Tuberculosis
| Tuberculosis | |
|---|---|
| Other names | Phthisis, phthisis pulmonalis, consumption, great white plague |
| Treatment | Antibiotics[1] |
| Frequency | 25% of people (latent TB)[6] |
| Deaths | 1.3 million (2022)[6] |
Tuberculosis (TB), also known colloquially as the "white death", or historically as consumption,
Tuberculosis is
Prevention of TB involves screening those at high risk, early detection and treatment of cases, and
In 2018, one quarter of the world's population was thought to have a latent infection of TB.[6] New infections occur in about 1% of the population each year.[11] In 2022, an estimated 10.6 million people developed active TB, resulting in 1.3 million deaths, making it the second leading cause of death from an infectious disease after COVID-19.[12] As of 2018, most TB cases occurred in the regions of South-East Asia (44%), Africa (24%), and the Western Pacific (18%), with more than 50% of cases being diagnosed in seven countries: India (27%), China (9%), Indonesia (8%), the Philippines (6%), Pakistan (6%), Nigeria (4%), and Bangladesh (4%).[13] By 2021, the number of new cases each year was decreasing by around 2% annually.[12][1] About 80% of people in many Asian and African countries test positive, while 5–10% of people in the United States test positive via the tuberculin test.[14] Tuberculosis has been present in humans since ancient times.[15]
History
Tuberculosis has existed since
Before the Industrial Revolution, folklore often associated tuberculosis with vampires. When one member of a family died from the disease, the other infected members would lose their health slowly. People believed this was caused by the original person with TB draining the life from the other family members.[21]
Identification
Although

Robert Koch identified and described the bacillus causing tuberculosis, M. tuberculosis, on 24 March 1882.[32][33] In 1905, he was awarded the Nobel Prize in Physiology or Medicine for this discovery.[34]
Development of treatments
In Europe, rates of tuberculosis began to rise in the early 1600s to a peak level in the 1800s, when it caused nearly 25% of all deaths.[35] In the 18th and 19th century, tuberculosis had become epidemic in Europe, showing a seasonal pattern.[36][37] Tuberculosis caused widespread public concern in the 19th and early 20th centuries as the disease became common among the urban poor. In 1815, one in four deaths in England was due to "consumption". By 1918, TB still caused one in six deaths in France.[citation needed] After TB was determined to be contagious, in the 1880s, it was put on a notifiable-disease list in Britain; campaigns started to stop people from spitting in public places, and the infected poor were "encouraged" to enter sanatoria that resembled prisons (the sanatoria for the middle and upper classes offered excellent care and constant medical attention).[29] Whatever the benefits of the "fresh air" and labor in the sanatoria, even under the best conditions, 50% of those who entered died within five years (c. 1916).[29]
Robert Koch did not believe the cattle and human tuberculosis diseases were similar, which delayed the recognition of infected milk as a source of infection. During the first half of the 1900s, the risk of transmission from this source was dramatically reduced after the application of the
Albert Calmette and Camille Guérin achieved the first genuine success in immunization against tuberculosis in 1906, using attenuated bovine-strain tuberculosis. It was called bacille Calmette–Guérin (BCG). The BCG vaccine was first used on humans in 1921 in France,[40] but achieved widespread acceptance in the US, Great Britain, and Germany only after World War II.[41]
By the 1950s mortality in Europe had decreased about 90%.[42] Improvements in sanitation, vaccination, and other public-health measures began significantly reducing rates of tuberculosis even before the arrival of streptomycin and other antibiotics, although the disease remained a significant threat.[42] In 1946, the development of the antibiotic streptomycin made effective treatment and cure of TB a reality. Prior to the introduction of this medication, the only treatment was surgical intervention, including the "pneumothorax technique", which involved collapsing an infected lung to "rest" it and to allow tuberculous lesions to heal.[43]
Current reemergence
Because of the emergence of
Signs and symptoms

Tuberculosis may infect any part of the body, but most commonly occurs in the lungs (known as pulmonary tuberculosis).[8] Extrapulmonary TB occurs when tuberculosis develops outside of the lungs, although extrapulmonary TB may coexist with pulmonary TB.[8]
General signs and symptoms include fever,
Pulmonary
If a tuberculosis infection does become active, it most commonly involves the lungs (in about 90% of cases).
Extrapulmonary
In 15–20% of active cases, the infection spreads outside the lungs, causing other kinds of TB.
Causes
Mycobacteria
The main cause of TB is Mycobacterium tuberculosis (MTB), a small, aerobic, nonmotile bacillus.[8] The high lipid content of this pathogen accounts for many of its unique clinical characteristics.[53] It divides every 16 to 20 hours, which is an extremely slow rate compared with other bacteria, which usually divide in less than an hour.[54] Mycobacteria have an outer membrane lipid bilayer.[55] If a Gram stain is performed, MTB either stains very weakly "Gram-positive" or does not retain dye as a result of the high lipid and mycolic acid content of its cell wall.[56] MTB can withstand weak disinfectants and survive in a dry state for weeks. In nature, the bacterium can grow only within the cells of a host organism, but M. tuberculosis can be cultured in the laboratory.[57]
Using
are also used.The
Other known pathogenic mycobacteria include M. leprae, M. avium, and M. kansasii. The latter two species are classified as "nontuberculous mycobacteria" (NTM) or atypical mycobacteria. NTM cause neither TB nor leprosy, but they do cause lung diseases that resemble TB.[69]

Transmission
When people with active pulmonary TB cough, sneeze, speak, sing, or spit, they expel infectious
Risk of transmission
People with prolonged, frequent, or close contact with people with TB are at particularly high risk of becoming infected, with an estimated 22% infection rate.
Risk factors
A number of factors make individuals more susceptible to TB infection and/or disease.[76]
Active disease risk
The most important risk factor globally for developing active TB is concurrent HIV infection; 13% of those with TB are also infected with HIV.[77] This is a particular problem in sub-Saharan Africa, where HIV infection rates are high.[78][79] Of those without HIV infection who are infected with tuberculosis, about 5–10% develop active disease during their lifetimes;[47] in contrast, 30% of those co-infected with HIV develop the active disease.[47]
Use of certain medications, such as
Other risk factors include:
).Infection susceptibility
Tobacco smoking increases the risk of infections (in addition to increasing the risk of active disease and death). Additional factors increasing infection susceptibility include young age.[76]
Pathogenesis

About 90% of those infected with M. tuberculosis have asymptomatic, latent TB infections (sometimes called LTBI),[86] with only a 10% lifetime chance that the latent infection will progress to overt, active tuberculous disease.[87] In those with HIV, the risk of developing active TB increases to nearly 10% a year.[87] If effective treatment is not given, the death rate for active TB cases is up to 66%.[73]
TB infection begins when the mycobacteria reach the
The primary site of infection in the lungs, known as the Ghon focus, is generally located in either the upper part of the lower lobe, or the lower part of the upper lobe.[14] Tuberculosis of the lungs may also occur via infection from the blood stream. This is known as a Simon focus and is typically found in the top of the lung.[90] This hematogenous transmission can also spread infection to more distant sites, such as peripheral lymph nodes, the kidneys, the brain, and the bones.[14][91] All parts of the body can be affected by the disease, though for unknown reasons it rarely affects the heart, skeletal muscles, pancreas, or thyroid.[92]
Tuberculosis is classified as one of the
If TB bacteria gain entry to the blood stream from an area of damaged tissue, they can spread throughout the body and set up many foci of infection, all appearing as tiny, white tubercles in the tissues.[95] This severe form of TB disease, most common in young children and those with HIV, is called miliary tuberculosis.[96] People with this disseminated TB have a high fatality rate even with treatment (about 30%).[52][97]
In many people, the infection waxes and wanes. Tissue destruction and necrosis are often balanced by healing and
Diagnosis
Active tuberculosis
Diagnosing active tuberculosis based only on signs and symptoms is difficult,
A definitive diagnosis of TB is made by identifying M. tuberculosis in a clinical sample (e.g., sputum, pus, or a tissue biopsy). However, the difficult culture process for this slow-growing organism can take two to six weeks for blood or sputum culture.[103] Thus, treatment is often begun before cultures are confirmed.[104]
Latent tuberculosis

The
The
Prevention

Tuberculosis prevention and control efforts rely primarily on the vaccination of infants and the detection and appropriate treatment of active cases.[15] The World Health Organization (WHO) has achieved some success with improved treatment regimens, and a small decrease in case numbers.[15] Some countries have legislation to involuntarily detain or examine those suspected to have tuberculosis, or involuntarily treat them if infected.[113]
Vaccines
The only available
It is the most widely used vaccine worldwide, with more than 90% of all children being vaccinated.[15] The immunity it induces decreases after about ten years.[15] As tuberculosis is uncommon in most of Canada, Western Europe, and the United States, BCG is administered to only those people at high risk.[117][118][119] Part of the reasoning against the use of the vaccine is that it makes the tuberculin skin test falsely positive, reducing the test's usefulness as a screening tool.[119] Several vaccines are being developed.[15]
Intradermal MVA85A vaccine in addition to BCG injection is not effective in preventing tuberculosis.[120]
Public health
Public health campaigns which have focused on overcrowding, public spitting and regular sanitation (including hand washing) during the 1800s helped to either interrupt or slow spread which when combined with contact tracing, isolation and treatment helped to dramatically curb the transmission of both tuberculosis and other airborne diseases which led to the elimination of tuberculosis as a major public health issue in most developed economies.[121][122] Other risk factors which worsened TB spread such as malnutrition were also ameliorated, but since the emergence of HIV a new population of immunocompromised individuals was available for TB to infect.
The World Health Organization (WHO) declared TB a "global health emergency" in 1993,
The benefits and risks of giving anti-tubercular drugs in those exposed to MDR-TB is unclear.[126] Making HAART therapy available to HIV-positive individuals significantly reduces the risk of progression to an active TB infection by up to 90% and can mitigate the spread through this population.[127]
Treatment

Treatment of TB uses antibiotics to kill the bacteria. Effective TB treatment is difficult, due to the unusual structure and chemical composition of the mycobacterial cell wall, which hinders the entry of drugs and makes many antibiotics ineffective.[128]
Active TB is best treated with combinations of several antibiotics to reduce the risk of the bacteria developing
Acetylsalicylic acid (aspirin) at a dose of 100 mg per day has been shown to improve clinical signs and symptoms, reduce cavitary lesions, lower inflammatory markers, and increase the rate of sputum-negative conversion in patients with pulmonary tuberculosis.[130]
Latent TB
Latent TB is treated with either
The treatment takes three to nine months depending on the medications used.[74][131][134][133] People with latent infections are treated to prevent them from progressing to active TB disease later in life.[135]
Education or counselling may improve the latent tuberculosis treatment completion rates.[136]
New onset
The recommended treatment of new-onset pulmonary tuberculosis, as of 2010[update], is six months of a combination of antibiotics containing rifampicin, isoniazid, pyrazinamide, and ethambutol for the first two months, and only rifampicin and isoniazid for the last four months.[15] Where resistance to isoniazid is high, ethambutol may be added for the last four months as an alternative.[15] Treatment with anti-TB drugs for at least 6 months results in higher success rates when compared with treatment less than 6 months, even though the difference is small. Shorter treatment regimen may be recommended for those with compliance issues.[137] There is also no evidence to support shorter anti-tuberculosis treatment regimens when compared to a 6-month treatment regimen.[138] However recently, results from an international, randomized, controlled clinical trial indicate that a four-month daily treatment regimen containing high-dose, or "optimized", rifapentine with moxifloxacin (2PHZM/2PHM) is as safe and effective as the existing standard six-month daily regimen at curing drug-susceptible tuberculosis (TB) disease.[139]
Recurrent disease
If tuberculosis recurs, testing to determine which antibiotics it is sensitive to is important before determining treatment.
Medication administration
Medication resistance
Primary resistance occurs when a person becomes infected with a resistant strain of TB. A person with fully susceptible MTB may develop secondary (acquired) resistance during therapy because of inadequate treatment, not taking the prescribed regimen appropriately (lack of compliance), or using low-quality medication.[145] Drug-resistant TB is a serious public health issue in many developing countries, as its treatment is longer and requires more expensive drugs. MDR-TB is defined as resistance to the two most effective first-line TB drugs: rifampicin and isoniazid. Extensively drug-resistant TB is also resistant to three or more of the six classes of second-line drugs.[146] Totally drug-resistant TB is resistant to all currently used drugs.[147] It was first observed in 2003 in Italy,[148] but not widely reported until 2012,[147][149] and has also been found in Iran and India.[150] There is some efficacy for linezolid to treat those with XDR-TB but side effects and discontinuation of medications were common.[151][152] Bedaquiline is tentatively supported for use in multiple drug-resistant TB.[153]
XDR-TB is a term sometimes used to define extensively resistant TB, and constitutes one in ten cases of MDR-TB. Cases of XDR TB have been identified in more than 90% of countries.[150]
For those with known rifampicin or MDR-TB, molecular tests such as the Genotype MTBDRsl Assay (performed on culture isolates or smear positive specimens) may be useful to detect second-line anti-tubercular drug resistance.[154][155]
Prognosis

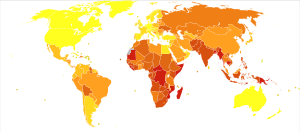
| no data ≤10 10–25 25–50 50–75 75–100 100–250 | 250–500 500–750 750–1000 1000–2000 2000–3000 ≥ 3000 |
Progression from TB infection to overt TB disease occurs when the bacilli overcome the immune system defenses and begin to multiply. In primary TB disease (some 1–5% of cases), this occurs soon after the initial infection.[14] However, in the majority of cases, a latent infection occurs with no obvious symptoms.[14] These dormant bacilli produce active tuberculosis in 5–10% of these latent cases, often many years after infection.[47]
The risk of reactivation increases with
In people with smear-positive pulmonary TB (without HIV co-infection), after 5 years without treatment, 50-60% die while 20-25% achieve spontaneous resolution (cure). TB is almost always fatal in those with untreated HIV co-infection and death rates are increased even with antiretroviral treatment of HIV.[159]
Epidemiology
Roughly one-quarter of the world's population has been infected with M. tuberculosis,
Tuberculosis[clarification needed] incidence is seasonal, with peaks occurring every spring and summer.[165][166][167][168] The reasons for this are unclear, but may be related to vitamin D deficiency during the winter.[168][169] There are also studies linking tuberculosis to different weather conditions like low temperature, low humidity and low rainfall. It has been suggested that tuberculosis incidence rates may be connected to climate change.[170]
At-risk groups
Tuberculosis is closely linked to both overcrowding and malnutrition, making it one of the principal diseases of poverty.[15] Those at high risk thus include: people who inject illicit drugs, inhabitants and employees of locales where vulnerable people gather (e.g., prisons and homeless shelters), medically underprivileged and resource-poor communities, high-risk ethnic minorities, children in close contact with high-risk category patients, and health-care providers serving these patients.[171]
The rate of tuberculosis varies with age. In Africa, it primarily affects adolescents and young adults.
In Canada and Australia, tuberculosis is many times more common among the Indigenous peoples, especially in remote areas.[174][175] Factors contributing to this include higher prevalence of predisposing health conditions and behaviours, and overcrowding and poverty. In some Canadian Indigenous groups, genetic susceptibility may play a role.[76]
Socioeconomic status (SES) strongly affects TB risk. People of low SES are both more likely to contract TB and to be more severely affected by the disease. Those with low SES are more likely to be affected by risk factors for developing TB (e.g., malnutrition, indoor air pollution, HIV co-infection, etc.), and are additionally more likely to be exposed to crowded and poorly ventilated spaces. Inadequate healthcare also means that people with active disease who facilitate spread are not diagnosed and treated promptly; sick people thus remain in the infectious state and (continue to) spread the infection.[76]
Geographical epidemiology
The distribution of tuberculosis is not uniform across the globe; about 80% of the population in many African, Caribbean, South Asian, and eastern European countries test positive in tuberculin tests, while only 5–10% of the U.S. population test positive.[14] Hopes of totally controlling the disease have been dramatically dampened because of many factors, including the difficulty of developing an effective vaccine, the expensive and time-consuming diagnostic process, the necessity of many months of treatment, the increase in HIV-associated tuberculosis, and the emergence of drug-resistant cases in the 1980s.[15]
In developed countries, tuberculosis is less common and is found mainly in urban areas. In Europe, deaths from TB fell from 500 out of 100,000 in 1850 to 50 out of 100,000 by 1950. Improvements in public health were reducing tuberculosis even before the arrival of antibiotics, although the disease remained a significant threat to public health, such that when the
In 2010, rates per 100,000 people in different areas of the world were: globally 178, Africa 332, the Americas 36, Eastern Mediterranean 173, Europe 63, Southeast Asia 278, and Western Pacific 139.[163]
Russia
Russia has achieved particularly dramatic progress with a decline in its TB mortality rate—from 61.9 per 100,000 in 1965 to 2.7 per 100,000 in 1993;[177][178] however, mortality rate increased to 24 per 100,000 in 2005 and then recoiled to 11 per 100,000 by 2015.[179]
China
China has achieved particularly dramatic progress, with about an 80% reduction in its TB mortality rate between 1990 and 2010.[163] The number of new cases has declined by 17% between 2004 and 2014.[150]
Africa
In 2007, the country with the highest estimated incidence rate of TB was Eswatini, with 1,200 cases per 100,000 people. In 2017, the country with the highest estimated incidence rate as a % of the population was Lesotho, with 665 cases per 100,000 people.[180]
In South Africa, 54 200 people died in 2022 from TB. The incidence rate was 468 per 100 000 people; in 2015, this was 988 per 100 000. The total incidence was 280 000 in 2022; in 2015, this was 552 000.[181]
India
As of 2017, India had the largest total incidence, with an estimated 2,740,000 cases.[180] According to the World Health Organization (WHO), in 2000–2015, India's estimated mortality rate dropped from 55 to 36 per 100,000 population per year with estimated 480 thousand people died of TB in 2015.[182][183] In India a major proportion of tuberculosis patients are being treated by private partners and private hospitals. Evidence indicates that the tuberculosis national survey does not represent the number of cases that are diagnosed and recorded by private clinics and hospitals in India.[184]
North America
In the United States, Native Americans have a fivefold greater mortality from TB,[185] and racial and ethnic minorities accounted for 84% of all reported TB cases.[186] The overall tuberculosis case rate in the United States was 3 per 100,000 persons in 2017.[180]
In Canada, tuberculosis was endemic in some rural areas as of 1998.[187]
Western Europe
In 2017, in the United Kingdom, the national average was 9 per 100,000 and the highest incidence rates in Western Europe were 20 per 100,000 in Portugal.
-
Number of new cases of tuberculosis per 100,000 people in 2016[188]
-
Tuberculosis deaths per million persons in 2012
-
Tuberculosis deaths by region, 1990 to 2017[189]
Society and culture
Names
Tuberculosis has been known by many names from the technical to the familiar.[190] Phthisis (Φθισις) is a Greek word for consumption, an old term for pulmonary tuberculosis;[7] around 460 BCE, Hippocrates described phthisis as a disease of dry seasons.[191] The abbreviation TB is short for tubercle bacillus. Consumption was the most common nineteenth century English word for the disease, and was also in use well into the twentieth century. The Latin root con meaning 'completely' is linked to sumere meaning 'to take up from under'.[192] In The Life and Death of Mr Badman by John Bunyan, the author calls consumption "the captain of all these men of death."[193] "Great white plague" has also been used.[190]
Art and literature

Tuberculosis was for centuries associated with
Tuberculosis formed an often-reused theme in
Public health efforts
In 2014, the WHO adopted the "End TB" strategy which aims to reduce TB incidence by 80% and TB deaths by 90% by 2030.[207] The strategy contains a milestone to reduce TB incidence by 20% and TB deaths by 35% by 2020.[208] However, by 2020 only a 9% reduction in incidence per population was achieved globally, with the European region achieving 19% and the African region achieving 16% reductions.[208] Similarly, the number of deaths only fell by 14%, missing the 2020 milestone of a 35% reduction, with some regions making better progress (31% reduction in Europe and 19% in Africa).[208] Correspondingly, also treatment, prevention and funding milestones were missed in 2020, for example only 6.3 million people were started on TB prevention short of the target of 30 million.[208]
The World Health Organization (WHO), the
India had the highest total number of TB cases worldwide in 2010, in part due to poor disease management within the private and public health care sector.
A 2014 EIU-healthcare report finds there is a need to address apathy and urges for increased funding. The report cites among others Lucica Ditui "[TB] is like an orphan. It has been neglected even in countries with a high burden and often forgotten by donors and those investing in health interventions."[150]
Slow progress has led to frustration, expressed by the executive director of the
There is insufficient data to show that active contact tracing helps to improve case detection rates for tuberculosis.[217] Interventions such as house-to-house visits, educational leaflets, mass media strategies, educational sessions may increase tuberculosis detection rates in short-term.[218] There is no study that compares new methods of contact tracing such as social network analysis with existing contact tracing methods.[219]
Stigma
Slow progress in preventing the disease may in part be due to
Stigma towards TB may result in delays in seeking treatment,[150] lower treatment compliance, and family members keeping cause of death secret[220] – allowing the disease to spread further.[150] In contrast, in Russia stigma was associated with increased treatment compliance.[220] TB stigma also affects socially marginalized individuals to a greater degree and varies between regions.[220]
One way to decrease stigma may be through the promotion of "TB clubs", where those infected may share experiences and offer support, or through counseling.[220] Some studies have shown TB education programs to be effective in decreasing stigma, and may thus be effective in increasing treatment adherence.[220] Despite this, studies on the relationship between reduced stigma and mortality are lacking as of 2010[update], and similar efforts to decrease stigma surrounding AIDS have been minimally effective.[220] Some have claimed the stigma to be worse than the disease, and healthcare providers may unintentionally reinforce stigma, as those with TB are often perceived as difficult or otherwise undesirable.[150] A greater understanding of the social and cultural dimensions of tuberculosis may also help with stigma reduction.[221]
Research
The BCG vaccine has limitations, and research to develop new TB vaccines is ongoing.[222] A number of potential candidates are currently in phase I and II clinical trials.[222][223] Two main approaches are used to attempt to improve the efficacy of available vaccines. One approach involves adding a subunit vaccine to BCG, while the other strategy is attempting to create new and better live vaccines.[222] MVA85A, an example of a subunit vaccine, is in trials in South Africa as of 2006, is based on a genetically modified vaccinia virus.[224] Vaccines are hoped to play a significant role in treatment of both latent and active disease.[225]
To encourage further discovery, researchers and policymakers are promoting new economic models of vaccine development as of 2006, including prizes, tax incentives, and
In 2012 a new medication regimen was approved in the US for multidrug-resistant tuberculosis, using bedaquiline as well as existing drugs. There were initial concerns about the safety of this drug,[232][233][234][235][236] but later research on larger groups found that this regimen improved health outcomes.[237] By 2017 the drug was used in at least 89 countries.[238] Another new drug is delamanid, which was first approved by the European Medicines Agency in 2013 to be used in multidrug-resistant tuberculosis patients,[239] and by 2017 was used in at least 54 countries.[240]
Steroids add-on therapy has not shown any benefits for active pulmonary tuberculosis infection.[241]
Other animals
Mycobacteria infect many different animals, including birds,[242] fish, rodents,[243] and reptiles.[244] The subspecies Mycobacterium tuberculosis, though, is rarely present in wild animals.[245] An effort to eradicate bovine tuberculosis caused by Mycobacterium bovis from the cattle and deer herds of New Zealand has been relatively successful.[246] Efforts in Great Britain have been less successful.[247][248]
As of 2015[update], tuberculosis appears to be widespread among captive elephants in the US. It is believed that the animals originally acquired the disease from humans, a process called reverse zoonosis. Because the disease can spread through the air to infect both humans and other animals, it is a public health concern affecting circuses and zoos.[249][250]
See also
Notes
References
- ^ a b c d e f g h i j k l m n o p "Tuberculosis (TB)". who.int. Archived from the original on 30 July 2020. Retrieved 8 May 2020.
- ISBN 978-0-323-07699-9.
- ^ PMID 25428938.
- ^ ISBN 978-92-4-154667-6. Archivedfrom the original on 2 June 2021. Retrieved 17 September 2017.
- ^ ISBN 978-0-7637-8047-0. Archivedfrom the original on 7 February 2024. Retrieved 17 September 2017.
- ^ a b c d "Tuberculosis (TB)". World Health Organization (WHO). 16 February 2018. Archived from the original on 30 December 2013. Retrieved 15 September 2018.
- ^ ISBN 978-81-86062-25-8. Archivedfrom the original on 6 September 2015.
- ^ ISBN 978-0-443-06839-3.
- ^ "Basic TB Facts". Centers for Disease Control and Prevention (CDC). 13 March 2012. Archived from the original on 6 February 2016. Retrieved 11 February 2016.
- ^ .
- ^ a b "Tuberculosis". World Health Organization (WHO). 2002. Archived from the original on 17 June 2013.
- ^ a b "Tuberculosis (TB)". WHO. Archived from the original on 30 July 2020. Retrieved 16 October 2021.
- ^ "Global tuberculosis report". World Health Organization (WHO). Archived from the original on 30 December 2013. Retrieved 9 November 2017.
- ^ OCLC 69672074.
- ^ S2CID 208791546.
- PMID 11438894.
- S2CID 6577678.
- PMID 19855821.
- PMID 12517873.
- PMID 12454182.
- (PDF) from the original on 18 February 2017.
- Who Named It?
- PMID 4914685.
- ^ Marten B (1720). A New Theory of Consumptions—More Especially a Phthisis or Consumption of the Lungs. London, England: T. Knaplock. Archived from the original on 26 March 2023. Retrieved 8 December 2020. P. 51: "The Original and Essential Cause ... may possibly be some certain Species of Animalcula or wonderfully minute living Creatures, ... " P. 79: "It may be therefore very likely, that by an habitual lying in the same Bed with a Consumptive Patient, constantly Eating and Drinking with him, or by very frequently conversing so nearly, as to draw in part of the Breath he emits from his Lungs, a Consumption may be caught by a sound Person; ... "
- ^ Laennec RT (1819). De l'auscultation médiate ... (in French). Vol. 1. Paris, France: J.-A. Brosson et J.-S Chaudé. p. 20. Archived from the original on 2 June 2021. Retrieved 6 December 2020. From p. 20: "L'existence des tubercules dans le poumon est la cause et constitue le charactère anatomique propre de la phthisie pulmonaire (a). (a) ... l'effet dont cette maladie tire son nom, c'est-à-dire, la consumption." (The existence of tubercles in the lung is the cause and constitutes the unique anatomical characteristic of pulmonary tuberculosis (a). (a) ... the effect from which this malady [pulmonary tuberculosis] takes its name, that is, consumption.)
- ^ Schönlein JL (1832). Allgemeine und specielle Pathologie und Therapie [General and Special Pathology and Therapy] (in German). Vol. 3. Würzburg, (Germany): C. Etlinger. p. 103. Archived from the original on 2 June 2021. Retrieved 6 December 2020.
- S2CID 53027676. See especially Appendix, p. iii.
- ^ "Kentucky: Mammoth Cave long on history". CNN. 27 February 2004. Archived from the original on 13 August 2006. Retrieved 8 October 2006.
- ^ from the original on 3 August 2012. Retrieved 28 September 2011.
- ^ Villemin JA (1865). "Cause et nature de la tuberculose" [Cause and nature of tuberculosis]. Bulletin de l'Académie Impériale de Médecine (in French). 31: 211–216. Archived from the original on 9 December 2021. Retrieved 6 December 2020.
- See also: Villemin JA (1868). Etudes sur la tuberculose: preuves rationnelles et expérimentales de sa spécificité et de son inoculabilité [Studies of tuberculosis: rational and experimental evidence of its specificity and inoculability] (in French). Paris, France: J.-B. Baillière et fils. Archived from the original on 7 February 2024. Retrieved 6 December 2020.
- ^ Burdon-Sanderson, John Scott. (1870) "Introductory Report on the Intimate Pathology of Contagion." Appendix to: Twelfth Report to the Lords of Her Majesty's Most Honourable Privy Council of the Medical Officer of the Privy Council [for the year 1869], Parliamentary Papers (1870), vol. 38, 229–256.
- ISBN 978-3-662-56454-7. Archivedfrom the original on 6 November 2018. Retrieved 15 June 2021.
- ^ "History: World TB Day". Centers for Disease Control and Prevention (CDC). 12 December 2016. Archived from the original on 7 December 2018. Retrieved 23 March 2019.
- ^ "The Nobel Prize in Physiology or Medicine 1905". www.nobelprize.org. Archived from the original on 10 December 2006. Retrieved 7 October 2006.
- ISBN 978-1-55581-072-6.
- ^ Frith J. "History of Tuberculosis. Part 1 – Phthisis, consumption and the White Plague". Journal of Military and Veterans' Health. Archived from the original on 8 April 2021. Retrieved 26 February 2021.
- PMID 27706149.
- PMID 14968644.
- ISBN 978-1-58603-832-8. Archivedfrom the original on 7 September 2015.
- PMID 16337557.
- PMID 7811874.
- ^ ISBN 978-1-4587-6712-7. Archivedfrom the original on 6 September 2015.
- ISBN 978-0-7817-7982-1. Archivedfrom the original on 6 September 2015.
- S2CID 24221563.
- ^ "Frequently asked questions about TB and HIV". World Health Organization (WHO). Archived from the original on 8 August 2011. Retrieved 15 April 2012.
- ^ Schiffman G (15 January 2009). "Tuberculosis Symptoms". eMedicine Health. Archived from the original on 16 May 2009.
- ^ ISBN 978-0-7279-1605-1. Archivedfrom the original on 8 December 2015.
- ISBN 978-81-8448-749-7. Archivedfrom the original on 6 September 2015.
- PMID 24624281.
- ISBN 978-93-5025-073-0. Archivedfrom the original on 7 September 2015.
- ^ PMID 16300038.
- ^ ISBN 978-1-4200-6749-1. Archivedfrom the original on 6 September 2015.
- ISBN 978-0-07-147722-2.
- ISBN 978-93-5025-073-0. Archivedfrom the original on 6 September 2015.
- PMID 20060722.
- ^ PMID 11475314.
- S2CID 28960959.
- ISBN 978-0-07-463223-9. Archivedfrom the original on 6 September 2015.
- ^ "Acid-Fast Stain Protocols". 21 August 2013. Archived from the original on 1 October 2011. Retrieved 26 March 2016.
- PMID 6208117.
- ISBN 978-1-934115-24-4. Archivedfrom the original on 6 September 2015.
- PMID 9336935.
- PMID 12202584.
- PMID 12791879.
- PMID 16387455.
- ISBN 978-1-4649-0122-5. Archivedfrom the original on 6 September 2015.
- PMID 9866740.
- PMID 20488936.
- PMID 9279284.
- PMID 9721404.
- PMID 15764538.
- ^ PMID 21514230.
- ^ a b "Tuberculosis Fact sheet N°104". World Health Organization (WHO). November 2010. Archived from the original on 4 October 2006. Retrieved 26 July 2011.
- ^ a b "Core Curriculum on Tuberculosis: What the Clinician Should Know" (PDF) (5th ed.). Centers for Disease Control and Prevention (CDC), Division of Tuberculosis Elimination. 2011. p. 24. Archived (PDF) from the original on 19 May 2012.
- ^ "Causes of Tuberculosis". Mayo Clinic. 21 December 2006. Archived from the original on 18 October 2007. Retrieved 19 October 2007.
- ^ PMID 23476764.
- ^ a b c "The sixteenth global report on tuberculosis" (PDF). World Health Organization (WHO). 2011. Archived from the original (PDF) on 6 September 2012.
- ^ "Global tuberculosis control–surveillance, planning, financing WHO Report 2006". World Health Organization (WHO). Archived from the original on 12 December 2006. Retrieved 13 October 2006.
- PMID 18337598.
- PMID 17638190.
- from the original on 17 December 2004.
- PMID 20044459.
These analyses indicate that smokers are almost twice as likely to be infected with TB and to progress to active disease (RR of about 1.5 for latent TB infection (LTBI) and RR of ~2.0 for TB disease). Smokers are also twice as likely to die from TB (RR of about 2.0 for TB mortality), but data are difficult to interpret because of heterogeneity in the results across studies.
- ^ "TB Risk Factors". CDC. 18 March 2016. Archived from the original on 30 August 2020. Retrieved 25 August 2020.
- PMID 20206579.
- ^ Good JM, Cooper S, Doane AS (1835). The Study of Medicine. Harper. p. 32. Archived from the original on 10 August 2016.
- ^ ISBN 978-0-7637-9751-5.
- ^ ISBN 978-1-60327-238-4. Archivedfrom the original on 6 September 2015.
- PMID 16406837.
- PMID 29218036.
- ISBN 978-81-312-2804-3. Archivedfrom the original on 6 September 2015.
- PMID 15620608.
- PMID 15857515.
- ^ PMID 12604509.
- PMID 24804000.
- ISBN 978-0-7637-6591-0. Archivedfrom the original on 6 September 2015.
- ISBN 978-92-4-154634-8. Archivedfrom the original on 6 September 2015.
- PMID 19114163.
- ^ S2CID 76156550.
- ^ S2CID 639982.
- PMID 21996694.
- ^ PMID 20847080.
- PMID 22069472.
- ISBN 978-92-4-156330-7. Archivedfrom the original on 6 September 2015.
- ^ National Institute for Health and Clinical Excellence. Clinical guideline 117: Tuberculosis. London, 2011.
- PMID 21857806.
- S2CID 25423684.
- PMID 18593687.
- ISBN 978-93-5025-073-0. Archivedfrom the original on 6 September 2015.
- PMID 20518271.
- PMID 27599331.
- PMID 30946831.
- PMID 31099768.
- S2CID 19924571.
- PMID 21893541.
- ^ "Vaccines | Basic TB Facts". CDC. 16 June 2021. Archived from the original on 30 December 2021. Retrieved 30 December 2021.
- PMID 25097193.
- ^ "Vaccine and Immunizations: TB Vaccine (BCG)". Centers for Disease Control and Prevention. 2011. Archived from the original on 17 November 2011. Retrieved 26 July 2011.
- ^ "BCG Vaccine Usage in Canada – Current and Historical". Public Health Agency of Canada. September 2010. Archived from the original on 30 March 2012. Retrieved 30 December 2011.
- ^ PMID 16714729.
- PMID 31038197.
- PMID 12435764.
- PMID 28515626.
- ^ "The Global Plan to Stop TB". World Health Organization (WHO). 2011. Archived from the original on 12 June 2011. Retrieved 13 June 2011.
- ISBN 978-0-19-857014-1. Archivedfrom the original on 6 September 2015.
- S2CID 39379915.
- PMID 16625639.
- PMID 21234380.
- PMID 7574484.
- PMID 17943842.
- PMID 35203473.
- ^ ISBN 978-92-4-155023-9. Archivedfrom the original on 2 June 2021. Retrieved 25 July 2018.
- PMID 29953429.
- ^ PMID 32053584.
- PMID 29910114.
- PMID 21441678.
- PMID 22592714.
- PMID 10796641.
- PMID 31828771.
- ^ "Landmark TB Trial Identifies Shorter-Course Treatment Regimen". CDC. NCHHSTP Media Team Centers for Disease Control and Prevention. 20 October 2020. Archived from the original on 27 November 2021. Retrieved 27 November 2021.
- ISBN 978-1-60327-238-4. Archivedfrom the original on 6 September 2015.
- ^ PMID 26022367.
- PMID 25403701.
- PMID 11687088.
- PMID 24470141.
- PMID 7973169.
- from the original on 22 May 2017.
- ^ a b McKenna M (12 January 2012). "Totally Resistant TB: Earliest Cases in Italy". Wired. Archived from the original on 14 January 2012. Retrieved 12 January 2012.
- PMID 17868596.
- ^ "Totally Drug-Resistant TB: a WHO consultation on the diagnostic definition and treatment options" (PDF). World Health Organization (WHO). Archived (PDF) from the original on 21 October 2016. Retrieved 25 March 2016.
- ^ a b c d e f g h i j k l m n o p Kielstra P (30 June 2014). Tabary Z (ed.). "Ancient enemy, modern imperative – A time for greater action against tuberculosis" (PDF). The Economist. Economist Intelligence Unit. Archived from the original (PDF) on 10 August 2014. Retrieved 22 January 2022.
- PMID 30893466.
- PMID 19349380.
- ^ "Provisional CDC Guidelines for the Use and Safety Monitoring of Bedaquiline Fumarate (Sirturo) for the Treatment of Multidrug-Resistant Tuberculosis". Archived from the original on 4 January 2014.
- PMID 27605387.
- ^ "The use of molecular line probe assays for the detection of resistance to second-line anti-tuberculosis drugs" (PDF). World Health Organization. Archived (PDF) from the original on 22 September 2021. Retrieved 18 June 2021.
- ^ "WHO Disease and injury country estimates". World Health Organization (WHO). 2004. Archived from the original on 11 November 2009. Retrieved 11 November 2009.
- PMID 12726976.
- PMID 17570116.
- ^ "1.4 Prognosis - Tuberculosis". medicalguidelines.msf.org. Archived from the original on 2 June 2021. Retrieved 25 August 2020.
- ^ "Fact Sheets: The Difference Between Latent TB Infection and Active TB Disease". Centers for Disease Control and Prevention (CDC). 20 June 2011. Archived from the original on 4 August 2011. Retrieved 26 July 2011.
- ^ "Global tuberculosis report 2013". World Health Organization (WHO). 2013. Archived from the original on 12 December 2006.
- from the original on 19 May 2020. Retrieved 18 March 2020.
- ^ a b c "Global Tuberculosis Control 2011" (PDF). World Health Organization (WHO). Archived from the original (PDF) on 17 June 2012. Retrieved 15 April 2012.
- ^ "Tuberculosis". WHO. 24 March 2020. Archived from the original on 30 July 2020. Retrieved 31 May 2020.
- PMID 8984709.
- PMID 22025704.
- PMID 22236842.
- ^ PMID 22410705.
- PMID 23483924.
- PMID 31481739.
- PMID 8964016.
- ^ "Global Tuberculosis Control Report, 2006 – Annex 1 Profiles of high-burden countries" (PDF). World Health Organization (WHO). Archived from the original (PDF) on 26 July 2009. Retrieved 13 October 2006.
- ^ "2005 Surveillance Slide Set". Centers for Disease Control and Prevention. 12 September 2006. Archived from the original on 23 November 2006. Retrieved 13 October 2006.
- PMID 10693593.
- ISBN 978-0-12-375087-7. Archivedfrom the original on 6 September 2015.
- Medical Research Council. Archived from the originalon 11 April 2008. Retrieved 7 October 2006.
- ISBN 0-8330-2446-9. Archivedfrom the original on 20 February 2023. Retrieved 20 February 2023.
- ^ "Global Tuberculosis Control". World Health Organization. 2011. Archived from the original on 12 December 2006.
- ^ "WHO global tuberculosis report 2016. Annex 2. Country profiles: Russian Federation". Archived from the original on 14 July 2017. Retrieved 22 August 2020.
- ^ a b c "Global Tuberculosis Report 2018" (PDF). Archived (PDF) from the original on 7 August 2020. Retrieved 27 September 2019.
- ^ Tomlinson, Catherine (10 November 2023). "In-depth: What new WHO TB numbers mean for South Africa". Spotlight. Retrieved 27 March 2024.
- ^ "WHO Global tuberculosis report 2016: India". Archived from the original on 6 February 2018. Retrieved 22 August 2020.
- ^ "Govt revisits strategy to combat tuberculosis". Daily News and Analysis. 8 April 2017. Archived from the original on 3 June 2021. Retrieved 22 August 2020.
- PMID 30064674.
- ISBN 978-0-19-988521-3. Archivedfrom the original on 6 September 2015.
- ^ "CDC Surveillance Slides 2012 – TB". Centers for Disease Control and Prevention. 24 October 2018. Archived from the original on 9 November 2013. Retrieved 17 September 2017.
- ^ Al-Azem A, Kaushal Sharma M, Turenne C, Hoban D, Hershfield E, MacMorran J, Kabani A (1998). "Rural outbreaks of Mycobacterium tuberculosis in a Canadian province". Abstr Intersci Conf Antimicrob Agents Chemother. 38: 555. abstract no. L-27. Archived from the original on 18 November 2011.
- ^ "Tuberculosis incidence (per 100,000 people)". Our World in Data. Archived from the original on 26 September 2019. Retrieved 7 March 2020.
- ^ "Tuberculosis deaths by region". Our World in Data. Archived from the original on 8 May 2020. Retrieved 7 March 2020.
- ^ a b c Lawlor C. "Katherine Byrne, Tuberculosis and the Victorian Literary Imagination". British Society for Literature and Science. Archived from the original on 6 November 2020. Retrieved 11 June 2017.
- ^ "Hippocrates 3.16 Classics, MIT". Archived from the original on 11 February 2005. Retrieved 15 December 2015.
{{cite web}}: CS1 maint: unfit URL (link) - ISBN 978-0-689-11810-4.
- ^ Bunyan J (1808). The Life and Death of Mr. Badman. London: W. Nicholson. p. 244. Retrieved 28 September 2016 – via Internet Archive.
captain.
- ISBN 978-1-107-67280-2.
- ^ "About Chopin's illness". Icons of Europe. Archived from the original on 28 September 2017. Retrieved 11 June 2017.
- PMID 27993687.
- ISBN 978-0-313-29916-2. Archivedfrom the original on 2 June 2021. Retrieved 4 October 2017.
- ^ Eschner K. "George Orwell Wrote '1984' While Dying of Tuberculosis". Smithsonian. Archived from the original on 24 March 2019. Retrieved 25 March 2019.
- ^ "Tuberculosis (whole issue)". Journal of the American Medical Association. 293 (22): cover. 8 June 2005. Archived from the original on 24 August 2020. Retrieved 4 October 2017.
- S2CID 191371443.
- ^ Wilsey AM (May 2012). 'Half in Love with Easeful Death:' Tuberculosis in Literature. Humanities Capstone Projects (PhD Thesis thesis). Pacific University. Archived from the original on 11 October 2017. Retrieved 28 September 2017.
- ^ PMID 12463180.
- ^ "Pulmonary Tuberculosis/In Literature and Art". McMaster University History of Diseases. Retrieved 9 June 2017.
- ^ Thomson G (1 June 2016). "Van Morrison – 10 of the best". The Guardian. Archived from the original on 14 August 2020. Retrieved 28 September 2017.
- ^ "Tuberculosis Throughout History: The Arts" (PDF). United States Agency for International Development (USAID). Archived (PDF) from the original on 30 June 2017. Retrieved 12 June 2017.
- ^ Corliss R (22 December 2008). "Top 10 Worst Christmas Movies". Time. Archived from the original on 22 September 2020. Retrieved 28 September 2017.
'If you don't cry when Bing Crosby tells Ingrid Bergman she has tuberculosis', Joseph McBride wrote in 1973, 'I never want to meet you, and that's that.'
- ^ "The End TB Strategy". who.int. Archived from the original on 22 July 2021. Retrieved 22 July 2021.
- ^ ISBN 978-92-4-001313-1. Archivedfrom the original on 22 July 2021. Retrieved 22 July 2021.
- ^ a b "Public–Private Partnership Announces Immediate 40 Percent Cost Reduction for Rapid TB Test" (PDF). World Health Organization (WHO). 6 August 2012. Archived (PDF) from the original on 29 October 2013.
- PMID 21958145.
- ^ "WHO says Cepheid rapid test will transform TB care". Reuters. 8 December 2010. Archived from the original on 11 December 2010.
- ^ STOPTB (5 April 2013). "The Stop TB Partnership, which operates through a secretariat hosted by the World Health Organization (WHO) in Geneva, Switzerland" (PDF). Archived (PDF) from the original on 24 January 2014.
- PMID 22140369.
- PMID 21731301.
- ^ Bhargava A, Pinto L, Pai M (2011). "Mismanagement of tuberculosis in India: Causes, consequences, and the way forward" (PDF). Hypothesis. 9 (1): e7. Archived from the original on 14 March 2016.
{{cite journal}}: CS1 maint: unfit URL (link) - S2CID 41788291.
- PMID 21901723.
- PMID 29182800.
- PMID 31461540.
- ^ PMID 20626191.
- PMID 25997539.
- ^ PMID 21420568.
- PMID 29341430.
- PMID 16870530.
- PMID 21029966.
- ^ Webber D, Kremer M (2001). "Stimulating Industrial R&D for Neglected Infectious Diseases: Economic Perspectives" (PDF). Bulletin of the World Health Organization. 79 (8): 693–801. Archived (PDF) from the original on 26 September 2007.
- S2CID 154454583. Archived from the originalon 5 November 2006.
- ISBN 978-92-1-104596-3. Archivedfrom the original on 6 September 2015.
- ISBN 978-1-60795-045-5. Archivedfrom the original on 6 September 2015.
- ^ Bill and Melinda Gates Foundation Announcement (12 February 2004). "Gates Foundation Commits $82.9 Million to Develop New Tuberculosis Vaccines". Archived from the original on 10 October 2009.
- ^ Nightingale K (19 September 2007). "Gates foundation gives US$280 million to fight TB". Archived from the original on 1 December 2008.
- from the original on 12 January 2020. Retrieved 8 May 2020.
- ^ "J&J Sirturo Wins FDA Approval to Treat Drug-Resistant TB". Bloomberg News. 31 December 2012. Archived from the original on 4 January 2013. Retrieved 1 January 2013.
- PMID 23430122.
- ^ US Food and Drug Administration. "Briefing Package: NDA 204–384: Sirturo" (PDF). Food and Drug Administration. Archived (PDF) from the original on 4 January 2014.
- from the original on 29 March 2022. Retrieved 29 March 2022.
- PMID 31002070.
- PMID 34690963.
- ^ "European Medicines Agency - News and Events - European Medicines Agency recommends two new treatment options for tuberculosis". 3 December 2013. Archived from the original on 3 December 2013. Retrieved 9 April 2024.
- PMID 34690963.
- PMID 25387839.
- PMID 22244112.
- PMID 22244111.
- PMID 22244116.
- ISBN 978-0-8138-0589-4. Archivedfrom the original on 6 September 2015.
- PMID 16330161.
- PMID 18706814.
- PMID 19846226.
- ^ Holt N (24 March 2015). "The Infected Elephant in the Room". Slate. Archived from the original on 14 April 2016. Retrieved 5 April 2016.
- ^ Mikota SK. "A Brief History of TB in Elephants" (PDF). Animal and Plant Health Inspection Service (APHIS). Archived (PDF) from the original on 6 October 2016. Retrieved 5 April 2016.
External links
- Tuberculosis at Curlie
- "Tuberculosis (TB)". Centers for Disease Control and Prevention (CDC). 24 October 2018.
- "Tuberculosis (TB)". London: Health Protection Agency. Archived from the original on 5 July 2007.
- WHO global 2016 TB report (infographic)
- WHO tuberculosis country profiles
- "Tuberculosis Among African Americans", 1990-11-01, In Black America; KUT Radio, American Archive of Public Broadcasting (WGBH and the Library of Congress)
- Working Group on New TB drugs, tracking clinical trials and drug candidates