Polycystic kidney disease
| Polycystic kidney disease | |
|---|---|
| Other names | Kidney - polycystic[1] |
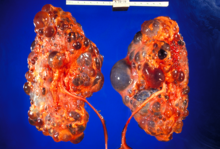 | |
| Severely affected polycystic kidneys removed at time of transplantation | |
| Specialty | Nephrology |
| Symptoms | Abdominal pain[1] |
| Types | ADPKD[2] and ARPKD[3] |
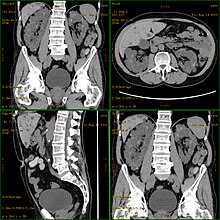
| Diagnostic method | MRI, CT scan, Ultrasound[1] |
| Treatment | Antihypertensives, Life style management[4] |
Polycystic kidney disease (PKD or PCKD, also known as polycystic kidney syndrome) is a
PKD is caused by abnormal genes that produce a specific abnormal protein; this protein has an adverse effect on tubule development. PKD is a general term for two types, each having their own pathology and genetic cause: autosomal dominant polycystic kidney disease (ADPKD) and autosomal recessive polycystic kidney disease (ARPKD). The abnormal gene exists in all cells in the body; as a result, cysts may occur in the liver, seminal vesicles, and pancreas. This genetic defect can also cause aortic root aneurysms, and aneurysms in the circle of Willis cerebral arteries, which if they rupture, can cause a subarachnoid hemorrhage.
Diagnosis may be suspected from one, some, or all of the following: new onset flank pain or red urine; a positive family history; palpation of enlarged kidneys on physical exam; an incidental finding on abdominal
Complications include hypertension due to the activation of the
Signs and symptoms
Signs and symptoms include high blood pressure, headaches, abdominal pain, blood in the urine, and excessive urination.[1] Other symptoms include pain in the back, and cyst formation (renal and other organs).[9]
Cause
PKD is caused by abnormal genes which produce a specific abnormal protein which has an adverse effect on tubule development. PKD is a general term for two types, each having their own pathology and genetic cause: autosomal dominant polycystic kidney disease (ADPKD) and autosomal recessive polycystic kidney disease (ARPKD).[10][11]
Autosomal dominant

- Gene PKD1 is located on chromosome 16 and codes for a protein involved in regulation of cell cycle and intracellular calcium transport in epithelial cells, and is responsible for 85% of the cases of ADPKD.[16]
- Gene PKD2 is identified, using genetic linkage study,cation channels, with inward selectivity for K>Na>>Ca and outward selectivity for Ca2+ ≈ Ba2+ > Na+ ≈ K+, are coded for by PKD2 on chromosome 4.[20]
- PKD3 recently appeared in research papers as a postulated third gene.kidney function.[11]
Autosomal recessive
Mechanism

Both autosomal dominant and autosomal recessive polycystic kidney disease cyst formation are tied to abnormal
The disease is characterized by a ‘second hit’ phenomenon, in which a mutated dominant allele is inherited from a parent, with cyst formation occurring only after the normal, wild-type gene sustains a subsequent second genetic ‘hit’, resulting in renal tubular cyst formation and disease progression.[21]
PKD results from defects in the
Diagnosis
Polycystic kidney disease can be ascertained via a
Natural history
Most cases progress to bilateral disease in adulthood.[12]
Treatment

In 2018, Jynarque (Tolvaptan) was introduced [24] as the first FDA-approved treatment for PKD. In a recent long-term study, patients using Tolvaptan had a 6.4% higher kidney function after 5 years compared to standard of care.[25] In 2019, a team of researchers at UCSB found that a ketogenic diet might be able to halt, or even reverse progression in mice,[26] and the results of a first human case series study are showing potential benefit.[27] The results of a 3-month randomized, prospective dietary intervention clinical trial are pending.[28] In addition, recent research indicates that mild to moderate calorie restriction or time-restricted feeding [29] slow the progression of autosomal dominant polycystic kidney disease (ADPKD) in mice[30]
[31]
Patient communities have been combining both ketogenic diets
That will either be some form of dialysis, which can be done at least two different ways at varying frequencies and durations (whether it is done at home or in the clinic depends on the method used and the patient's stability and training) and eventually, if they are eligible because of the nature and severity of their condition and if a suitable match can be found, unilateral or bilateral kidney transplantation.[35]
A Cochrane Review study of autosomal dominant polycystic kidney disease made note of the fact that it is important at all times, while avoiding
Prognosis
ADPKD individuals might have a normal life; conversely, ARPKD can cause kidney dysfunction and can lead to kidney failure by the age of 40–60. ADPKD1 and ADPKD2 are very different, in that ADPKD2 is much milder.[36]
Currently, there are no therapies proven effective to prevent the progression of ADPKD.[37]
Epidemiology
PKD is one of the most common hereditary diseases in the United States, affecting more than 600,000 people. It is the cause of nearly 10% of all end-stage renal disease. It equally affects men, women, and all races.[38] PKD occurs in some animals as well as humans.[39][40]
See also
References
- ^ a b c d e "Polycystic kidney disease". MedlinePlus Medical Encyclopedia. Retrieved 2015-07-30.
- ^ "Autosomal Dominant Polycystic Kidney Disease". National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Retrieved 3 January 2018.
- ^ "Autosomal Recessive Polycystic Kidney Disease". National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Retrieved 3 January 2018.
- ^ "What Is Polycystic Kidney Disease?". National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Retrieved 3 January 2018.
- PMID 20382325.
- PMID 1767134.
- ^ "polycystic kidney disease" at Dorland's Medical Dictionary
- PMID 26088074.
- ^ "Polycystic Kidney Disease". www.niddk.nih.gov. Archived from the original on 2017-01-04. Retrieved 2015-07-31.
- ISBN 9781582557243.
- ^ PMID 25490692.
- ^ S2CID 12417947.
- ^ S2CID 1700992.
- ^ PMID 16816842.
- PMID 27259053.
- PMID 16449663.
- S2CID 22331271.
- PMID 1980516.
- PMID 8307555.
- S2CID 28192819.
- ^ PMID 21694932.
- ISBN 9780323242875.
- ^ "Polycystic Kidney Disease". National Kidney Foundation. 2016-01-07. Retrieved 2022-11-17.
- ISSN 1555-905X.
- PMID 35570988.
- PMID 31631001.
- PMID 35664270.
- ^ Müller R (2022-08-23). "Ketogenic Dietary Interventions in Autosomal Dominant Polycystic Kidney Disease (ADPKD)". University of Cologne.
- PMID 32086281.
- PMID 26538633.
- PMID 26764208.
- ^ Spencer S (2021-12-25). "6 Ways People with PKD Can Lower Their Blood Pressure". Medium. Retrieved 2022-10-24.
- PMID 31361604.
- ^ "Breakthrough Results After 7 Years of Reversing Pkd". 2022-10-20. Retrieved 2022-10-24.
- ^ S2CID 70649130.
- ^ Torra R (2018-07-20). Talavera F, Aronoff GR (eds.). "Polycystic Kidney Disease: Practice Essentials, Background, Pathophysiology". Medscape.
- PMID 26171904.
- ISBN 978-0-8036-2505-1.
- ^ "Polycystic kidney disease (PKD): Gene test and negative register". International Cat Care. Archived from the original on 17 November 2016. Retrieved 2 November 2014.
- ^ "PKD - Polycystic Kidney Disease - British Shorthair". Antagene. Archived from the original on 17 August 2018. Retrieved 2 November 2014.
Further reading
- Chapin HC, Caplan MJ (November 2010). "The cell biology of polycystic kidney disease". The Journal of Cell Biology. 191 (4): 701–710. PMID 21079243.
- Harris PC, Torres VE (2009-01-01). "Polycystic kidney disease". Annual Review of Medicine. 60: 321–337. PMID 18947299.
- Halvorson CR, Bremmer MS, Jacobs SC (2010). "Polycystic kidney disease: inheritance, pathophysiology, prognosis, and treatment". International Journal of Nephrology and Renovascular Disease. 3: 69–83. PMID 21694932.
