Parasitic worm

Parasitic worms, also known as helminths,
Some parasitic worms, including
Parasitic worms live in and feed in living
Many of the worms referred to as helminths are intestinal parasites. An infection by a helminth is known as helminthiasis, helminth infection, or intestinal worm infection. There is a naming convention which applies to all helminths: the ending "-asis" (or in veterinary science: "-osis") is added at the end of the name of the worm to denote the infection with that particular worm.[citation needed] For example, Ascaris is the name of a type of helminth, and ascariasis is the name of the infection caused by that helminth.
Taxonomy


Helminths are a group of organisms which share a similar form but are not necessarily
There may be as many as 300,000 species of parasites affecting vertebrates,[9] and as many as 300 affecting humans alone.[10]
Helminths of importance in the
Reproduction and life cycle
The lifetime of adult worms varies tremendously from one species to another but is generally in the range of 1 to 8 years (see following table). This lifetime of several years is a result of their ability to manipulate the immune response of their hosts by secreting immunomodulatory products.[4]
Helminths can be either hermaphroditic (having the sex organs of both sexes), like tapeworms and flukes (not including the blood fluke), or have their sexes differentiated, like the roundworms.[13] All helminths produce eggs (also called ova) for reproduction.[14]
Eggs
Generally, thousands or even hundreds of thousands of eggs are produced each time the female worm deposits its eggs - a process called
Helminth eggs are resistant to various environmental conditions due to the composition of the egg shell. Each helminth egg species has 3 to 4 layers with different physical and chemical characteristics:
Larvae
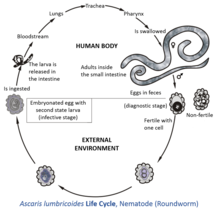
Larvae hatch from eggs, either inside or outside the host, depending on the type of helminth. For eggs in moist soil at optimal temperature and oxygen levels, the embryo develops into an infective larva after 2 to 4 weeks, named "second-stage larva". Once ingested by a host, this larva has the ability to get out of the egg, hatch in the small intestine and migrate to different organs. These infective larvae (or "infective eggs") may remain viable in soil for two years or longer.[22]
The process of larval maturation in the host can take from about two weeks up to four months, depending on the helminth species.[citation needed]
The following table shows the principal morphological and reproductive distinctions for three helminth groups:
| Tapeworms (Cestodes) |
Flukes (Trematodes) |
Roundworms (Nematodes) | ||||||
|---|---|---|---|---|---|---|---|---|
| Examples | Taenia solium, Taenia saginata, Hymenolepis spp., Echinococcus granulosus, Echinococcus multilocularis, Multiceps multiceps | Schistosoma mansoni, Schistosoma japonicum, | Ascaris spp., Enterobius, Filarioidea, Onchocerca spp., Rhabditis spp., Trichuris spp., Necator americanus, Ancylostoma spp. | |||||
| Pathological conditions caused in humans | Tapeworm infection, echinococcosis, alveolar echinococcosis
|
Schistosomiasis, swimmer's itch | enterobiasis (pinworm), filariasis, hookworm infection (includes Necatoriasis and Ancylostoma duodenale infection), onchocerciasis, trichinosis, trichuriasis (whipworm)
| |||||
| Shape | Segmented plane | Unsegmented plane | Cylindrical | |||||
| Body cavity | None | None | Present | |||||
| Body covering | Tegument |
Tegument | Cuticle | |||||
| Digestive tube | None | Ends in cecum | Ends in anus | |||||
| Sex | Hermaphroditic |
dioecious |
Dioecious
| |||||
| Attachment organs | bothridia, and rostellum with hooks |
Oral sucker and ventral sucker or acetabulum | Lips, teeth, filariform extremities, and dentary plates | |||||
|
Number of species |
6000[23] | Estimated > 15,000[24] Registered > 9,000[25] | Estimated > 800,000 to 1,000,000
Registered > 25,000[24] | |||||
| Number of species known to infect humans | 40[23] | 16[24] | > 12,000[24] | |||||
| Species |
Hookworm |
Toxocara spp.
| ||||||
| Timeline of lifecycle stages | Larval formation |
Some days (eggs can survive for months)[26] |
9–15 days[23] |
18 days to several weeks[27] |
1–2 days[28] |
15–30 days[29] |
||
| Larval growth |
After hatching, the larvae develop into cysticercoid, which can survive for years in an animal[26] |
5–7 weeks as |
10–14 days[27] |
5–10 days (after maturing can survive for weeks outside the host)[28] |
60–70 days (from hatching to mature state)[29] |
5–6 days[23] | ||
| Maturation to adult |
2 months (from cysticercoid to adult)[26] |
3–4 months[15] |
2–3 months[27] |
2–8 weeks[23] (can become dormant for months) |
||||
| Lifespan of adult worm |
4–6 weeks |
Several years[26] |
8–10 years[23] |
1–2 years[27] |
Several years[28] |
1 year[29] |
||
| Eggs laid per day | 250,000[3] to 700,000[23] | 3,000 to 25,000[24] | 3,000[3] to 250,000[23] | |||||
| Egg deposition | Frequency |
up to 6 times a day[26] |
daily[27] |
daily[28] |
daily[29] |
|||
| Number of eggs per event |
50,000-100,000[26] |
5,000-10,000[23] |
3,000-20,000[29] |
|||||
| Larvae per egg | 1 | 1 | 300 | 1 | 1 | 1 | 1 | |
Draft genomes for all categories of helminth have been sequenced in recent years and are available through the ParaSite sub-portal of WormBase.[30]
Use in medicine
Parasitic worms have been used as a medical treatment for various diseases, particularly those involving an overactive immune response.[31] As humans have evolved with parasitic worms, proponents argue they are needed for a healthy immune system.[31] Scientists are looking for a connection between the prevention and control of parasitic worms and the increase in allergies such as hay-fever in developed countries.[31] Removal of parasitic worms from areas is correlated with an increase in autoimmune disorders in those areas.[32] Parasitic worms may be able to damp down the immune system of their host, making it easier for them to live in the intestine without coming under attack.[31] This may be one mechanism for their proposed medicinal effect.[citation needed]
One study suggests a link between the rising rates of metabolic syndrome in the developed worlds and the largely successful efforts of Westerners to eliminate intestinal parasites. The work suggests eosinophils (a type of white blood cell) in fat tissue play an important role in preventing insulin resistance by secreting interleukin 4, which in turn switches macrophages into "alternative activation". Alternatively-activated macrophages are important to maintaining glucose homeostasis (i.e., blood sugar regulation). Helminth infection causes an increase in eosinophils. In the study, the authors fed rodents a high-fat diet to induce metabolic syndrome, and then injected them with helminths. Helminth infestation improved the rodents' metabolism.[33] The authors concluded:
Although sparse in blood of persons in developed countries, eosinophils are often elevated in individuals in rural developing countries where intestinal parasitism is prevalent and metabolic syndrome rare. We speculate that eosinophils may have evolved to optimize metabolic homeostasis during chronic infections by ubiquitous intestinal parasites….[33]
Human stool samples
For medical purposes, the exact number of helminth eggs is less important and therefore most
Relevance for sanitation


Helminth eggs can reach the soil when polluted wastewater, sewage sludge or human waste are used as fertilizer. Such soil is often characterized by moist and warm conditions. Therefore, the risk of using contaminated wastewater and sludge in agricultural fields is a real problem, especially in poor countries, where this practice is prevalent.[18][34] Helminth eggs are regarded as the main biological health risk when applying sewage sludge, fecal sludge or fecal matter on agricultural soils.[16] The eggs are the infective stage of the helminths’ life cycle for causing the disease helminthiasis.[citation needed]
Due to this strong shell, helminth eggs or ova remain viable in soil, fresh water and sewage for many months. In feces, fecal sludge and sewage sludge they can even remain viable for several years.[16][17] Helminth eggs of concern in wastewater used for irrigation have a size between 20 and 90 μm and a relative density of 1.06–1.23.[18] It is very difficult to inactivate helminth eggs, unless temperature is increased above 40 °C or moisture is reduced to less than 5%.[18] Eggs that are no longer viable do not produce any larvae. In the case of Ascaris lumbricoides (giant roundworm), which has been considered the most resistant and common helminth type, fertilized eggs deposited in soil are resistant to desiccation but are, at this stage of development, very sensitive to environmental temperatures: The reproduction of a fertilized egg within the eggshell develops at an environmental soil temperature about 25 °C which is lower than the body temperature of the host (i.e., 37 °C for humans).[22] However, development of the larvae in the egg stops at temperatures below 15.5 °C, and eggs cannot survive temperatures much above 38 °C. If the temperature is around 25 °C, the infectiousness occurs after nearly 10 days of incubation.[8][35][36]
Removal versus inactivation
In order to physically remove (but not inactivate) helminth eggs from wastewater, processes that remove particles, such as sedimentation, filtration or
Helminth ova cannot be inactivated with chlorine, UV light or ozone (in the latter case at least not with economical doses because >36 mg/L ozone are needed with 1 hour contact time).[citation needed]
Inactivation of helminth ova can be achieved in sewage sludge treatment where the temperature is increased over 40 °C or moisture is reduced to less than 5%.[18] Best results can be obtained when both of these conditions are combined for an extended period of time.[39] Details about the contact time under these conditions and other related environmental factors are generally not well-defined for every type of helminth egg species.[8] Helminth eggs are considered highly resistant biological structures.[18]
Measurements
Indicator organism

The eggs from
Helminth eggs that are found in wastewater and sludge stem from soil-transmitted helminths (STHs) which include Ascaris lumbricoides (Ascaris), Anclostoma duodenale and Necator americanus (hookworm), and Trichuris trichiura (whipworm).[43] Ascaris and whipworm that are identified in reusable wastewater systems can cause certain diseases and complications if ingested by humans and pigs.[44] Hookworms will plant and hatch their larvae into the soil where they grow until maturity. Once the hookworm eggs are fully developed, they infect organisms by crawling through the organism’s skin.[45]
The presence or absence of viable helminth eggs ("viable" meaning that a larva would be able to hatch from the egg) in a sample of dried fecal matter,
Environmental samples
For the purpose of setting treatment standards and reuse legislation, it is important to be able to determine the amount of helminth eggs in an environmental sample with some accuracy. The detection of viable helminth eggs in samples of wastewater, sludge or fresh feces (as a diagnostic tool for the infection helminthiasis) is not straight forward. In fact, many laboratories in developing countries lack the right equipment or skilled staff required to do so. An important step in the analytical methods is usually the concentration of the eggs in the sample, especially in the case of wastewater samples. A concentration step may not be required in samples of dried feces, e.g. samples collected from urine-diverting dry toilets.[citation needed]
See also
- Helminthology – the study of parasitic worms and their effects on their hosts
References
- ^ a b "CDC - Parasites - About Parasites". www.cdc.gov. 20 April 2018.
- PMID 34880874.
- ^ a b c "CDC Centers for Disease Control and Prevention, about parasites". CDC. Retrieved 28 November 2014.
- ^ ISBN 978-1-60805-985-0.
- ^ "Navigating the Phylogeny Wing, University of Berkeley, USA". Retrieved 19 December 2014.
- ^ "Tree of Life web project". Retrieved 19 December 2014.
- ^ a b "Schistosomiasis Research Group, University of Cambridge, UK". Archived from the original on 13 October 2014. Retrieved 19 December 2014.
- ^ PMID 22794801.)
{{cite journal}}: CS1 maint: multiple names: authors list (link - PMID 18695218.
- PMID 12364371.
- ^ Mayo Clinic Staff. "Ringworm (body) - Symptoms and causes". Mayo Clinic. Retrieved 4 July 2018.
- ^ "Ringworm". American Academy of Dermatology. Retrieved 4 July 2018.
- ^ PMID 36588778.
- PMID 35711670.
- ^ a b c "Centers for Disease Control and Prevention: Parasites - Fascioliasis (Fasciola Infection)". Retrieved 13 January 2015.
- ^ ISBN 978-9241546850.
- ^ a b Feachem, R., Bradley, D., Garelick, H., Mara, D. (1983). Sanitation and Disease: Health Aspects of Excreta and Wastewater Management. John Wiley and Sons, New York, NY.
- ^ PMID 17305174.

- S2CID 222626.
- S2CID 39350893.)
{{cite journal}}: CS1 maint: multiple names: authors list (link - ^ ISBN 978-0-12-415915-0.
- ^ ISBN 9684630514)
- ^ a b c d e f Pumarola, A., Rodríguez-Torres, A., García, R.J.A., Piedrola, A.G. (1987). Medical Microbiology and Parasitology (in Spanish), Ediciones Científicas y Técnicas, S. A., Barcelona, Spain, pp 850 - 880
- ^ "Animal diversity web". Animal Diversity Web. September 2001. Retrieved 17 December 2014.
- ^ a b c d e f "Centers for Disease Control and Prevention". Parasites - Taeniasis (Biology). Retrieved 22 January 2015.
- ^ a b c d e f "Centers for Disease Control and Prevention: Parasites - Ascariasis". Retrieved 13 January 2015.
- ^ a b c d "Centers for Disease Control and Prevention: Parasites - Hookworm". Retrieved 13 January 2015.
- ^ a b c d e "Centers for Disease Control and Prevention: Parasites - Trichuriasis (also known as Whipworm Infection)". Retrieved 13 January 2015.
- ^ "WormBase ParaSite". Retrieved 15 April 2016.
- ^ a b c d "Eat worms - feel better". BBC News. 3 December 2003. Retrieved 13 July 2011.
- S2CID 22950215. Retrieved 25 October 2020.
- ^ PMID 21436399. Archived from the original(PDF) on 2016-04-18. Retrieved 18 April 2011.
- ^ Keraita B., Jiménez B., Drechsel P. (2008). Extent and Implications of Agricultural Reuse of Untreated, partly Treated and Diluted Wastewater in Developing Countries. CAB Reviews: Perspectives in Agriculture, Veterinary Science, Nutrition and Natural Resources, Vol 3, No 58, pp 1-15
- PMID 11695127.
- PMID 15276741.)
{{cite journal}}: CS1 maint: multiple names: authors list (link - ^ Jimenez B., Chavez-Mejia A. (1997). Treatment of Mexico City Wastewater for Irrigation Purposes. Environmental Technology, Vol 18, pp 721-730
- ^ Jiménez B., Maya C., Salgado G. (2001). The Elimination of Helminth Ova, Fecal Coliforms, Salmonella and Protozoan Cysts by Various Physicochemical Processes in Wastewater and Sludge. Water Science and Technology, Vol 43, No 12, pp 179-182 (DOI= 10.2166/wst.2001.0733)

- ^ Schmidt, G.D., Roberts, L.S. (1981). Foundations of Parasitology, second ed. C.V. Mosby Company, 795 pp
- ^ ISSN 1476-1777.
- ^ .
- ^ S2CID 46046758.
- ^ Prevention, CDC-Centers for Disease Control and (2021-01-13). "CDC - Soil-Transmitted Helminths". www.cdc.gov. Retrieved 2021-04-27.
- PMID 21508556.
- ^ PMID 17881836.
- PMID 22794801.)
{{cite journal}}: CS1 maint: multiple names: authors list (link
Further reading
- ISBN 978-0231161954).
