Otilimab
This article may have been created or edited in return for undisclosed payments, a violation of Wikipedia's terms of use. It may require cleanup to comply with Wikipedia's content policies, particularly neutral point of view. (November 2019) |
| Monoclonal antibody | |
|---|---|
| Type | ? |
| Clinical data | |
| Other names | GSK3196165; MOR103 |
| Legal status | |
| Legal status |
|
| Identifiers | |
| CAS Number | |
| UNII | |
| KEGG | |
Otilimab (development codes MOR103 and GSK3196165) is a fully human antibody which has been developed by the biotechnology company MorphoSys.[1] It can also be referred to as HuCAL antibody, HuCAL standing for Human Combinatorial Antibody Library and being a technology used to generate monoclonal antibodies. Otilimab is directed against the granulocyte-macrophage colony stimulating factor (GM-CSF), a monomeric glycoprotein functioning as a cytokine promoting both proliferation and activation of macrophages and neutrophils.
Mode of action
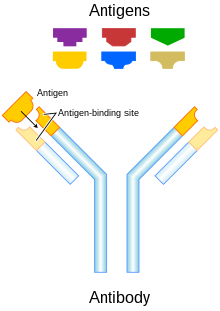
Otilimab, as its monoclonal antibody, specifically binds to GM-CSF which is consequently neutralised and incapable of binding its targeted inflammatory cells as it should in order to allow their proliferation and activation. There is no following induction of inflammation (through cytokines e.g. TNF-α, IL-1, IL-6), chemotaxis (via chemokines e.g. IL-8), tissue degradation (caused by e.g. MMPs, H2O2) or T and B cell response (following up-regulated MHC II level).
Medical uses
Beyond its role in natural immune pathways, GM-CSF has been shown to be involved in autoimmune diseases such as multiple sclerosis (MS) and rheumatoid arthritis (RA) in which cases GM-CSF levels are elevated and mediate an increased production of pro-inflammatory elements (cytokines, chemokines, proteases). The factor is also known to be involved in osteoarthritis of the hand. Research has thus been working on it as a molecular target for the treatment of such disorders, notably through immunotherapy such as monoclonal antibody therapy which is known to be efficient against autoimmune diseases.
Rheumatoid arthritis
There already exist treatments of rheumatoid arthritis through monoclonal antibodies (i.e.
Multiple sclerosis
In multiple sclerosis (MS), GM-CSF is produced by
There are numerous existing monoclonal antibodies used in the treatment of multiple sclerosis: natalizumab (targets α4-integrin), daclizumab and alemtuzumab (both binding to CD25, the α-subunit of IL-2 receptor on the surface of mature lymphocytes), ocrelizumab (against CD20 marker on B-cells).[2] However, the frequent adverse effects notified, including secondary autoimmune phenomena,[3] suggest that the uncovering of a new molecular target for monoclonal antibody therapy would be welcomed in the research for an improved treatment against MS.
Otilimab is currently undergoing
References
- ^ "Official web page of MOR103/GSK3196165 on the MorphoSys website". MorphoSys AG. 2014-10-27. Retrieved 2018-06-23.
- S2CID 19160653.
- S2CID 34738692.
- PMID 26185773.
