Conjunctivitis
| Conjunctivitis | |
|---|---|
| Other names | Pink eye |
Handwashing[1] | |
| Treatment | Based on underlying cause[3] |
| Frequency | 3–6 million per year (US)[1][3] |
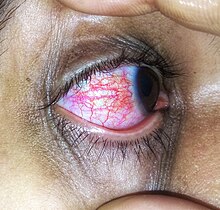
Conjunctivitis, also known as pink eye,[4] is inflammation of the outermost layer of the white part of the eye and the inner surface of the eyelid.[5] It makes the eye appear pink or reddish.[1] Pain, burning, scratchiness, or itchiness may occur.[1] The affected eye may have increased tears or be "stuck shut" in the morning.[1] Swelling of the white part of the eye may also occur.[1] Itching is more common in cases due to allergies.[3] Conjunctivitis can affect one or both eyes.[1]
The most common infectious causes in adults are viral, whereas in children bacterial causes predominate.
Prevention is partly by
About 3 to 6 million people get acute conjunctivitis each year in the United States.[1][3] Typically, people get better in one or two weeks.[1][3] If visual loss, significant pain, sensitivity to light or signs of herpes occur, or if symptoms do not improve after a week, further diagnosis and treatment may be required.[3] Conjunctivitis in a newborn, known as neonatal conjunctivitis, may also require specific treatment.[1]
Signs and symptoms

Conjunctivitis is identified by inflammation of the conjunctiva, manifested by irritation and redness. Examination using a slit lamp (biomicroscope) may improve diagnostic accuracy. Examination of the palpebral conjunctiva, that overlying the inner aspects of the eyelids, is usually more diagnostic than examination of the bulbal conjunctiva, that overlying the sclera.[citation needed]
Viral
Approximately 80% of cases of conjunctivitis in adults and less than 20% in children are due to viruses, with 65% to 90% of these cases being attributed to adenoviruses.[8][6] Viral conjunctivitis is often associated with an infection of the upper respiratory tract, a common cold, or a sore throat. Other associated signs may include pre-auricular lymph node swelling and contact with another person with a red eye.[6] Eye pain may be present if the cornea is also involved.[6] Its symptoms include excessive watering and itching. The discharge in viral conjunctivitis is usually (but not always) watery in nature.[6] The infection usually begins in one eye but may spread easily to the other eye.[citation needed]
Viral conjunctivitis manifests as a fine, diffuse pinkness of the conjunctiva which may be mistaken for
Allergic

Bacterial

Bacteria are responsible for approximately 70% of conjunctivitis in children and less than 20% of cases in adults.

Bacteria such as
Chemical
Chemical eye injury may result when an
Irritant or toxic conjunctivitis is primarily marked by redness. If due to a chemical splash, it is often present in only the lower conjunctival sac. With some chemicals, above all with caustic alkalis such as
Biomarkers
Omics technologies have been used to identify biomarkers that inform on the emergence and progression of conjunctivitis. For example, in chronic inflammatory cicatrizing conjunctivitis, active
Other

Inclusion conjunctivitis of the newborn is a conjunctivitis that may be caused by the bacterium Chlamydia trachomatis, and may lead to acute,
Causes
Infective conjunctivitis is most commonly caused by a virus.[3] Bacterial infections, allergies, other irritants, and dryness are also common causes. Both bacterial and viral infections are contagious, passing from person to person or spread through contaminated objects or water. Contact with contaminated fingers is a common cause of conjunctivitis. Bacteria may also reach the conjunctiva from the edges of the eyelids and the surrounding skin, from the nasopharynx, from infected eye drops or contact lenses, from the genitals or the bloodstream.[17] Infection by human adenovirus accounts for 65% to 90% of cases of viral conjunctivitis.[18]
Viral
Bacterial
The most common causes of acute bacterial conjunctivitis are
Allergic
Conjunctivitis may also be caused by allergens such as pollen, perfumes, cosmetics, smoke,[22][unreliable medical source?] dust mites, Balsam of Peru,[23] or eye drops.[24] The most frequent cause of conjunctivitis is allergic conjunctivitis and it affects 15% to 40% of the population.[25] Allergic conjunctivitis accounts for 15% of eye related primary care consultations; most including seasonal exposures in the spring and summer or perpetual conditions.[26]
Other
- Computer vision syndrome
- Dry eye syndrome
- autoimmune cross-reactivity following certain bacterial infections. Reactive arthritis is highly associated with HLA-B27. Conjunctivitis is associated with the autoimmune disease relapsing polychondritis.[27][28]
Diagnosis

Cultures are not often taken or needed as most cases resolve either with time or typical antibiotics. If bacterial conjunctivitis is suspected, but no response to topical antibiotics is seen, swabs for bacterial culture should be taken and tested. Viral culture may be appropriate in epidemic case clusters.[29]
A patch test is used to identify the causative allergen in allergic conjunctivitis.[30]
Although conjunctival scrapes for
Classification
Conjunctivitis may be classified either by cause or by extent of the inflamed area.[citation needed]
Causes
- Allergy
- Bacteria
- Viruses
- Chemicals
- Autoimmune
Neonatal conjunctivitis is often grouped separately from bacterial conjunctivitis because it is caused by different bacteria than the more common cases of bacterial conjunctivitis.[citation needed]
By extent of involvement
Blepharoconjunctivitis is the dual combination of conjunctivitis with blepharitis (inflammation of the eyelids).[citation needed]
Keratoconjunctivitis is the combination of conjunctivitis and keratitis (corneal inflammation).[citation needed]
Blepharokeratoconjunctivitis is the combination of conjunctivitis with blepharitis and keratitis. It is clinically defined by changes of the lid margin, meibomian gland dysfunction, redness of the eye, conjunctival chemosis and inflammation of the cornea.[33]
Differential diagnosis
Some more serious conditions can present with a red eye, such as infectious keratitis, angle-closure glaucoma, or iritis. These conditions require the urgent attention of an ophthalmologist. Signs of such conditions include decreased vision, significantly increased sensitivity to light, inability to keep the eye open, a pupil that does not respond to light, or a severe headache with nausea.
A more comprehensive differential diagnosis for the red or painful eye includes:[34]
- Corneal abrasion
- Subconjunctival hemorrhage
- Pinguecula
- Blepharitis
- Dacryocystitis
- Keratoconjunctivitis sicca(dry eye)
- Keratitis
- Herpes simplex
- Herpes zoster
- Episcleritis - an inflammatory condition that produces a similar appearance to conjunctivitis, but without discharge or tearing
- Uveitis
- Acute angle-closure glaucoma
- Endophthalmitis
- Orbital cellulitis
Prevention
The most effective prevention is good hygiene, especially avoiding rubbing the eyes with infected hands. Vaccination against some of the causative pathogens such as Haemophilus influenzae, pneumococcus, and Neisseria meningitidis is also effective.[35]
Povidone-iodine eye solution has been found to prevent neonatal conjunctivitis.[36] It is becoming more commonly used globally because of its low cost.[36]
Management
Conjunctivitis resolves in 65% of cases without treatment, within 2–5 days. The prescription of antibiotics is not necessary in most cases.[37]
Viral
Viral conjunctivitis usually resolves on its own and does not require any specific treatment.[3] Antihistamines (e.g., diphenhydramine) or mast cell stabilizers (e.g., cromolyn) may be used to help with the symptoms.[3] Povidone-iodine has been suggested as a treatment, but as of 2008, evidence to support it was poor.[38]
Allergic
For allergic conjunctivitis, cool water poured over the face with the head inclined downward constricts capillaries, and
Bacterial
Bacterial conjunctivitis usually resolves without treatment.
The choice of antibiotic varies based on the strain or suspected strain of bacteria causing the infection.
When investigated as a treatment, povidone-iodine ophthalmic solution has also been observed to have some effectiveness against bacterial and chlamydial conjunctivitis, with a possible role suggested in locations where topical antibiotics are unavailable or costly.[42]
Chemical
Conjunctivitis due to chemicals is treated via
Epidemiology
Conjunctivitis is the most common eye disease.[44] Rates of disease is related to the underlying cause which varies by the age as well as the time of year. Acute conjunctivitis is most frequently found in infants, school-age children and the elderly.[17] The most common cause of infectious conjunctivitis is viral conjunctivitis.[25]
It is estimated that acute conjunctivitis affects 6 million people annually in the United States.[3]
Some seasonal trends have been observed for the occurrence of different forms of conjunctivitis. In the northern hemisphere, the occurrence of bacterial conjunctivitis peaks from December to April, viral conjunctivitis peaks in the summer months and allergic conjunctivitis is more prevalent throughout the spring and summer.[17]
History
An adenovirus was first isolated by Rowe et al. in 1953. Two years later, Jawetz et al. published on epidemic keratoconjunctivitis.[45]: 437 "Madras eye" is a colloquial term that has been used in India for the disease.
Outbreak in Pakistan
In September 2023, a significant outbreak of conjunctivitis occurred in Pakistan. The outbreak began in Karachi and quickly spread to Lahore, Rawalpindi, and Islamabad. By the end of the month, over 86,133 cases had been reported in Punjab alone. The rapid spread of the disease led to the temporary closure of schools in the region. This event marked one of the largest outbreaks of Pink Eye in the country's recent history.[46][47][48][49]
Society and culture
Conjunctivitis imposes economic and social burdens. The cost of treating bacterial conjunctivitis in the United States was estimated to be $377 million to $857 million per year.[3] Approximately 1% of all primary care office visits in the United States are related to conjunctivitis. Approximately 70% of all people with acute conjunctivitis present to primary care and urgent care.[3]
See also
References
- ^ a b c d e f g h i j k l m n o p q r s "Facts About Pink Eye". National Eye Institute. November 2015. Archived from the original on 9 March 2016. Retrieved 8 March 2016.
- ISBN 978-0-323-46132-0.
- ^ PMID 24150468.
- ^ "What is Viral Conjunctivitis a.k.a. Sore Eyes? | National Institutes of Health".
- S2CID 245084568.
- ^ S2CID 266433325.
- PMID 31082078, retrieved 23 May 2023
- PMID 24150468.
- S2CID 34371872.
- ^ "Pink Eye (Conjunctivitis)". MedicineNet. Archived from the original on 22 June 2013.
- ^ "Acute Bacterial Conjunctivitis – Eye Disorders". Merck Manuals Professional Edition. Archived from the original on 28 December 2016. Retrieved 31 December 2016.
- ISBN 978-0-9904491-1-9.
- ^ S2CID 38124735.
- ^ PMID 18592066.
- PMID 32313985.
- ^ ISBN 978-0-7817-8215-9.
- ^ S2CID 20629824.
- PMID 29735838.
- ^ ISBN 978-0-323-05751-6.
- PMID 19836177.
- ^ CDC (2 October 2017). "Protect Yourself From Pink Eye". Centers for Disease Control and Prevention. Retrieved 7 December 2018.
- ^ "Allergic Conjunctivitis". familydoctor.org. Archived from the original on 6 September 2015. Retrieved 18 September 2015.
- ]
- ^ "What Is Allergic Conjunctivitis? What Causes Allergic Conjunctivitis?". medicalnewstoday.com. Archived from the original on 16 March 2010. Retrieved 6 April 2010.
- ^ S2CID 80882721.
- PMID 26600465.
- S2CID 205754989.
- PMID 24461536.
- ISBN 978-1-4160-2447-7, retrieved 23 May 2023
- ISBN 978-0-7817-0269-0. Archivedfrom the original on 5 July 2014. Retrieved 23 April 2014.
- PMID 27758983.
- ISBN 978-3-030-76525-5, retrieved 10 December 2023
- PMID 27236587.
- ^ a b Longo DL (2012). "Disorders of the Eye(Horton JC)". Harrison's Principles of Internal Medicine. McGra-Hill.
- ^ "Protect Yourself From Pink Eye". Centers for Disease Control and Prevention. 2 October 2017. Retrieved 18 October 2017.
- ^ PMID 17491857.
- S2CID 45899988.
- ISBN 978-0-7506-7576-5. Archivedfrom the original on 3 December 2016.
- S2CID 5316455.
- PMID 19910590.
- ^ PMID 36912752.
- PMID 12429243.
- ^ "Conjunctivitis". American Optometric Association. Retrieved 15 March 2024.
- ISBN 978-0-7817-8589-1. Archivedfrom the original on 15 August 2016.
- PMID 26077630.
- ^ "From pink eye to blindness". 28 September 2023.
- ^ "86,133 pink eye cases in Punjab in September and counting". 28 September 2023.
- ^ Ahmed S (27 September 2023). "Punjab Announces Holiday for Schools Amid Pink Eye Outbreak". Propakistani.
- ^ "85 new cases of Pink Eye infection reported in Pakistan's Lahore - ET HealthWorld".
External links
- "Pink Eye". MedlinePlus. U.S. National Library of Medicine.
- "Metabolomics for Ocular Surface Disease". MSBB Group, Leiden University.
