Passive immunity
In
Naturally acquired
Maternal passive immunity
Maternal passive immunity is a type of naturally acquired passive immunity, and refers to
Passive immunity is also provided through
Other species besides humans transfer maternal antibodies before birth, including primates and lagomorphs (which includes rabbits and hares).[9] In some of these species IgM can be transferred across the placenta as well as IgG. All other mammalian species predominantly or solely transfer maternal antibodies after birth through milk. In these species, the neonatal gut is able to absorb IgG for hours to days after birth. However, after a period of time the neonate can no longer absorb maternal IgG through their gut, an event that is referred to as "gut closure". If a neonatal animal does not receive adequate amounts of colostrum prior to gut closure, it does not have a sufficient amount of maternal IgG in its blood to fight off common diseases. This condition is referred to as failure of passive transfer. It can be diagnosed by measuring the amount of IgG in a newborn's blood, and is treated with intravenous administration of immunoglobulins. If not treated, it can be fatal.[citation needed]
Other
A
Antibodies from vaccination can be present in saliva and thereby may have utility in preventing infection.
Artificially acquired
Artificially acquired passive immunity is a short-term immunization achieved by the transfer of antibodies, which can be administered in several forms; as human or animal
History and applications of artificial passive immunity
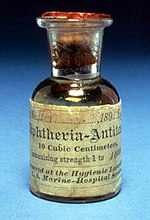
In 1888
Prior to the advent of vaccines and

In 1890 antibody therapy was used to treat
Antibody therapy is also used to treat viral infections. In 1945, hepatitis A infections, epidemic in summer camps, were successfully prevented by immunoglobulin treatment. Similarly, hepatitis B immune globulin (HBIG) effectively prevents hepatitis B infection. Antibody prophylaxis of both hepatitis A and B has largely been supplanted by the introduction of vaccines; however, it is still indicated following exposure and prior to travel to areas of endemic infection.[21]
In 1953, human
During a 1995
FDA licensed immunoglobulins
The following immunoglobulins are the immunoglobulins currently approved for use for
| Disease | Product[a] | Source | Use |
|---|---|---|---|
| Botulism | Specific equine IgG | horse | Treatment of wound and food borne forms of botulism. |
| Despeciated equine IgG[24] | |||
| Human specific IgG[24] | human | Treatment of infant botulism types A and B; brand name "BabyBIG". | |
| Cytomegalovirus (CMV) | hyperimmune IVIG | human | Prophylaxis, used most often in transplant patients.
|
| Diphtheria | Specific equine IgG | horse | Treatment of diphtheria infection. |
| Hepatitis B | Hepatitis B Ig | human | Post-exposure prophylaxis, prevention in high-risk infants (administered with Hepatitis B vaccine). |
| Hepatitis A, measles | Pooled human Ig | human serum | Prevention of Hepatitis A and measles infection, treatment of congenital or acquired immunodeficiency .
|
| Pooled human IgG | human serum | Treatment of ITP and Kawasaki disease, prevention/treatment of opportunistic infection with IgG deficiency. | |
| Rabies | Rabies Ig | human | Post-exposure prophylaxis (administered with rabies vaccine). |
| Tetanus | Tetanus Ig |
human | Treatment of tetanus infection. |
| Vaccinia | Vaccinia Ig | human | Treatment of progressive vaccinia infection including eczema and ocular forms (usually resulting from immunocompromised individuals).
|
Varicella (chicken-pox) |
Varicella-zoster Ig | human | Post-exposure prophylaxis in high risk individuals. |
| Rh disease | Rho(D) immune globulin | human | Prevention of RhD isoimmunization in Rh(D)-negative mothers[25]
|
- normal human immunoglobulin.
Passive transfer of cell-mediated immunity
The one exception to passive humoral immunity is the passive transfer of
Advantages and disadvantages
Passive immunity starts working faster than vaccines do, as the patient's immune system does not need to make its own antibodies: B cells take time to activate and multiply after a vaccine is given. Passive immunity works even if an individual has a immune system disorder that prevents them from making antibodies in response to a vaccine.[18] In addition to conferring passive immunities, breastfeeding has other lasting beneficial effects on the baby's health, such as decreased risk of allergies and obesity.[26]
A disadvantage to passive immunity is that producing antibodies in a laboratory is expensive and difficult to do. In order to produce antibodies for infectious diseases, there is a need for possibly thousands of human donors to donate blood or immune animals' blood would be obtained for the antibodies. Patients who are immunized with the antibodies from animals may develop serum sickness due to the proteins from the immune animal and develop serious allergic reactions.[6] Antibody treatments can be time-consuming and are given through an intravenous injection or IV, while a vaccine shot or jab is less time-consuming and has less risk of complication than an antibody treatment. Passive immunity is effective, but only lasts a short amount of time.[18]
See also
- Active immunity
- Immunity (medical)
- Antitoxin
- Immunoglobulin therapy
- Hyperimmune globulin
References
- ^ "Vaccines: Vac-Gen/Immunity Types". www.cdc.gov. Archived from the original on 2011-12-22. Retrieved 2015-11-20.
- ^ a b c "Microbiology/Virology/Immunology/Bacteriology/Parasitology Text Book On-line". www.microbiologybook.org. Archived from the original on 2021-05-30. Retrieved 2023-09-28.
- ^ "Passive Immunization - Infectious Diseases". Merck Manuals Professional Edition. Archived from the original on 2020-04-08. Retrieved 2015-11-12.
- PMID 25210721.
- from the original on 2017-05-09. Retrieved 2023-09-28.
- ^ a b c d "Centers for Disease Control and Prevention" (PDF). Archived (PDF) from the original on 2020-04-08. Retrieved 2017-09-07.
- ^ ISBN 0-8153-4101-6. Archivedfrom the original on 2009-06-28. Retrieved 2017-09-07..
- ^ "WHO | Exclusive breastfeeding". www.who.int. Archived from the original on 2019-10-30. Retrieved 2016-06-06.
- ISBN 9780124158474.
- medRxiv 10.1101/2022.04.28.22274443.
- S2CID 248389239.
- ^ "prophylactically". Archived from the original on 2020-04-08. Retrieved 2015-11-20.
{{cite journal}}: Cite journal requires|journal=(help) - ^ from the original on 28 September 2023. Retrieved 28 September 2023.
- ^ "Types of Immunity to a Disease | CDC". www.cdc.gov. 2022-04-06. Archived from the original on 2011-12-22. Retrieved 2023-09-28.
- PMID 18045976.
- PMID 4581249.
- ^ Silverstein, Arthur M. (1989) History of Immunology (Hardcover) Academic Press. Note: The first six pages of this text are available online at: (Amazon.com easy reader Archived 2020-04-08 at the Wayback Machine)
- ^ a b c "Passive Immunization — History of Vaccines". www.historyofvaccines.org. Archived from the original on 2020-04-08. Retrieved 2015-11-20.
- PMC 5050965.
- from the original on 2022-10-09. Retrieved 2023-09-29.
- ^ Casadevall, A., and M. D. Scharff. 1995. Return to the past: the case for antibody-based therapies in infectious diseases. Clin. Infect. Dis. 21:150-161
- ^ Mupapa, K., M. Massamba, K. Kibadi, K. Kivula, A. Bwaka, M. Kipasa, R. Colebunders, and J. J. Muyembe-Tamfum on behalf of the International Scientific and Technical Committee. 1999. Treatment of Ebola hemorrhagic fever with blood transfusions from convalescent patients. J. Infect. Dis. 179(Suppl.):S18-S23
- ^ Robbins, John B.; Schneerson, Rachel; Szu, Shousun C. (1996). "Table 8-2, U.S. Licensed Immunoglobulin For Passive Immunization". www.ncbi.nlm.nih.gov. Archived from the original on 2013-12-05. Retrieved 2023-09-29.
- ^ ISBN 978-0-16-095526-6.
- ^ "Rho(D) Immune Globulin". Drugs.com. The American Society of Health-System Pharmacists. Archived from the original on 9 January 2017. Retrieved 8 January 2017.
- ^ "Breastfeeding Overview". WebMD. Archived from the original on 2020-04-08. Retrieved 2015-11-20.
