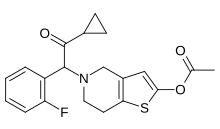
Prasugrel
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Effient, Efient |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a609027 |
| License data | |
| Pregnancy category |
|
| Routes of administration | By mouth |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | ≥79% |
| Protein binding | Active metabolite: ~98% |
| Elimination half-life | ~7 h (range 2 h to 15 h) |
| Excretion | Urine (~68% inactive metabolites); feces (27% inactive metabolites) |
| Identifiers | |
| |
JSmol) | |
| |
| |
| | |
Prasugrel, sold under the brand name Effient in the US, Australia and India, and Efient in the EU) is a medication used to prevent
Prasugrel was approved for use in the European Union in February 2009,[1] and in the US in July 2009, for the reduction of thrombotic cardiovascular events (including stent thrombosis) in people with acute coronary syndrome (ACS) who are to be managed with percutaneous coronary intervention (PCI).[2]
Medical uses
Prasugrel is used in combination with
Prasugrel does not change the risk of death when given to people who have had a STEMI[citation needed] or NSTEMI.
Given the risk of bleeding, prasugrel should not be used in people who are older than 75 years, who have low body weight or a history of transient ischemic attacks or strokes.[3][4] The initiation of prasugrel before coronary angiography outside the context of primary PCI is not recommended.[5][6][4]
Approval status
The drug was introduced to clinical practice in Canada in 2010 [7] but was subsequently withdrawn by the manufacturer in 2020 as a "business decision". This has left a gap in the management of high-risk patients in certain situations in Canada where Effient was the drug of choice.[8]
Contraindications
Prasugrel should not be given to people with active pathological bleeding, such as peptic ulcer or a history of transient ischemic attack or stroke, because of higher risk of stroke (thrombotic stroke and intracranial hemorrhage).[9]
Adverse effects
Adverse effects include:[10]
- Cardiovascular: Hypertension (8%), hypotension (4%), atrial fibrillation (3%), bradycardia (3%), noncardiac chest pain (3%), peripheral edema (3%), thrombotic thrombocytopenic purpura (TTP)
- Central nervous system: Headache (6%), dizziness (4%), fatigue (4%), fever (3%), extremity pain (3%)
- Dermatologic: Rash (3%)
- Endocrine and metabolic: Hypercholesterolemia/hyperlipidemia (7%)
- Gastrointestinal: Nausea (5%), diarrhea (2%), gastrointestinal hemorrhage (2%)
- Hematologic: Leukopenia (3%), anemia (2%)
- Neuromuscular and skeletal: Back pain (5%)
- Respiratory: Epistaxis (6%), dyspnea (5%), cough (4%)
- Hypersensitivity, including angioedema
Interactions
Prasugrel has a low potential for interactions. It may, for example, be used with
Pharmacology
Mechanism of action
Prasugrel is a member of the
[15][16] The TRITON-TIMI 38 study compared prasugrel with clopidogrel, and showed that prasugrel reduced rates of ischaemic events, but increased bleeding risk. Overall mortality rates were similar for each drug.[17]
Clopidogrel, unlike prasugrel, was issued a
Pharmacodynamics
Prasugrel produces inhibition of
Pharmacokinetics

Prasugrel is a
Chemistry
Prasugrel has one
References
- ^ "European Public Assessment Report for Efient" (PDF). EMA. 2009.
- S2CID 37160513.
- ^ PMID 17982182.
- ^ S2CID 13014429.
- PMID 25954988.
- S2CID 205095981.
- ^ "Product information -Effient". Health Canada. 2021. Retrieved February 18, 2021.
- PMID 34169260.
- ^ "Effient (prasugrel hydrochloride) Prescribing Information". U.S. Food and Drug Administration (FDA). September 2011. Archived from the original on 2017-01-18. Retrieved 2019-12-16.
- ^ a b "Efient (prasugrel) tablets: Highlights of prescribing information" (PDF). Eli Lilly. 2011. Archived from the original (PDF) on 31 January 2012.
- PMID 22570398.
- PMID 30510515.
- S2CID 205956050.
- PMID 27143321.
- PMID 17174640.
- S2CID 8226182.
- PMID 17982182.
- ^ "FDA Announces New Boxed Warning on Plavix: Alerts patients, health care professionals to potential for reduced effectiveness" (Press release). U.S. Food and Drug Administration (FDA). March 12, 2010. Archived from the original on March 15, 2010. Retrieved March 13, 2010.
- ^ "FDA Drug Safety Communication: Reduced effectiveness of Plavix (clopidogrel) in patients who are poor metabolizers of the drug". U.S. Food and Drug Administration (FDA). March 12, 2010. Retrieved March 13, 2010.
- PMID 21093072.
- PMID 17982182.
- S2CID 20617890.
- PMID 31198410.
- ^ O'Riordan M. "Switching from clopidogrel to prasugrel further reduces platelet function". TheHeart.org. Retrieved 1 April 2011.
- S2CID 1698598.
- PMID 26718653.
Further reading
- Dean L (2017). "Prasugrel Therapy and CYP Genotype". In Pratt VM, McLeod HL, Rubinstein WS, et al. (eds.). Medical Genetics Summaries. PMID 28520385. Bookshelf ID: NBK425796.
External links
- "Prasugrel". Drug Information Portal. U.S. National Library of Medicine.
- US 5288726 claims prasugrel compound; expired on 14 April 2017
- US 6693115 claims hydrochloride salt of prasugrel; will expire on 3 July 2021
