Phantom pain
| Phantom pain | |
|---|---|
| Specialty | Neurology |
Phantom pain is a painful perception that an individual experiences relating to a limb or an organ that is not physically part of the body, either because it was removed or was never there in the first place.[1]
Sensations are reported most frequently following the amputation of a limb, but may also occur following the removal of a breast, tongue, or internal organ.[2] Phantom eye syndrome can occur after eye loss. The pain sensation and its duration and frequency varies from individual to individual.
Phantom pain should be distinguished from other conditions that may present similarly, such as phantom limb sensation and residual limb pain. Phantom limb sensation is any sensory phenomenon, except pain, which is felt at an absent limb or a portion of the limb.[3] It is estimated that up to 80% of amputees experience phantom limb sensations at some time of their lives.[4] Some experience some level of this phantom feeling in the missing limb for the rest of their lives. Residual limb pain, also referred to as stump pain, is a painful perception that originates from the residual limb, or stump, itself.[2] It is typically a manifestation of an underlying source, such as surgical trauma, neuroma formation, infection, or an improperly fitted prosthetic device.[5] Although these are different clinical conditions, individuals with phantom pain are more likely to concomitantly experience residual limb pain as well.[6]
The term "phantom limb" was first coined by American neurologist Silas Weir Mitchell in 1871.[7] Mitchell described that "thousands of spirit limbs were haunting as many good soldiers, every now and then tormenting them".[8] However, in 1551, French military surgeon Ambroise Paré recorded the first documentation of phantom limb pain when he reported that "for the patients, long after the amputation is made, say that they still feel pain in the amputated part".[8]
Signs and symptoms
The symptomatic course of phantom pain is widely variable, but the onset often presents within the first week after amputation.[2] The reported pain may be intermittent and lasting seconds to minutes, but can be continuous with acute exacerbations.[9] The duration of symptoms varies among individuals, with some reporting decreased pain over time and others reporting a more stable or even increasing trajectory.[10] Sensations may be described as shooting, stabbing, squeezing, throbbing, tingling, or burning, and sometimes feels as if the phantom part is being forced into an uncomfortable position.[11]
While the sensation often affects the part of the limb farthest from the body, such as the fingers or toes, other body parts closer to the brain, such as the arm or leg, can still experience similar sensations.
Overall, the sensations may be triggered by pressure on the remaining part of the limb, emotional stress, or changes in temperature.[14]
Causes
Individuals may experience phantom pain following surgical or traumatic amputation of a limb, removal of an organ, or in instances of congenital limb deficiency. It is most commonly observed after amputation, although less frequent cases have been reported following the removal of a breast, tongue, or eye.[2] Phantom pain is seen more often in older adults as compared to individuals with congenital limb deficiency or amputation at an early age.[15] It has also been reported that individuals with a prior history of chronic pain, anxiety, or depression are more likely to develop phantom pain than those without these risk factors.[16]
Pathophysiology
The
Peripheral mechanisms
Neuromas formed from injured nerve endings at the stump site show increased
Spinal mechanisms

In addition to peripheral mechanisms, spinal mechanisms are thought to have an influencing role in the development of phantom pain. Peripheral nerve injury can lead to the degeneration of C fibers in the
Central mechanisms
Under ordinary circumstances, the genetically determined circuitry in the brain remains largely stable throughout life. For much of the twentieth century, it was believed that no new neural circuits could be formed in the adult mammalian brain, but experiments from the 1980s onward cast this into doubt.
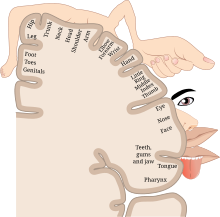
Most of the studies using functional MRI to investigate cortical remapping in humans have been in upper limb amputees. Following the loss of an arm, the majority of motor reorganization occurred as a downward shift of the hand area of the cortex onto the area of face representation, especially the lips.[21] In individuals with phantom limb pain, the reorganization was great enough to cause a change in cortical lip representation into the hand areas only during lip movements.[17] Additionally, as phantom pains in upper extremity amputees increased, there was a higher degree of medial shift of the facial motor representation.[22] It has also been found that there is a high correlation between the severity of phantom limb pain and the extent to which cortical reorganization has occurred.[22]
The neuromatrix
The neuromatrix theory, initially coined by psychologist Ronald Melzack in the 1990s, proposes that there is an extensive network connecting the
Support for the neuromatrix theory is largely from studies where cordotomy, and therefore elimination of pain signals transmitted to the brain, fail to treat phantom pains.[26] Opposition to the theory exists largely because it fails to explain why relief from phantom sensations rarely eliminates phantom pains. It also does not address how sensations can spontaneously end and how some amputees do not experience phantom sensations at all.[8] In addition, a major limitation of the neuromatrix theory is that it is difficult to be tested empirically, especially when testing painless phantom sensations.[23]
Diagnosis
Phantom pain is a clinical diagnosis based on the signs and symptoms an individual describes.[2] There are no specific laboratory studies or imaging findings that support its diagnosis.[1] However, it is important for a doctor to perform a thorough physical examination to assess for other potential causes of pain. Evaluation of the residual limb should be done to inspect for signs of infection, bursa or pressure ulcer formation, or deep tissue injury.[2] If an individual has a prosthesis, evaluation of fit and alignment should also be performed. A thorough neurological and musculoskeletal examination should be conducted, including assessment of strength, range of motion, and reflexes, to rule out any other central or peripheral causes for the pain.[12]
Management
Various methods have been used to treat phantom limb pain. There are currently no specific management guidelines or stepwise approaches to therapy. Instead, treatment involves a multimodal approach with a variety of available interventions.[27] Doctors may prescribe medications, and some antidepressants or antiepileptics have been shown to have a beneficial effect on reducing phantom limb pain.[28] Physical methods such as light massage, electrical stimulation, and hot and cold therapy have been used with variable results.[29][30]
There are many different treatment options for phantom limb pain that are actively being researched. Most treatments do not take into account the mechanisms underlying phantom pains, and are therefore difficult to investigate. However, there are a few treatment options that have been shown to alleviate pain in some patients, but these treatment options usually have a success rate of less than 30%.[8] It is important to note that this rate of success does not exceed the placebo effect.
Medication
Mirror therapy


Although the use of mirror therapy has been shown to be effective in some cases, there is still no widely accepted theory of how it works. According to a 2017 paper that reviewed a wide range of studies using mirror therapy, patients may experience reduced phantom pains after four weeks of treatment.[38] The study goes on to say that while the exact mechanism of mirror therapy isn't completely understood, it is a safe and inexpensive option for patients to consider.[38]
Little research was published on mirror therapy before 2009, and much of the research since then has been of low quality.[39] Out of 115 publications between 2012 and 2017 that investigated the use of mirror therapy for phantom pain, a 2018 review found only 15 studies whose scientific results should be considered. From these 15 studies, the reviewers concluded that mirror therapy is an effective tool to reduce both the duration and intensity of phantom pain.[40]
Current theories on how mirror therapy may reduce phantom pain have largely come from studies investigating changes in the brain using functional MRI. There is evidence to show a reduction and reversal of cortical reorganization within the somatosensory cortex following mirror therapy.[41] Since maladaptive changes within cortical regions of the brain are proposed to be a central mechanism of phantom pain, a reversal of this remapping is thought to alleviate pain.
Graded motor imagery
Graded motor imagery was initially developed to help patients suffering from complex regional pain syndrome, but has since expanded to other chronic pain conditions, including phantom pain.[42] The treatment is thought to work in a similar fashion as mirror box therapy, where maladaptive cortical reorganization is reversed and there is no longer a functional connection between movement and pain. A recent systematic review and meta-analysis provided support for the use of graded motor imagery to help reduce the severity of phantom pain in amputees.[43]
Motor execution with biofeedback
Phantom motor execution with biofeedback is a newer therapeutic intervention that takes advantage of augmented and virtual reality.[44] During these sessions, patients wear virtual reality goggles that allow them to visualize their phantom limb as a normal, intact limb. They are then able to participate in different interactive games, such as reaching for and grasping objects. It is theorized that by doing so, there becomes a 'match' between the visual and somatosensory systems, which may lead to decreased phantom pain.[45] Importantly, as opposed to conventional mirror box therapy, the ability to interact with virtual reality games may increase patients' participation and result in improved outcomes.[44] Numerous case reports and case series have shown promising results, but a more robust analysis is likely needed to substantiate these claims.[46][47][48]
Deep brain stimulation

Epidemiology
It is estimated that the reported prevalence of phantom pain may be as high as 80% among amputees.[4] It is more commonly observed in the adult population, with less common occurrences seen among individuals with amputations at an early age or in those with congenital limb deficiency.[15] Gender, side of limb loss, and etiology of amputation have not been shown to affect the onset of phantom limb pain.[2] One investigation of lower limb amputation observed that as stump length decreased, and therefore length of the phantom limb increased, there was a greater incidence of moderate and severe phantom pain.[8] It has also been reported that individuals with bilateral amputations, especially in the lower limbs, experience phantom pain more commonly.[52][53]
See also
References
- ^ PMID 28846343, retrieved 2024-01-19
- ^ a b c d e f g knadmin (2017-03-03). "Phantom Pain". PM&R KnowledgeNow. Retrieved 2024-01-19.
- PMID 27375755.
- ^ PMID 30583983.
- S2CID 222156523.
- PMID 29123664.
- S2CID 31375410.
- ^ S2CID 42653229.
- PMID 6624883.
- S2CID 21102803.
- ^ PMID 36288580.
- ^ a b "Phantom Limb Pain". Physiopedia. Retrieved 2024-01-19.
- S2CID 23797588.
- ^ "Phantom Limb Pain: What is It, Causes, Treatment & Outcome". Cleveland Clinic. Retrieved 2024-01-17.
- ^ S2CID 253072027.
- S2CID 53864052.
- ^ PMID 9762952.
- PMID 30672368.
- PMID 27296638.
- PMID 14757926.
- ^ PMID 32428706.
- ^ PMID 11331390.
- ^ S2CID 42209339.
- S2CID 20967995.
- PMID 1566028.
- PMID 20433282.
- PMID 33490849.
- ^ PMID 20303003.
- PMID 22935086.
- PMID 22110933.
- S2CID 26515957.
- PMID 16266358.
- PMID 14970960.
- PMID 16129989.
- S2CID 45858493.
- PMID 18349204.
- ^ S2CID 4819370.
- ^ a b Mirror therapy: A potential intervention for pain management, Wittkopf,Johnson,2017 Nov;63(11):[1]
- PMID 27256539.
Up to the 26th November 2015, 85 articles were retrieved on the Medline, Cochrane and Embase databases with using the keywords phantom limb and mirror therapy. It was noted that from 2009, the number of articles increased markedly (Fig. 1), showing increased interest in MT following amputation.
- PMID 30447854.
It is a valid, simple, and inexpensive treatment for PLP. The methodological quality of most publications in this field is very limited, highlighting the need for additional, high-quality studies to develop clinical protocols that could maximise the benefits of MT for patients with PLP.
- S2CID 44669695.
- ^ "Graded Motor Imagery". Physiopedia. Retrieved 2024-01-26.
- PMID 37214633.
- ^ PMID 36320223.
- PMID 28691602.
- S2CID 22995879.
- S2CID 4846236.
- PMID 16640472.
- ^ PMID 30407905.
- S2CID 29788874.
- PMID 30774224.
- S2CID 38138668.
- PMID 12551807.
External links
- MacLachlan, Malcolm; McDonald, Dympna; Waloch, Justine (2004), "Mirror Treatment of Lower Limb Phantom Pain: A Case Study" (PDF), Disability and Rehabilitation, 26 (14/15): 901–904, S2CID 36325980
- Richardson, Cliff; Glenn, Sheila; Horgan, Maureen; Nurmikko, Turo (October 2007), "A Prospective Study of Factors Associated with the Presence of Phantom Limb Pain Six Months After Major Lower Limb Amputation in Patients with Peripheral Vascular Disease", The Journal of Pain, 8 (10): 793–801, PMID 17631056
