syndrome.[28]
Inflammatory
Neoplastic
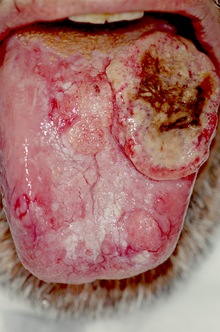
- human papillomavirus, and hematopoietic stem cell transplantation.[29]The earlier the oral cancer is diagnosed, the better the chances for full recovery. Persistent suspicious masses or ulcers on the mouth should always be examined. Diagnosis is usually made with a biopsy; treatment depends on the exact type of cancer, where it is situated, and extent of spreading.
Environmental
Unknown
There are many oral and maxillofacial pathologies which are not fully understood.
- Burning mouth syndrome (BMS) is a disorder where there is a burning sensation in the mouth that has no identifiable medical or dental cause. The disorder can affect anyone but tends to occur most often in middle-aged women. BMS has been hypothesized to be linked to a variety of factors such as the menopause, dry mouth (xerostomia) and allergies. BMS usually lasts for several years before disappearing for unknown reasons. Other features of this disorder include anxiety, depression and social isolation. There is no cure for this disorder and treatment includes use of hydrating agents, pain medications, vitamin supplements or the usage of antidepressants.[30]

- Aphthous stomatitis is a condition where ulcers (canker sores) appear on the inside of the mouth, lips and on tongue. Most small canker sores disappear within 10–14 days. Canker sores are most common in young and middle aged individuals. Sometimes individuals with allergies are more prone to these sores. Besides an awkward sensation, these sores can also cause pain or tingling or a burning sensation. Unlike herpes sores, canker sores are always found inside the mouth and are usually less painful.[citation needed] Good oral hygiene helps but topical corticosteroids may be necessary.[31]

- floor of the mouth.[32]
Specialty
| Occupation | |
|---|---|
| Names | Oral and Maxillofacial Pathologist, Oral Pathologist |
Occupation type | Specialty |
Activity sectors | Pathology, Dentistry, Medicine |
| Specialty | gastroenterology |
| Description | |
Education required | Varies. Typically dental degree followed by specialist training |
Oral and maxillofacial pathology, previously termed oral pathology, is a speciality involved with the diagnosis and study of the causes and effects of diseases affecting the oral and maxillofacial regions (i.e. the mouth, the jaws and the face). It can be considered a speciality of dentistry and pathology.[4] Oral pathology is a closely allied speciality with oral and maxillofacial surgery and oral medicine.
The clinical evaluation and diagnosis of oral mucosal diseases are in the scope of oral and maxillofacial pathology specialists and oral medicine practitioners,[33] both disciplines of dentistry.
When a
In some parts of the world, oral and maxillofacial pathologists take on responsibilities in
Geographic variation
United Kingdom
There are approximately 30 consultant oral and maxillofacial pathologists in the UK. A dental degree is mandatory, but a medical degree is not. The shortest pathway to becoming an oral pathologist in the UK is completion of two years' general professional training and then five years in a diagnostic histopathology training course. After passing the required
New Zealand
There are five practising oral pathologists in New Zealand (as of May 2013[update]).[36] Oral pathologists in New Zealand also take part in forensic evaluations.[36]
See also
References
- ^ "gnath(o)-". TheFreeDictionary.com.
- ^ "ICD-10".
- ^ Mouth Disease Information Archived 2010-02-06 at the Wayback Machine Retrieved on 2010-02-01
- ^ ISBN 978-0721690032.
- ^ )
- )
- ^ )
- PMID 24607185.
- PMID 24607185.
- ^ )
- ^ Young G. Cleft Lip and Palate. Available at http://www2.utmb.edu/otoref/Grnds/Cleft-lip-palate-9801.htm[permanent dead link].
- S2CID 7017113.
- PMID 15947228.
- ^ )
- PMID 12501105.
- PMID 5251442.
- ISBN 9780721690032.
- PMID 19881063.
- ^ "Periodontal (Gum) Disease: Causes, Symptoms, and Treatments". National Institute of Dental and Craniofacial Research. Retrieved 2013-12-27.
- ^ "Gingivitis". Emedicine. Retrieved 2013-12-25.
- ^ OCLC 61756542.
- S2CID 2969472.
- ^ Herpes Guide: How do I know if I have herpes Canadian Herpes Information portal. Retrieved on 2010-02-01
- ^ What are Mumps Archived 2010-02-05 at the Wayback Machine Ministry of health and long term care portal. Retrieved on 2010-02-01
- ^ "Women's Oral Health and Overall". Archived from the original on 2009-12-03. Retrieved 2010-02-02.
- S2CID 23211726.
- PMID 25114590.
- S2CID 11132886.
- PMID 21119507.
- ^ Burning Mouth Syndrome Archived 2010-12-03 at the Wayback Machine American Academy of Family Physicians. Retrieved on 2010-02-01
- ^ Diseases of the Digestive System The oral cavity FAQ's Health Portal. Retrieved on 2010-02-01
- PMID 21763590.
- PMID 21883487.
- ^ "ADA.org: Dentistry Definitions". Archived from the original on 2009-02-28. Retrieved 2010-02-02.
- ^ "The British Society of Oral & Maxillofacial Pathologists". Archived from the original on 10 December 2013. Retrieved 25 April 2013.
- ^ a b "Specialisation". New Zealand Dental Association. Archived from the original on 5 March 2016. Retrieved 10 September 2013.
Further reading
- Fechner RE (2002). "A Brief History of Head and Neck Pathology". Modern Pathology. 15 (3): 221–228. PMID 11904339.
