Pancreas
| Pancreas | |
|---|---|
Splenic lymph nodes, celiac lymph nodes and superior mesenteric lymph nodes | |
| Identifiers | |
| Latin | pancreas |
| Greek | Πάνκρεας (Pánkreas) |
| MeSH | D010179 |
| TA98 | A05.9.01.001 |
| TA2 | 3114 |
| FMA | 7198 |
| Anatomical terminology] | |
The pancreas is an
Inflammation of the pancreas is known as
The word pancreas comes from the Greek πᾶν (pân, "all") & κρέας (kréas, "flesh"). The function of the pancreas in diabetes has been known since at least 1889, with its role in insulin production identified in 1921.
Structure
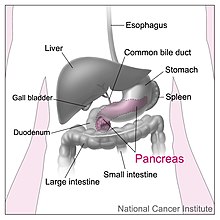
The pancreas is an organ that in humans lies in the abdomen, stretching from behind the stomach to the left upper abdomen near the spleen. In adults, it is about 12–15 centimetres (4.7–5.9 in) long, lobulated, and salmon-coloured in appearance.[7]
Anatomically, the pancreas is divided into a head, neck, body, and tail. The pancreas stretches from the inner curvature of the duodenum, where the head surrounds two blood vessels: the superior mesenteric artery and vein. The longest part of the pancreas, the body, stretches across behind the stomach, and the tail of the pancreas ends adjacent to the spleen.[7]
Two ducts, the
Parts
The head of the pancreas sits within the curvature of the duodenum, and wraps around the superior mesenteric artery and vein. To the right sits the descending part of the duodenum, and between these travel the superior and inferior pancreaticoduodenal arteries. Behind rests the inferior vena cava, and the common bile duct. In front sits the peritoneal membrane and the transverse colon.[7] A small uncinate process emerges from below the head, situated behind the superior mesenteric vein and sometimes artery.[7]
The neck of the pancreas separates the head of the pancreas, located in the curvature of the duodenum, from the body. The neck is about 2 cm (0.79 in) wide, and sits in front of where the
The body is the largest part of the pancreas, and mostly lies behind the stomach, tapering along its length. The peritoneum sits on top of the body of the pancreas, and the
The pancreas narrows towards the tail, which sits near to the spleen.
Blood supply
The pancreas has a rich blood supply, with vessels originating as branches of both the
The body and neck of the pancreas drain into the
The pancreas drains into lymphatic vessels that travel alongside its
Microanatomy
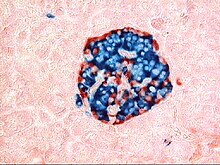
The pancreas contains tissue with an
The majority of pancreatic tissue has a digestive role. The cells with this role form clusters (
The tissues with an
Variation
The size of the pancreas varies considerably.
Gene and protein expression
10,000 protein coding genes (~50% of all human genes) are expressed in the normal human pancreas.[14][15] Less than 100 of these genes are specifically expressed in the pancreas. Similar to the salivary glands, most pancreas-specific genes encode for secreted proteins. Corresponding pancreas-specific proteins are either expressed in the exocrine cellular compartment and have functions related to digestion or food uptake such as digestive chymotrypsinogen enzymes and pancreatic lipase PNLIP, or are expressed in the various cells of the endocrine pancreatic islets and have functions related to secreted hormones such as insulin, glucagon, somatostatin and pancreatic polypeptide.[16]
Development
The pancreas forms during development from two buds that arise from the duodenal part of the foregut, an embryonic tube that is a precursor to the gastrointestinal tract.[11] It is of endodermal origin.[11] Pancreatic development begins with the formation of a dorsal and ventral pancreatic bud. Each joins with the foregut through a duct. The dorsal pancreatic bud forms the neck, body, and tail of the developed pancreas, and the ventral pancreatic bud forms the head and uncinate process.[11]
The definitive pancreas results from rotation of the ventral bud and the fusion of the two buds.
Cellular development
The cells of the exocrine pancreas differentiate through molecules that induce differentiation including
Pancreatic progenitor cells differentiate into endocrine islet cells under the influence of
Function
The pancreas is involved in
Blood glucose regulation

Cells within the pancreas help to maintain blood glucose levels (homeostasis). The cells that do this are located within the pancreatic islets that are present throughout the pancreas. When blood glucose levels are low, alpha cells secrete glucagon, which increases blood glucose levels. When blood glucose levels are high beta cells secrete insulin to decrease glucose in blood. Delta cells in the islet also secrete somatostatin which decreases the release of insulin and glucagon.[9]
Glucagon acts to increase glucose levels by promoting the
The main factor influencing the secretion of insulin and glucagon are the levels of glucose in blood plasma.
Digestion
The pancreas plays a vital role in the
The cells in each acinus are filled with granules containing the digestive enzymes. These are secreted in an inactive form termed
- Enzymes that break down proteins begin with activation of trypsinogen to trypsin. The free trypsin then cleaves the rest of the trypsinogen, as well as chymotrypsinogen to its active form chymotrypsin.[21]
- Enzymes secreted involved in the digestion of fats include
- Enzymes that break down starch and other carbohydrates include amylase.[21]
These enzymes are secreted in a fluid rich in
A variety of mechanisms act to ensure that the digestive action of the pancreas does not act to digest pancreatic tissue itself. These include the secretion of inactive enzymes (zymogens), the secretion of the protective enzyme trypsin inhibitor, which inactivates trypsin, the changes in pH that occur with bicarbonate secretion that stimulate digestion only when the pancreas is stimulated, and the fact that the low calcium within cells causes inactivation of trypsin.[21]
Additional functions
The pancreas also secretes vasoactive intestinal peptide and pancreatic polypeptide. Enterochromaffin cells of the pancreas secrete the hormones motilin, serotonin, and substance P.[9]
Clinical significance
Inflammation
Inflammation of the pancreas is known as
In pancreatitis, enzymes of the exocrine pancreas damage the structure and tissue of the pancreas. Detection of some of these enzymes, such as amylase and lipase in the blood, along with symptoms and findings on medical imaging such as ultrasound or a CT scan, are often used to indicate that a person has pancreatitis. Pancreatitis is often managed medically with pain reliefs, and monitoring to prevent or manage shock, and management of any identified underlying causes. This may include removal of gallstones, lowering of blood triglyceride or glucose levels, the use of corticosteroids for autoimmune pancreatitis, and the cessation of any medication triggers.[25]
Cancer

Pancreatic adenocarcinoma is the most common form of pancreatic cancer, and is cancer arising from the exocrine digestive part of the pancreas. Most occur in the head of the pancreas.
Because of the late development of symptoms, most cancer presents at an advanced
There are several types of pancreatic cancer, involving both the endocrine and exocrine tissue. The many types of
A solid pseudopapillary tumour is a low-grade malignant tumour of the pancreas of papillary architecture that typically afflicts young women.[35]
Diabetes mellitus
Type 1 diabetes
Type 2 diabetes
Diabetes mellitus type 2 is the most common form of diabetes.[36] The causes for high blood sugar in this form of diabetes usually are a combination of insulin resistance and impaired insulin secretion, with both genetic and environmental factors playing a role in the development of the disease.[38] Over time, pancreatic beta cells may become "exhausted" and less functional.[36] The management of type 2 diabetes involves a combination of lifestyle measures, medications if required and potentially insulin.[39] With relevance to the pancreas, several medications act to enhance the secretion of insulin from beta cells, particularly
Removal
It is possible for a person to live without a pancreas, provided that the person takes insulin for proper regulation of blood glucose concentration and pancreatic enzyme supplements to aid digestion.[40]
History
The pancreas was first identified by
The way the tissue of the pancreas has been viewed has also changed. Previously, it was viewed using simple staining methods such as H&E stains. Now, immunohistochemistry can be used to more easily differentiate cell types. This involves visible antibodies to the products of certain cell types, and helps identify with greater ease cell types such as alpha and beta cells.[9]
Other animals
Pancreatic tissue is present in all
In teleost fish, and a few other species (such as rabbits), there is no discrete pancreas at all, with pancreatic tissue being distributed diffusely across the mesentery and even within other nearby organs, such as the liver or spleen. In a few teleost species, the endocrine tissue has fused to form a distinct gland within the abdominal cavity, but otherwise it is distributed among the exocrine components. The most primitive arrangement, however, appears to be that of lampreys and lungfish, in which pancreatic tissue is found as a number of discrete nodules within the wall of the gut itself, with the exocrine portions being little different from other glandular structures of the intestine.[46]
Cuisine
The pancreas of calf (ris de veau) or lamb (ris d'agneau), and, less commonly, of beef or pork, are used as food under the culinary name of sweetbread.[47][48]
Additional images
-
A normal pancreas on ultrasound.
-
Identifying pancreas on abdominal ultrasonography when it is partly obscured by bowel gas.
-
Pancreas of a human embryo at end of sixth week
-
The pancreas and its surrounding structures
-
Duodenum and pancreas. Deep dissection.
References
- ^ Nosek, Thomas M. "Section 6/6ch2/s6ch2_30". Essentials of Human Physiology. Archived from the original on 2016-03-24.
- PMID 2865807.
- ^ "Pancreas Gland - Endocrine System". Innerbody. Retrieved 2021-06-12.
- ^ Beger's 2018, pp. 124.
- ^ "Endocrine Pancreas - an overview ScienceDirect Topics". www.sciencedirect.com. Retrieved 2021-06-12.
- PMID 6111521.
- ^ a b c d e f g h i j k l m n o p q r Gray's 2016, pp. 1179–1189.
- ^ a b Gray's 2008, pp. 1183–1190.
- ^ a b c d e f g h i Wheater's Histology 2013, pp. 332–333.
- ^ a b c Wheater's Histology 2013, pp. 287–291.
- ^ ISBN 9781496383907.
- ^ Kanth, Rajan; Roy, Praveen K; Al Samman, Mounzer; Patti, Marco G (2019-11-21). "Pancreatic Divisum: Pathophysiology". emedicine.medscape.com. Medscape.
- PMID 26388905.
- ^ "The human proteome in pancreas – The Human Protein Atlas". www.proteinatlas.org. Retrieved 2017-09-25.
- S2CID 802377.
- PMID 25546435.
- ^ ISBN 978-0323523752.
- ^ a b Harrison's 2015, pp. 2853–4.
- ^ OCLC 1076268769.)
{{cite book}}: CS1 maint: location missing publisher (link - ISBN 978-1-4557-7016-8.
- ^ a b c d e f g h Harrison's 2015, pp. 2086–2102.
- ^ Harrison's 2015, pp. 2090.
- ^ Beger's 2018, pp. 16, 57.
- from the original on Nov 18, 2022.
- ^ a b c d e f g h i j k Davidson's 2018, p. 837-844.
- PMID 21721197.
Diagram by Mikael Häggström, M.D. - ^ PMID 25207767.
- ^ "Pancreatic Cancer Treatment (PDQ®) Patient Version". National Cancer Institute. 2014-04-17. Retrieved 8 June 2014.
- PMID 23856911.
- PMID 18695761.
- ^ ISBN 978-9283204299.
- ^ "American Cancer Society: Cancer Facts & Figures 2010: see page 4 for incidence estimates, and page 19 for survival percentages" (PDF). Archived from the original (PDF) on 2015-01-14.
- ^ "Pancreatic Cancer Treatment (PDQ®) Health Professional Version". NCI. 2014-02-21. Retrieved 8 June 2014.
- S2CID 7329783.
- PMID 18333264.
- ^ OCLC 1076268769.
- ^ Davidson's 2018, p. 735.
- ^ Davidson's 2018, p. 730-732.
- ^ a b Davidson's 2018, p. 745-751.
- PMID 20567557.
- ISBN 978-1461505556.
- ISBN 978-8129118097.
- ^ Harper, Douglas. "Pancreas". Online Etymology Dictionary. Retrieved 2007-04-04.
- ISBN 978-0742547803.
- ^ PMID 26788261.
- ^ ISBN 978-0039102845.
- Oxford Companion to Food; Oxford English Dictionary
- ISBN 0747560463.
Bibliography
- Barrett, Kim E. (2019). Ganong's review of medical physiology. Barman, Susan M.,, Brooks, Heddwen L., Yuan, Jason X.-J. (26th ed.). New York. OCLC 1076268769.)
{{cite book}}: CS1 maint: location missing publisher (link - Beger HG, ed. (2018). The pancreas : an integrated textbook of basic science, medicine, and surgery (third ed.). Hoboken, NJ. OCLC 1065547789.)
{{cite book}}: CS1 maint: location missing publisher (link - Kasper D, Fauci A, Hauser S, Longo D, Jameson J, Loscalzo J (2015). Harrison's Principles of Internal Medicine (19 ed.). McGraw-Hill Professional. ISBN 9780071802154.
- Ralston SH, Penman ID, Strachan MW, Hobson RP, eds. (2018). Davidson's principles and practice of medicine (23rd ed.). Elsevier. ISBN 978-0-7020-7028-0.
- Standring, Susan; Borley, Neil R.; et al., eds. (2008). Gray's anatomy : the anatomical basis of clinical practice (40th ed.). London: Churchill Livingstone. ISBN 978-0-8089-2371-8.
- Standring, Susan, ed. (2016). Gray's anatomy : the anatomical basis of clinical practice (41st ed.). Philadelphia. )
- Young, Barbara; O'Dowd, Geraldine; Woodford, Phillip (2013). Wheater's functional histology: a text and colour atlas (6th ed.). Philadelphia: Elsevier. ISBN 9780702047473.
External links
 Media related to Pancreas at Wikimedia Commons
Media related to Pancreas at Wikimedia Commons- Pancreas at the Human Protein Atlas
- Pancreatic Diseases – English – The Gastro Specialist





