Pituitary adenoma
| Pituitary adenoma | |
|---|---|
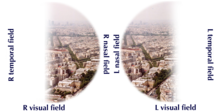 | |
| Visual field loss in bitemporal hemianopsia: peripheral vision loss affecting both eyes, resulting from a tumor – typically a pituitary adenoma – putting pressure on the optic chiasm | |
| Specialty | Oncology, endocrinology |
Pituitary adenomas are
Non-invasive and non-secreting pituitary adenomas are considered to be
Adenomas exceeding 10 mm (0.39 in) in size are defined as macroadenomas, with those smaller than 10 mm (0.39 in) referred to as microadenomas. Most pituitary adenomas are microadenomas and have an estimated prevalence of 16.7% (14.4% in
Pituitary macroadenomas are the most common cause of hypopituitarism.[4][5]
While pituitary adenomas are common, affecting approximately one in 6 of the general population, clinically active pituitary adenomas that require surgical treatment are more rare, affecting approximately one in 1,000 of the general population.[6]
Signs and symptoms
Physical
Hormone secreting pituitary adenomas cause one of several forms of hyperpituitarism. The specifics depend on the type of hormone. Some tumors secrete more than one hormone, the most common combination[7] being GH and prolactin, which present as unexpected bone growth and unexpected lactation (in both men and women).[citation needed]
A patient with pituitary adenoma may present with
Also, a pituitary adenoma can cause symptoms of increased intracranial pressure. Prolactinomas often start to give symptoms especially during pregnancy, when the increased hormone level estrogen can increase the tumor's growth rate.[9]
Various types of headaches are common in patients with pituitary adenomas. The adenoma may be the prime causative factor behind the headache or may serve to exacerbate a headache caused by other factors. Amongst the types of headaches experienced are both chronic and episodic
Compressive symptoms of pituitary adenomas (visual field deficits, decreased visual acuity, headaches) are more commonly seen with macroadenomas (which are greater than 10 mm in diameter) than with microadenomas (which are less than 10 mm in diameter).[14]
Non-secreting adenomas can go undetected for an extended time because no obvious abnormalities are seen; the gradual reduction in normal activities due to decreased production of hormones is rather less evident. For example, insufficient adrenocorticotropic hormone means that the adrenal glands will not produce sufficient cortisol, resulting in slow recovery from illness, inflammation, and chronic fatigue; insufficient growth hormone in children and adolescents leads to diminished stature but which can have many other explanations.[citation needed]
Psychiatric
Various psychiatric manifestations have been associated with pituitary disorders including pituitary adenomas. Psychiatric symptoms such as depression, anxiety[15] apathy, emotional instability, easy irritability and hostility have been noted.[16]
Complications
- Acromegaly is a syndrome that results when the anterior pituitary gland produces excess growth hormone (GH). Approximately 90–95% of acromegaly cases are caused by a pituitary adenoma and it most commonly affects middle aged adults,[17] Acromegly can result in severe disfigurement, serious complicating conditions, and premature death if unchecked. The disease which is often also associated with gigantism, is difficult to diagnose in the early stages and is frequently missed for many years, until changes in external features, especially of the face, become noticeable with the median time from the development of initial symptoms to diagnosis being twelve years.[18]
- Cushing's disease may cause fatigue, weight gain, fatty deposits around the abdomen and lower back (truncal obesity) and face ("moon face"), stretch marks (glucose intolerance, and various infections. In women, it may cause excessive growth of facial hair (hirsutism) and in men erectile dysfunction. Psychiatric manifestations may include depression, anxiety, easy irritability, and emotional instability. It may also result in various cognitive difficulties.[citation needed]
- Hyperpituitarism is a disease of the anterior lobe of the pituitary gland which is usually caused by a functional pituitary adenoma and results in hypersecretion of adenohypophyseal hormones such as growth hormone; prolactin; thyrotropin; luteinizing hormone; follicle-stimulating hormone; and adrenocorticotropic hormone.[citation needed]
- corticosteroids and if necessary surgical intervention.[21]
- antidiuretic hormone vasopressin that causes severe thirst and excessive production of very dilute urine (polyuria) which can lead to dehydration. Vasopressin is produced in the hypothalamus and is then transported down the pituitary stalk and stored in the posterior lobe of the pituitary gland which then secretes it into the bloodstream.[22]
As the pituitary gland is in close proximity to the brain, invasive adenomas may invade the
Risk factors
Multiple endocrine neoplasia
Adenomas of the anterior pituitary gland are a major clinical feature of
Carney complex
Familial isolated pituitary adenoma
Familial isolated pituitary adenoma (FIPA) is a term that is used to identify a condition that displays an
Genetics of FIPA
FIPA has two known genetic causes,
X-LAG is a rare syndrome of very early childhood onset pituitary tumors/hyperplasia that leads to growth hormone excess and severe overgrowth and pituitary gigantism.
Mechanism
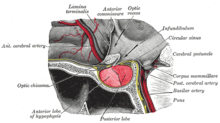
The pituitary gland or hypophysis is often referred to as the "master gland" of the human body. Part of the
The pituitary gland is divided into two lobes, the anterior lobe (which accounts for two thirds of the volume of the gland), and the posterior lobe (one third of the volume) separated by the pars intermedia.[7]
The
The pituitary gland's anterior lobe (adenohypophysis) is a true gland which produces and secretes six different hormones: thyroid-stimulating hormone (TSH), adrenocorticotropic hormone (ACTH), follicle-stimulating hormone (FSH), luteinizing hormone (LH), growth hormone (GH), and prolactin (PRL).[46]
Diagnosis
Diagnosis of pituitary adenoma can be made, or at least suspected, by a constellation of related symptoms presented above.[8]
The differential diagnosis includes pituitary tuberculoma, especially in developing countries and in immumocompromised patients.
Classification
Unlike tumors of the posterior Pituitary, Pituitary adenomas are classified as endocrine tumors (not brain tumors). Pituitary adenomas are classified based upon anatomical, histological and functional criteria.[48]
- Anatomically pituitary tumors are classified by their size based on radiological findings; either microadenomas (less than <10 mm) or macroadenomas (equal or greater than ≥10 mm).
- Classification based on radioanatomical findings places adenomas into 1 of 4 grades (I–IV):[49]
- Stage I: microadenomas (<1 cm) without sella expansion.
- Stage II: macroadenomas (≥1 cm) and may extend above the sella.
- Stage III: macroadenomas with enlargement and invasion of the floor or suprasellar extension.
- Stage IV: destruction of the sella.
- Histological classification utilizes an immunohistological characterization of the tumors in terms of their hormone production.hematoxylin and eosin. This classification has fallen into disuse, in favor of a classification based on what type of hormone is secreted by the tumor. Approximately 20–25% of adenomas do not secrete any readily identifiable active hormones ('non-functioning tumors') yet they are still sometimes referred to as 'chromophobic'.[citation needed]
- Functional classification is based upon the tumors endocrine activity as determined by immunohistochemical staining.[50] The "Percentage of hormone production cases" values are the fractions of adenomas producing each related hormone of each tumor type as compared to all cases of pituitary tumors, and does not directly correlate to the percentages of each tumor type because of smaller or greater incidences[spelling?] of absence of secretion of the expected hormone. Thus, non secretive adenomas may be either null cell adenomas or a more specific adenoma that, however, remains non-secretive.[citation needed]
- Any type of pituitary adenocarcinoma listed in the table below may cause compressive symptoms due to local expansion in addition to the systemic effects of secreted hormones listed in the pathology column.[citation needed]
- Null cell adenomas by definition do not secrete hormones, but they commonly cause compressive effects on the pituitary stalk (stalk effect). This leads to decreased levels of dopamine from the hypothalamus reaching the anterior pituitary gland. Dopamine exerts an inhibitory effect on prolactin secretion. With the absence of this inhibitory effect, prolactin levels increase and are often increased in null cell adenomas. This leads to symptoms of hypogonadism.[14]
| Type of adenoma | Secretion | Staining | Pathology | Percentage of hormone production cases | Percentage of silent cases[51] |
|---|---|---|---|---|---|
| lactotrophic adenomas (prolactinomas) | secrete prolactin | acidophilic | impotence |
30%[52] | <9%[51] |
somatotrophic adenomas |
secrete growth hormone (GH) | acidophilic | acromegaly in adults; gigantism in children | 15%[52] | <9%[51] |
corticotrophic adenomas |
secrete adenocorticotropic hormone (ACTH) | basophilic | Cushing's disease | 2–6%[14] | 10% |
gonadotrophic adenomas |
secrete luteinizing hormone (LH), follicle-stimulating hormone (FSH) and their subunits | basophilic |
usually do not cause symptoms, occasionally hypergonadism[14] | 10%[52] | 73%[51] |
thyrotrophic adenomas (rare) |
secrete thyroid-stimulating hormone (TSH) | basophilic to chromophobic |
occasionally hyperthyroidism,[53] usually do not cause symptoms | Less than 1%[52] | <9% |
| null cell adenomas | do not secrete hormones | may stain positive for synaptophysin | Asymptomatic or hypogonadism[14] | 25% of pituitary adenomas are nonsecretive[52] | 1%[51] |
-
Somatotroph pituitary adenoma, showing acidophilic cytoplasm
-
A silent gonadotroph pituitary adenoma which is, in this case, eosinophilic (contrary to normal, basophilic, gonadotroph cells)
-
True null cell adenomas are typically composed of uniform, mildly atypical cells with chromophobic cytoplasm. This case has papillary architecture similar to gonadotroph adenomas.[54]
Pituitary incidentalomas
Pituitary incidentalomas are pituitary tumors that are characterized as an
It has been recommended in the current Clinical Practice Guidelines (2011) by the Endocrine Society – a professional, international medical organization in the field of endocrinology and metabolism – that all patients with pituitary incidentalomas undergo a complete medical history and physical examination, laboratory evaluations to screen for hormone hypersecretion and for hypopituitarism. If the lesion is in close proximity to the optic nerves or optic chiasm, a visual field examination should be performed. For those with incidentalomas which do not require surgical removal, follow up clinical assessments and neuroimaging should be performed as well follow-up visual field examinations for incidentalomas that abut or compress the optic nerve and chiasm and follow-up endocrine testing for macroincidentalomas.[56]
Ectopic pituitary adenoma
An ectopic (occurring in an abnormal place) pituitary adenoma is a rare type of tumor which occurs outside of the
Metastases to the pituitary gland
Carcinomas that metastasize into the pituitary gland are uncommon and typically seen in the elderly,[59][60] with lung and breast cancers being the most prevalent,[61] In breast cancer patients, metastases to the pituitary gland occur in approximately 6–8% of cases.[62]
Symptomatic pituitary metastases account for only 7% of reported cases. In those who are symptomatic
Treatment
Treatment options depend on the type of tumor and on its size:
- MRI) to detect any increase in size or mass effect on nearby structures. If medical therapy fails, the second option is usually transphenoidal pituitary surgery.[64] A third line therapy is radiation therapy, proton therapy to shrink the tumor.[64]
- Thyrotropinomas are treated with transsphenoidal pituitary surgery as the first line treatment option.[64] Medical therapy is a second line treatment, and thyrotropinomas respond to treatment with somatostatin receptor ligands such as octreotide or lanreotide.[64] In people with thyrotropinomas, treatment with somatostatin receptor ligands normalized thyroid hormone levels in 80-90% of people, and 42% of people had a decreased tumor size.[64]
- Somatotrophic adenomas are primarily treated with transsphenoidal pituitary surgery, especially if symptoms of acromegaly are present.IGF-1) levels in studies.[14] The growth hormone receptor antagonist pegvisomant is also used in the treatment of somatotrophic adenomas. Pegvisomant blocks the action of growth hormone. It can either be used as monotherapy or combined with a somatostatin analog.[65]
- Corticotropinomas are primarily treated with transsphenoidal pituitary surgery, especially if signs and symptoms of Cushing syndrome are present.[64] Medication therapy is second line, and includes steroidogenesis inhibitors (ketoconazole, metyrapone, osilodrostat, etomidate or mitotane) which decrease production of cortisol, pituitary blockers such as somatostatin receptor ligand pasireotide or the dopamine agonist cabergoline, or the glucocorticoid receptor antagonist mifepristone.[64] These medications can be combined for a synergistic effect. Medication therapy is often used in conjunction with radiation therapy for corticotropinomas.[64]
- Surgery is a common treatment for pituitary tumors. The normal approach is trans-sphenoidal adenectomy, which usually can remove the tumor without affecting the brain or optic nerves.[66]
- Radiation is also used to treat pituitary adenomas. Examples include external beam or proton beam radiation therapy or stereotactic radiosurgery. External radiation of pituitary adenomas can arrest tumor growth for several years but pituitary failure develops within 10 years in most patients necessitating lifelong hormone replacement.[14] Radiation therapy for pituitary adenomas is associated with a four-fold increase in mortality due to cerebrovascular disease.[14] Lifelong monitoring of pituitary hormones is recommended after radiation therapy as hypopituitarism developed in 17% of those undergoing radiation therapy.[64]
See also
References
- ^ a b Pituitary Tumors Treatment (PDQ®)–Health Professional Version NIH National Cancer Institute
- ^ S2CID 16595581.
- PMID 18684022.
- S2CID 208791062.
- ^ Hyperthyroidism unmasked several years after the medical and radiosurgical treatment of an invasive macroprolactinoma inducing hypopituitarism: a case report. L Foppiani, A Ruelle, P Cavazzani, P del Monte – Cases Journal, 2009
- PMID 16968795.
- ^ S2CID 27780583.
- ^ a b "Acromegaly and Gigantism". The Lecturio Medical Concept Library. Retrieved 26 June 2021.
- PMID 26074878.
- PMID 15888539.
- PMID 14617728.
- S2CID 1681207.
- S2CID 9475046.
- ^ S2CID 212417223.
- PMID 19073833.
- PMID 15939968.
- ^ "Acromegaly and Gigantism". Merck.com. Retrieved 26 October 2010.
- S2CID 221550204.
- PMID 16378774.
- PMID 10997535.
- PMID 11561045.
- S2CID 24638358.
- PMID 31855373. Retrieved 26 June 2021.
- PMID 21454234.
- PMID 21249756.
- ^ a b Carney Syndrome at eMedicine
- S2CID 20522398.
- PMID 3951243.
- PMID 7477198.
- PMID 15761655.
- S2CID 52924983.
- ^ PMID 16787992.
- PMID 29440248.
- ^ Valdes-Socin, Hernan & Poncin, J & Stevens, V & Stevenaert, Achille & Beckers, A. (2000). Familial isolated pituitary adenomas unrelated to MEN1 mutations: A follow-up of 27 patients. Ann Endocrinol (Paris). 61.
- ^ PMID 23371967.
- PMID 17244780.
- ^ PMID 25470569.
- PMID 20685857.
- ^ PMID 26187128.
- ^ PMID 25712922.
- PMID 28457479.
- PMID 28049632.
- PMID 26935837.
- ^ Dhruve
- ISBN 978-0-203-45043-7.[page needed]
- PMID 19900438.
- PMID 17657390.
- ^ PMID 12890801.
- S2CID 32722411.
- S2CID 8095432.
- ^ PMID 30020466.
- ^ ISBN 978-0-7817-9079-6.
- S2CID 27660512.
- PMID 30020466.)"
- "This article has been published under the terms of the Creative Commons Attribution License (CC BY; https://creativecommons.org/licenses/by/4.0/ - PMID 21474687.
- PMID 21474686.
- PMID 22430769.
- ISBN 92-832-2417-5
- PMID 12470187.
- PMID 11516470.
- PMID 9647174.
- ^ Daniel R. Fassett, M.D.; William T. Couldwell, M.D., PhD;Medscape:Metastases to the Pituitary Gland [1]
- PMID 14764764.
- ^ S2CID 258310567.
- S2CID 19588354.
- ^ Transsphenoidal Surgery FAQ Neuroendocrine Clinical Center, Massachusetts General Hospital/Harvard Medical School. Retrieved November 25, 2016



![True null cell adenomas are typically composed of uniform, mildly atypical cells with chromophobic cytoplasm. This case has papillary architecture similar to gonadotroph adenomas.[54]](http://upload.wikimedia.org/wikipedia/commons/thumb/4/40/Histopathology_of_a_true_null_cell_adenoma.jpg/120px-Histopathology_of_a_true_null_cell_adenoma.jpg)