Psychiatry
 | |
| Occupation | |
|---|---|
| Names | Physician |
Activity sectors | Medicine |
| Description | |
Education required |
|
Related jobs |
|
Psychiatry is the medical specialty devoted to the diagnosis, prevention, and treatment of deleterious mental conditions.[1][2] These include various matters related to mood, behaviour, cognition, perceptions, and emotions.
Initial psychiatric assessment of a person begins with creating a
Treatment may include
Etymology

The term psychiatry was first coined by the German physician Johann Christian Reil in 1808 and literally means the 'medical treatment of the soul' (psych- 'soul' from Ancient Greek psykhē 'soul'; -iatry 'medical treatment' from Gk. iātrikos 'medical' from iāsthai 'to heal'). A medical doctor specializing in psychiatry is a psychiatrist (for a historical overview, see: Timeline of psychiatry).
Theory and focus
"Psychiatry, more than any other branch of medicine, forces its practitioners to wrestle with the nature of evidence, the validity of introspection, problems in communication, and other long-standing philosophical issues" (Guze, 1992, p.4).
Psychiatry refers to a field of medicine focused specifically on the mind, aiming to study, prevent, and treat mental disorders in humans.[10][11][12] It has been described as an intermediary between the world from a social context and the world from the perspective of those who are mentally ill.[13]
People who specialize in psychiatry often differ from most other mental health professionals and physicians in that they must be familiar with both the social and biological sciences.[11] The discipline studies the operations of different organs and body systems as classified by the patient's subjective experiences and the objective physiology of the patient. [14] Psychiatry treats mental disorders, which are conventionally divided into three general categories: mental illnesses, severe learning disabilities, and personality disorders.[15] Although the focus of psychiatry has changed little over time, the diagnostic and treatment processes have evolved dramatically and continue to do so. Since the late 20th century, the field of psychiatry has continued to become more biological and less conceptually isolated from other medical fields.[16]
Scope of practice
Though the medical specialty of psychiatry uses research in the field of neuroscience, psychology, medicine, biology, biochemistry, and pharmacology,[17] it has generally been considered a middle ground between neurology and psychology.[18] Because psychiatry and neurology are deeply intertwined medical specialties, all certification for both specialties and for their subspecialties is offered by a single board, the American Board of Psychiatry and Neurology, one of the member boards of the American Board of Medical Specialties.[19] Unlike other physicians and neurologists, psychiatrists specialize in the doctor–patient relationship and are trained to varying extents in the use of psychotherapy and other therapeutic communication techniques.[18] Psychiatrists also differ from psychologists in that they are physicians and have post-graduate training called residency (usually four to five years) in psychiatry; the quality and thoroughness of their graduate medical training is identical to that of all other physicians.[20] Psychiatrists can therefore counsel patients, prescribe medication, order laboratory tests, order neuroimaging, and conduct physical examinations.[3]
Ethics
The World Psychiatric Association issues an ethical code to govern the conduct of psychiatrists (like other purveyors of professional ethics). The psychiatric code of ethics, first set forth through the Declaration of Hawaii in 1977 has been expanded through a 1983 Vienna update and in the broader Madrid Declaration in 1996. The code was further revised during the organization's general assemblies in 1999, 2002, 2005, and 2011.[21]
The World Psychiatric Association code covers such matters as confidentiality, the death penalty, ethnic or cultural discrimination,[21] euthanasia, genetics, the human dignity of incapacitated patients, media relations, organ transplantation, patient assessment, research ethics, sex selection,[22] torture,[23][24] and up-to-date knowledge.
In establishing such ethical codes, the profession has responded to a number of controversies about the practice of psychiatry, for example, surrounding the use of lobotomy and electroconvulsive therapy.
Discredited psychiatrists who operated outside the norms of medical ethics include Harry Bailey, Donald Ewen Cameron, Samuel A. Cartwright, Henry Cotton, and Andrei Snezhnevsky.[25][page needed]
Approaches
Psychiatric illnesses can be conceptualised in a number of different ways. The
Once a medical professional diagnoses a patient there are numerous ways that they could choose to treat the patient. Often psychiatrists will develop a treatment strategy that incorporates different facets of different approaches into one. Drug prescriptions are very commonly written to be regimented to patients along with any therapy they receive. There are three major pillars of psychotherapy that treatment strategies are most regularly drawn from. Humanistic psychology attempts to put the "whole" of the patient in perspective; it also focuses on self exploration.[30] Behaviorism is a therapeutic school of thought that elects to focus solely on real and observable events, rather than mining the unconscious or subconscious. Psychoanalysis, on the other hand, concentrates its dealings on early childhood, irrational drives, the unconscious, and conflict between conscious and unconscious streams.[31]
Practitioners
This section relies largely or entirely upon a single source. (August 2017) ) |
All
As a career choice in the US
Psychiatry was not a popular career choice among medical students, even though medical school placements are rated favorably.
Subspecialties
The field of psychiatry has many subspecialties that require additional training and certification by the American Board of Psychiatry and Neurology (ABPN). Such subspecialties include:[36]
- Addiction psychiatry, addiction medicine
- Brain injury medicine[37][38]
- Child and adolescent psychiatry
- Clinical neurophysiology
- Consultation-liaison psychiatry[39]
- Forensic psychiatry
- Geriatric psychiatry
- Hospice and palliative medicine
- Sleep medicine[40]
Additional psychiatry subspecialties, for which the ABPN does not provide formal certification, include:[41]
- Biological psychiatry
- Cognitive diseases, as in various forms of dementia
- Community psychiatry
- Cross-cultural psychiatry
- Emergency psychiatry
- Evolutionary psychiatry
- Global mental health
- Learning disabilities
- Military psychiatry
- Neurodevelopmental disorders
- Neuropsychiatry
- Social psychiatry
In larger healthcare organizations, psychiatrists often serve in senior management roles, where they are responsible for the efficient and effective delivery of mental health services for the organization's constituents. For example, the Chief of Mental Health Services at most VA medical centers is usually a psychiatrist, although psychologists occasionally are selected for the position as well.[citation needed]
In the United States, psychiatry is one of the few specialties which qualify for further education and board-certification in pain medicine, palliative medicine, and sleep medicine.
Research
Psychiatric research is, by its very nature, interdisciplinary; combining social, biological and psychological perspectives in attempt to understand the nature and treatment of mental disorders.[48] Clinical and research psychiatrists study basic and clinical psychiatric topics at research institutions and publish articles in journals.[17][49][50][51] Under the supervision of institutional review boards, psychiatric clinical researchers look at topics such as neuroimaging, genetics, and psychopharmacology in order to enhance diagnostic validity and reliability, to discover new treatment methods, and to classify new mental disorders.[52][page needed]
Clinical application
Diagnostic systems
Potential use of MRI/fMRI in diagnosis
In 2018, the
- "have a sensitivity of at least 80% for detecting a particular psychiatric disorder"
- "should have a specificity of at least 80% for distinguishing this disorder from other psychiatric or medical disorders"
- "should be reliable, reproducible, and ideally be noninvasive, simple to perform, and inexpensive"
- "proposed biomarkers should be verified by 2 independent studies each by a different investigator and different population samples and published in a peer-reviewed journal"
The review concluded that although neuroimaging diagnosis may technically be feasible, very large studies are needed to evaluate specific biomarkers which were not available.[63]
Diagnostic manuals
Three main diagnostic manuals used to classify mental health conditions are in use today. The ICD-11 is produced and published by the World Health Organization, includes a section on psychiatric conditions, and is used worldwide.[64] The Diagnostic and Statistical Manual of Mental Disorders, produced and published by the American Psychiatric Association (APA), is primarily focused on mental health conditions and is the main classification tool in the United States.[65] It is currently in its fifth revised edition and is also used worldwide.[65] The Chinese Society of Psychiatry has also produced a diagnostic manual, the Chinese Classification of Mental Disorders.[66]
The stated intention of diagnostic manuals is typically to develop replicable and clinically useful categories and criteria, to facilitate consensus and agreed upon standards, whilst being atheoretical as regards etiology.[65][67] However, the categories are nevertheless based on particular psychiatric theories and data; they are broad and often specified by numerous possible combinations of symptoms, and many of the categories overlap in symptomology or typically occur together.[68] While originally intended only as a guide for experienced clinicians trained in its use, the nomenclature is now widely used by clinicians, administrators and insurance companies in many countries.[69]
The DSM has attracted praise for standardizing psychiatric diagnostic categories and criteria. It has also attracted controversy and criticism. Some critics argue that the DSM represents an
Treatment
General considerations

Individuals receiving psychiatric treatment are commonly referred to as
A psychiatrist or medical provider evaluates people through a psychiatric assessment for their mental and physical condition. This usually involves interviewing the person and often obtaining information from other sources such as other health and social care professionals, relatives, associates, law enforcement personnel, emergency medical personnel, and psychiatric rating scales. A mental status examination is carried out, and a physical examination is usually performed to establish or exclude other illnesses that may be contributing to the alleged psychiatric problems. A physical examination may also serve to identify any signs of self-harm; this examination is often performed by someone other than the psychiatrist, especially if blood tests and medical imaging are performed.
Like most medications, psychiatric medications can cause
Inpatient treatment
This section needs additional citations for verification. (August 2017) |
Average inpatient psychiatric treatment stay has decreased significantly since the 1960s, a trend known as
Psychiatric inpatients are people admitted to a hospital or clinic to receive psychiatric care. Some are admitted involuntarily, perhaps committed to a secure hospital, or in some jurisdictions to a facility within the prison system. In many countries including the United States and Canada, the criteria for involuntary admission vary with local jurisdiction. They may be as broad as having a mental health condition, or as narrow as being an immediate danger to themselves or others. Bed availability is often the real determinant of admission decisions to hard pressed public facilities.
People may be admitted voluntarily if the treating doctor considers that safety is not compromised by this less restrictive option. For many years, controversy has surrounded the use of involuntary treatment and use of the term "lack of insight" in describing patients. Internationally, mental health laws vary significantly but in many cases, involuntary psychiatric treatment is permitted when there is deemed to be a significant risk to the patient or others due to the patient's illness. Involuntary treatment refers to treatment that occurs based on a treating physician's recommendations, without requiring consent from the patient.[83]
Inpatient psychiatric wards may be secure (for those thought to have a particular risk of violence or self-harm) or unlocked/open. Some wards are mixed-sex whilst same-sex wards are increasingly favored to protect women inpatients. Once in the care of a hospital, people are
In many developed countries there has been a massive reduction in psychiatric beds since the mid 20th century, with the growth of community care. Standards of inpatient care remain a challenge in some public and private facilities, due to levels of funding, and facilities in developing countries are typically grossly inadequate for the same reason. Even in developed countries, programs in public hospitals vary widely. Some may offer structured activities and therapies offered from many perspectives while others may only have the funding for medicating and monitoring patients. This may be problematic in that the maximum amount of therapeutic work might not actually take place in the hospital setting. This is why hospitals are increasingly used in limited situations and moments of crisis where patients are a direct threat to themselves or others. Alternatives to psychiatric hospitals that may actively offer more therapeutic approaches include rehabilitation centers or "rehab" as popularly termed.[citation needed]
Outpatient treatment
Outpatient treatment involves periodic visits to a psychiatrist for consultation in his or her office, or at a community-based outpatient clinic. During initial appointments, a psychiatrist generally conducts a psychiatric assessment or evaluation of the patient. Follow-up appointments then focus on making medication adjustments, reviewing potential medication interactions, considering the impact of other medical disorders on the patient's mental and emotional functioning, and counseling patients regarding changes they might make to facilitate healing and remission of symptoms. The frequency with which a psychiatrist sees people in treatment varies widely, from once a week to twice a year, depending on the type, severity and stability of each person's condition, and depending on what the clinician and patient decide would be best.
Increasingly, psychiatrists are limiting their practices to psychopharmacology (prescribing medications), as opposed to previous practice in which a psychiatrist would provide traditional 50-minute psychotherapy sessions, of which psychopharmacology would be a part, but most of the consultation sessions consisted of "talk therapy". This shift began in the early 1980s and accelerated in the 1990s and 2000s.[85] A major reason for this change was the advent of managed care insurance plans,[clarification needed] which began to limit reimbursement for psychotherapy sessions provided by psychiatrists. The underlying assumption was that psychopharmacology was at least as effective as psychotherapy, and it could be delivered more efficiently because less time is required for the appointment.[86][87][88][89][90][91][a][excessive citations] Because of this shift in practice patterns, psychiatrists often refer patients whom they think would benefit from psychotherapy to other mental health professionals, e.g., clinical social workers and psychologists.[92]
Telepsychiatry

Telepsychiatry or telemental health refers to the use of telecommunications technology (mostly videoconferencing and phone calls) to deliver psychiatric care remotely for people with mental health conditions. It is a branch of telemedicine.[93][94]
Telepsychiatry can be effective in treating people with mental health conditions. In the short-term it can be as acceptable and effective as face-to-face care.[95]
It can improve access to mental health services for some but might also represent a barrier for those lacking access to a suitable device, the internet or the necessary digital skills. Factors such as poverty that are associated with lack of internet access are also associated with greater risk of mental health problems, making digital exclusion an important problem of telemental health services.[95]
During the COVID-19 pandemic mental health services were adapted to telemental health in high-income countries. It proved effective and acceptable for use in an emergency situation but there were concerns regarding its long-term implementation.[96]History
Earliest knowledge
The earliest known texts on mental disorders are from ancient India and include the Ayurvedic text, Charaka Samhita.[97][98] The first hospitals for curing mental illness were established in India during the 3rd century BCE.[99]
Greek philosophers, including
In the 6th century AD,
The
The first bimaristan was founded in Baghdad in the 9th century, and several others of increasing complexity were created throughout the Arab world in the following centuries. Some of the bimaristans contained wards dedicated to the care of mentally ill patients.[106] During the Middle Ages, Psychiatric hospitals and lunatic asylums were built and expanded throughout Europe. Specialist hospitals such as Bethlem Royal Hospital in London were built in medieval Europe from the 13th century to treat mental disorders, but were used only as custodial institutions and did not provide any type of treatment. It is the oldest extant psychiatric hospital in the world.[107]
An ancient text known as
Medical specialty
The beginning of psychiatry as a medical specialty is dated to the middle of the nineteenth century,
During the Enlightenment, attitudes towards the mentally ill began to change. It came to be viewed as a disorder that required compassionate treatment. In 1758, English physician William Battie wrote his Treatise on Madness on the management of mental disorder. It was a critique aimed particularly at the Bethlem Royal Hospital, where a conservative regime continued to use barbaric custodial treatment. Battie argued for a tailored management of patients entailing cleanliness, good food, fresh air, and distraction from friends and family. He argued that mental disorder originated from dysfunction of the material brain and body rather than the internal workings of the mind.[111][112]

The introduction of moral treatment was initiated independently by the French doctor
Although Tuke, Pinel and others had tried to do away with physical restraint, it remained widespread into the 19th century. At the Lincoln Asylum in England, Robert Gardiner Hill, with the support of Edward Parker Charlesworth, pioneered a mode of treatment that suited "all types" of patients, so that mechanical restraints and coercion could be dispensed with—a situation he finally achieved in 1838. In 1839, Sergeant John Adams and Dr. John Conolly were impressed by the work of Hill, and introduced the method into their Hanwell Asylum, by then the largest in the country.[114][115][page needed]
The modern era of institutionalized provision for the care of the mentally ill, began in the early 19th century with a large state-led effort. In England, the
At the turn of the century, England and France combined had only a few hundred individuals in asylums.[118] By the late 1890s and early 1900s, this number had risen to the hundreds of thousands. However, the idea that mental illness could be ameliorated through institutionalization ran into difficulties.[119] Psychiatrists were pressured by an ever-increasing patient population,[119] and asylums again became almost indistinguishable from custodial institutions.[120]
In the early 1800s, psychiatry made advances in the diagnosis of mental illness by broadening the category of mental disease to include mood disorders, in addition to disease level delusion or irrationality.[121] The 20th century introduced a new psychiatry into the world, with different perspectives of looking at mental disorders. For Emil Kraepelin, the initial ideas behind biological psychiatry, stating that the different mental disorders are all biological in nature, evolved into a new concept of "nerves", and psychiatry became a rough approximation of neurology and neuropsychiatry.[122] Following Sigmund Freud's pioneering work, ideas stemming from psychoanalytic theory also began to take root in psychiatry.[123] The psychoanalytic theory became popular among psychiatrists because it allowed the patients to be treated in private practices instead of warehoused in asylums.[123]
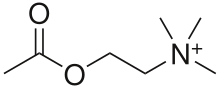
By the 1970s, however, the psychoanalytic school of thought became marginalized within the field.[123] Biological psychiatry reemerged during this time. Psychopharmacology and neurochemistry became the integral parts of psychiatry starting with Otto Loewi's discovery of the neuromodulatory properties of acetylcholine; thus identifying it as the first-known neurotransmitter. Subsequently, it has been shown that different neurotransmitters have different and multiple functions in regulation of behaviour. In a wide range of studies in neurochemistry using human and animal samples, individual differences in neurotransmitters' production, reuptake, receptors' density and locations were linked to differences in dispositions for specific psychiatric disorders. For example, the discovery of chlorpromazine's effectiveness in treating schizophrenia in 1952 revolutionized treatment of the disorder,[124] as did lithium carbonate's ability to stabilize mood highs and lows in bipolar disorder in 1948.[125] Psychotherapy was still utilized, but as a treatment for psychosocial issues.[126] This proved the idea of neurochemical nature of many psychiatric disorders.
Another approach to look for biomarkers of psychiatric disorders is [127] Neuroimaging that was first utilized as a tool for psychiatry in the 1980s.[128]
In 1963, US president John F. Kennedy introduced legislation delegating the National Institute of Mental Health to administer Community Mental Health Centers for those being discharged from state psychiatric hospitals.[129] Later, though, the Community Mental Health Centers focus shifted to providing psychotherapy for those with acute but less serious mental disorders.[129] Ultimately there were no arrangements made for actively following and treating severely mentally ill patients who were being discharged from hospitals, resulting in a large population of chronically homeless people with mental illness.[129]
Controversy and criticism
The institution of psychiatry has attracted controversy since its inception.
Double argues that most critical psychiatry is anti-reductionist. Rashed argues new mental health science has moved beyond this reductionist critique by seeking integrative and biopsychosocial models for conditions and that much of critical psychiatry now exists with orthodox psychiatry but notes that many critiques remain unaddressed[131]: 237
The term
See also
Notes
- ^ This article does not enter into that debate or seek to summarize the comparative efficacy literature. It simply explains why managed care insurance companies stopped routinely reimbursing psychiatrists for traditional psychotherapy, without commenting on the validity of that rationale.
References
Citations
- ^ Alarcón RD (2016). "Psychiatry and Its Dichotomies". Psychiatric Times. 33 (5): 1. Archived from the original on 2019-01-30. Retrieved 2016-07-26.
- ^ a b "Information about Mental Illness and the Brain (Page 3 of 3)". The Science of Mental Illness. National Institute of Mental Health. January 31, 2006. Archived from the original on 12 October 2007. Retrieved April 19, 2007.
- PMID 29856559.
- PMID 20483976.
- S2CID 25268111.
- ^ "Psychiatry Specialty Description". American Medical Association. Archived from the original on 12 October 2020. Retrieved 10 October 2020.
- ^ Rabuzzi M (November 1997). "Butterfly Etymology". Cultural Entomology Digest. No. 4. Archived from the original on 3 December 1998.
- .
- ^ Guze 1992, p. 4.
- ^ OCLC 599349242.
- ^ Lyness 1997, p. 3.
- ^ Gask 2004, p. 7.
- ^ Guze 1992, p. 131.
- ^ Gask 2004, p. 113.
- ^ Gask 2004, p. 128.
- ^ PMID 14594732.
- ^ a b Shorter 1997, p. 326.
- ^ "Specialty and Subspecialty Certificates", American Board of Medical Specialties, n.d., archived from the original on 23 January 2020, retrieved 27 July 2016
- ^ Hauser MJ. "Student Information". Psychiatry.com. Archived from the original on 23 October 2010. Retrieved 21 September 2007.
- ^ a b "Madrid Declaration on Ethical Standards for Psychiatric Practice". World Psychiatric Association. 21 September 2011. Archived from the original on 4 March 2016. Retrieved 3 November 2014.
- S2CID 39675837.
These practices, in which racial hygiene constituted one of the fundamental principles and euthanasia programmes were the most obvious consequence, violated the majority of known bioethical principles. Psychiatry played a central role in these programmes, and the mentally ill were the principal victims.
- PMID 1795363.
Based on the generally accepted definition, we correctly term the utilisation of psychiatry for the punishment of political dissidents as torture.
- from the original on 2015-09-10. Retrieved 2007-10-04.
Over the past two decades the systematic use of torture and psychiatric abuse have been sanctioned or condoned by more than one-third of the nations in the United Nations, about half of mankind.
- OCLC 935892629.
- PMID 7627683.
- ^ S2CID 12321002.
- ^ ISBN 978-1-932690-39-2.[page needed]
- ^ ISBN 978-1-61599-011-5.[page needed]
- ^ Michael H. "Humanistic Therapy". CRC Health Group. Archived from the original on 2 June 2019. Retrieved 29 March 2015.
- ^ McLeod S (2014). "Psychoanalysis". Simply Psychology. Archived from the original on 19 April 2015. Retrieved 29 March 2015.
- ^ S2CID 13274934.
- ^ Japsen B (15 September 2015). "Psychiatrist Shortage Worsens Amid 'Mental Health Crisis'". Forbes. Archived from the original on 9 September 2017. Retrieved 8 September 2017.
- PMID 25764147.
- .
- ^ "Taking a Subspecialty Exam". American Board of Psychiatry and Neurology. Archived from the original on 2015-09-05. Retrieved 2015-09-19.
- ^ "Brain Injury Medicine". American Board of Psychiatry and Neurology. Archived from the original on 2017-08-20. Retrieved 2017-08-20.
- .
- ^ "Psychosomatic Medicine". American Board of Psychiatry and Neurology. Archived from the original on 2017-08-20. Retrieved 2017-08-20.
- ^ "Sleep Medicine". American Board of Psychiatry and Neurology. Archived from the original on 2017-08-20. Retrieved 2017-08-20.
- ^ "Careers info for School leavers". The Royal College of Psychiatrists. 2005. Archived from the original on 9 July 2007. Retrieved March 25, 2007.
- ^ "About AACP". American Association of Community Psychiatrists. University of Pittsburgh School of Medicine, Department of Psychiatry. Archived from the original on 6 September 2009. Retrieved August 5, 2008.
- PMID 20483977.
- )
- )
- OCLC 455800587.
- )
- ^ "Research in Psychiatry". University of Manchester. Archived from the original on 23 December 2007. Retrieved 13 October 2007.
- ^ "New York State Psychiatric Institute". 15 March 2007. Archived from the original on 5 November 2020. Retrieved 13 October 2007.
- ^ "Canadian Psychiatric Research Foundation". 27 July 2007. Archived from the original on 10 October 2007. Retrieved 13 October 2007.
- ^ "Journal of Psychiatric Research". Elsevier. 8 October 2007. Archived from the original on 30 September 2020. Retrieved 13 October 2007.
- OCLC 632834662.
- PMID 7414302.
- OCLC 869194520.
- ^ Lyness 1997, p. 10.
- S2CID 35203096.
- S2CID 147489857.
- ^ "Neuroimaging and Mental Illness: A Window Into the Brain". National Institute of Mental Health. U.S. Department of Health and Human Services. 2009. Archived from the original on 1 June 2013.
- S2CID 44658585.
- PMID 17207536.
- S2CID 23676927.
- PMID 32128436.
- PMID 30173550.
- ^ "ICD-11". icd.who.int. Retrieved 2024-01-24.
- ^ ISBN 978-0-89042-025-6.
- S2CID 24080102.
- S2CID 145140298.
- S2CID 44798734.
- S2CID 26516651.
- PMID 20048461.

- PMID 12505793.
- PMID 17329740.
- PMID 9862559.
- PMID 14974002.
- PMID 11087016.
- ^ Lutterman, Ted; Shaw, Robert; Fisher, William; Manderscheid, Ronald (2017). Trend in Psychiatric Inpatient Capacity, United States and Each State, 1970 to 2014 (PDF) (Report). Alexandria, VA: National Association of State Mental Health Program Directors. Archived (PDF) from the original on 2022-09-01.
- (PDF) from the original on 2022-09-04. Retrieved 2019-09-05.
- PMID 9736004.
- PMID 22751995.
- ^ "Number of patients physically restrained at psychiatric hospitals soars". The Japan Times Online. 2016-05-09. Archived from the original on 2023-03-11. Retrieved 2018-01-04.
- ^ 長谷川利夫. (2016). 精神科医療における隔離・ 身体拘束実態調査 ~その急増の背景要因を探り縮減への道筋を考える~. 病院・地域精神医学, 59(1), 18–21.
- ^ Unzicker R, Wolters KP, Robinson DE (20 January 2000). "From Privileges to Rights: People Labeled with Psychiatric Disabilities Speak for Themselves". National Council on Disability. Archived from the original on 28 December 2010.
- OCLC 223935527.
- PMID 18678801.
- PMID 20511735.
- PMID 16548751.
- S2CID 21269419.
- S2CID 40179147.
- PMID 20048220.
- PMID 11779262.
- ^ Harris G (March 5, 2011). "Talk Doesn't Pay, So Psychiatry Turns to Drug Therapy". The New York Times. Archived from the original on September 4, 2011. Retrieved March 6, 2011.
- ^ "What is Telepsychiatry?". American Psychiatric Association. Retrieved 2023-02-20.
- ^ "What is Telemental Health?". National Institute of Mental Health (NIMH). Retrieved 2023-02-20.
- ^ PMID 35767691.
- PMID 34709179.
- OCLC 955106253.
- OCLC 916942828.
- OCLC 476009436.
- OL 3149647W.
- ^ OCLC 4687317.
- OCLC 761231096.
- S2CID 235334263.
- ^ S2CID 235334263.
- ^ a b Mohamed WM (August 2008). "History of Neuroscience: Arab and Muslim Contributions to Modern Neuroscience" (PDF). International Brain Research Organization. Archived from the original (PDF) on 10 June 2014.
- PMID 17139063.
- ^ Shorter 1997, p. 4.
- ^ Shorter 1997, p. 1.
- ^ "The Bethel Hospital". Norwich HEART: Heritage Economic & Regeneration Trust. Archived from the original on 13 November 2011.
- ^ Shorter 1997, p. 5.
- S2CID 13162025.
- ^ Shorter 1997, p. 9.
- ]
- PMID 7877402.
- OCLC 538062123.
- ^ Wright, David: "Mental Health Timeline", 1999
- ISBN 978-0-8166-4939-6– via Google Books.
- ^ Shorter 1997, p. 34.
- ^ a b Shorter 1997, p. 46.
- ISBN 978-0-316-75745-4.
- ^ Borch-Jacobsen M (7 October 2010). "Which came first, the condition or the drug?". London Review of Books. 32 (19): 31–33. Archived from the original on 13 March 2015. Retrieved 30 November 2012.
- ^ Shorter 1997, p. 114.
- ^ a b c Shorter 1997, p. 145.
- PMID 17204765.
- PMID 18142718.
- ^ Shorter 1997, p. 239.
- ^ Shorter 1997, p. 246.
- ^ Shorter 1997, p. 270.
- ^ a b c Shorter 1997, p. 280.
- ^ S2CID 149547063.
- PMID 32102717.
- ISBN 3-927408-82-4, page 87
- ^ "Citizens Commission on Human Rights Expands its Activities to Expose and Handle Psychiatric Abuse in Clearwater, Tampa Bay via New Center". Scientology. Archived from the original on 2018-03-11. Retrieved 2018-03-10.
Cited texts
- Gask L (2004). A Short Introduction to Psychiatry. London: SAGE Publications Ltd. OCLC 56009828.
- Guze SB (1992). Why Psychiatry Is a Branch of Medicine. New York: Oxford University Press. OCLC 25315637.
- Lyness JM (1997). Psychiatric Pearls. Philadelphia: F.A. Davis Company. OCLC 807453406.
- Shorter E (1998) [1997]. A History of Psychiatry: From the Era of the Asylum to the Age of Prozac. New York: John Wiley & Sons, Inc. OCLC 60169541.
Further reading
- Berrios GE, Porter R, eds. (1995). The History of Clinical Psychiatry. London: Athlone Press. OCLC 1000559759.
- Berrios GE (1996). History of Mental symptoms: The History of Descriptive Psychopathology since the 19th century. Cambridge: Cambridge University Press. OCLC 668203298.
- Ford-Martin PA (2002). "Psychosis". In Longe JL, Blanchfield DS (eds.). Gale Encyclopedia of Medicine. Vol. 4 (2nd ed.). Detroit: Gale Group. OCLC 51166617.
- Francis, Gavin, "Changing Psychiatry's Mind" (review of Anne Harrington, Mind Fixers: Psychiatry's Troubled Search for the Biology of Mental Illness, Norton, 366 pp.; and Nathan Filer, This Book Will Change Your Mind about Mental Health: A Journey into the Heartland of Psychiatry, London, Faber and Faber, 248 pp.), The New York Review of Books, vol. LXVIII, no. 1 (14 January 2021), pp. 26–29. "[M]ental disorders are different [from illnesses addressed by other medical specialties].... [T]o treat them as purely physical is to misunderstand their nature." "[C]are [needs to be] based on distress and [cognitive, emotional, and physical] need rather than [on psychiatric] diagnos[is]", which is often uncertain, erratic, and unreplicable. (p. 29.)
- Big Data technologies will make psychiatric signs and symptomsmore quantifiably objective. Sue Halpern cautions, however, that "When numbers have no agreed-upon, scientifically-derived, extrinsic meaning, quantification is unavailing." (p. 62.)
- Hirschfeld RM, Lewis L, Vornik LA (February 2003). "Perceptions and impact of bipolar disorder: how far have we really come? Results of the national depressive and manic-depressive association 2000 survey of individuals with bipolar disorder". The Journal of Clinical Psychiatry. 64 (2): 161–74. PMID 12633125.
- Krieke LV, Jeronimus BF, Blaauw FJ, Wanders RB, Emerencia AC, Schenk HM, Vos SD, Snippe E, Wichers M, Wigman JT, Bos EH, Wardenaar KJ, Jonge PD (June 2016). "HowNutsAreTheDutch (HoeGekIsNL): A crowdsourcing study of mental symptoms and strengths" (PDF). International Journal of Methods in Psychiatric Research. 25 (2): 123–44. PMID 26395198. Archived from the original(PDF) on 2019-08-02. Retrieved 2019-12-06.
- McGorry PD, Mihalopoulos C, Henry L, Dakis J, Jackson HJ, Flaum M, Harrigan S, McKenzie D, Kulkarni J, Karoly R (February 1995). "Spurious precision: procedural validity of diagnostic assessment in psychotic disorders". The American Journal of Psychiatry. 152 (2): 220–3. PMID 7840355.
- Moncrieff J, Cohen D (2005). "Rethinking models of psychotropic drug action". Psychotherapy and Psychosomatics. 74 (3): 145–53. S2CID 6917144.
- Burke C (February 2000). "Psychiatry: a "value-free" science?". from the original on 2021-11-29. Retrieved 2011-01-22.
- "What is Cognitive-Behavioral Therapy?". National Association of Cognitive-Behavioral Therapists. Archived from the original on 25 September 2006. Retrieved 20 September 2006.
- Van Os J, Gilvarry C, Bale R, Van Horn E, Tattan T, White I, Murray R (May 1999). "A comparison of the utility of dimensional and categorical representations of psychosis. UK700 Group". Psychological Medicine. 29 (3): 595–606. S2CID 38854519.
- Walker E, Young PD (1986). A Killing Cure (1st ed.). New York: H. Holt and Co. OCLC 12665467.
- Williams JB, Gibbon M, First MB, Spitzer RL, Davies M, Borus J, Howes MJ, Kane J, Pope HG, Rounsaville B (August 1992). "The Structured Clinical Interview for DSM-III-R (SCID). II. Multisite test-retest reliability". Archives of General Psychiatry. 49 (8): 630–6. PMID 1637253.
- Hiruta G (June 2002). Beveridge A (ed.). "Japanese psychiatry in the Edo period (1600-1868)". History of Psychiatry. 13 (50): 131–51. S2CID 143377079.
