Renin–angiotensin system

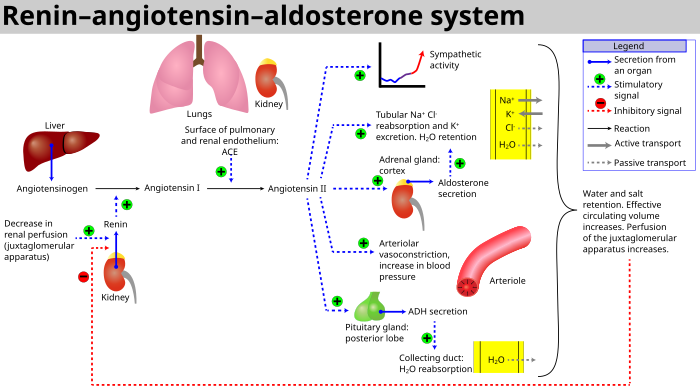
The renin–angiotensin system (RAS), or renin–angiotensin–aldosterone system (RAAS), is a hormone system that regulates blood pressure, fluid and electrolyte balance, and systemic vascular resistance.[2][3]
When
Angiotensin III increases blood pressure and stimulates aldosterone secretion from the adrenal cortex; it has 100% adrenocortical stimulating activity and 40% vasopressor activity of angiotensin II.
Angiotensin II is a potent vasoconstrictive peptide that causes blood vessels to narrow, resulting in increased blood pressure.[6] Angiotensin II also stimulates the secretion of the hormone aldosterone[6] from the adrenal cortex. Aldosterone causes the renal tubules to increase the reabsorption of sodium which in consequence causes the reabsorption of water into the blood, while at the same time causing the excretion of potassium (to maintain electrolyte balance). This increases the volume of extracellular fluid in the body, which also increases blood pressure.
If the RAS is abnormally active, blood pressure will be too high. There are several types of drugs which includes
Activation
The system can be activated when there is a loss of
- If the perfusion of the juxtaglomerular apparatus in the kidney's macula densa decreases, then the juxtaglomerular cells (granular cells, modified pericytes in the glomerular capillary) release the enzyme renin.
- Renin angiotensinogen, a globular protein. The decapeptide is known as angiotensin I.
- Angiotensin I is then converted to an octapeptide, angiotensin II by angiotensin-converting enzyme (ACE),[9] which is thought to be found mainly in endothelial cells of the capillaries throughout the body, within the lungs and the epithelial cells of the kidneys. One study in 1992 found ACE in all blood vessel endothelial cells.[10]
- Angiotensin II is the major bioactive product of the renin–angiotensin system, binding to receptors on paracrine, and intracrinehormone.
Cardiovascular effects

Angiotensin I may have some minor activity, but angiotensin II is the major bio-active product. Angiotensin II has a variety of effects on the body:[citation needed]
- Throughout the body, angiotensin II is a potent vasoconstrictor of arterioles.
- In the kidneys, angiotensin II constricts plasma proteins) in the peritubular capillaries. The effect of decreased hydrostatic pressure and increased oncotic pressure in the peritubular capillaries will facilitate increased reabsorption of tubular fluid.
- Angiotensin II decreases medullary blood flow through the vasa recta. This decreases the washout of NaCl and urea in the kidney medullary space. Thus, higher concentrations of NaCl and urea in the medulla facilitate increased absorption of tubular fluid. Furthermore, increased reabsorption of fluid into the medulla will increase passive reabsorption of sodium along the thick ascending limb of the Loop of Henle.
- Angiotensin II stimulates Na+
/H+
exchangers located on the apical membranes (faces the tubular lumen) of cells in the proximal tubule and thick ascending limb of the loop of Henle in addition to Na+
channels in the collecting ducts. This will ultimately lead to increased sodium reabsorption. - Angiotensin II stimulates the hypertrophy of renal tubule cells, leading to further sodium reabsorption.
- In the is secreted into the tubules, becomes part of urine and is excreted.
- Angiotensin II causes the release of anti-diuretic hormone (ADH),[6] also called vasopressin – ADH is made in the hypothalamus and released from the posterior pituitary gland. As its name suggests, it also exhibits vaso-constrictive properties, but its main course of action is to stimulate reabsorption of water in the kidneys. ADH also acts on the central nervous system to increase an individual's appetite for salt, and to stimulate the sensation of thirst.
These effects directly act together to increase blood pressure and are opposed by atrial natriuretic peptide (ANP).
Local renin–angiotensin systems
Locally expressed renin–angiotensin systems have been found in a number of tissues, including the
In the adrenal glands, it is likely involved in the
Fetal renin–angiotensin system
In the fetus, the renin–angiotensin system is predominantly a sodium-losing system,[citation needed] as angiotensin II has little or no effect on aldosterone levels. Renin levels are high in the fetus, while angiotensin II levels are significantly lower; this is due to the limited pulmonary blood flow, preventing ACE (found predominantly in the pulmonary circulation) from having its maximum effect.[citation needed]
Clinical significance

- ACE inhibitors of angiotensin-converting enzyme inhibitors are often used to reduce the formation of the more potent angiotensin II. Captopril is an example of an ACE inhibitor. ACE cleaves a number of other peptides, and in this capacity is an important regulator of the kinin–kallikrein system, as such blocking ACE can lead to side effects.[18]
- Angiotensin II receptor antagonists, also known as angiotensin receptor blockers, can be used to prevent angiotensin II from acting on its receptors.
- Direct renin inhibitors can also be used for hypertension.[19] The drugs that inhibit renin are aliskiren[20] and the investigational remikiren.[21]
- Vaccines against angiotensin II, for example CYT006-AngQb, have been investigated.[22][23]
See also
References
- OCLC 1127823558. Archivedfrom the original on 9 April 2022. Retrieved 8 April 2022.
- from the original on 29 April 2019. Retrieved 9 May 2019.
- PMID 31925571.
- from the original on 9 April 2022. Retrieved 8 April 2022.
- OCLC 1058067942. Archivedfrom the original on 9 April 2022. Retrieved 8 April 2022.
- ^ PMID 20380974.
- ^ Bakris GL (November 2022). "High Blood Pressure: Heart and Blood Vessel Disorders". Merck Manual Home Edition. Archived from the original on 5 November 2010. Retrieved 6 June 2008.
- ^ Solomon SD, Anavekar N (2005). "A Brief Overview of Inhibition of the Renin–Angiotensin System: Emphasis on Blockade of the Angiotensin II Type-1 Receptor". Medscape Cardiology. 9 (2). Archived from the original on 15 December 2019. Retrieved 6 June 2008.
- ^ PMID 16816138.
- S2CID 25785488.
- PMID 17878513.
- ^ PMID 9570034.[permanent dead link]
- ^ PMID 21087212.
- S2CID 39068591.
- S2CID 46657557.
- PMID 12676175.
- S2CID 23123825.
- PMID 10971519.
- ^ Mehta A (January 2011). "Direct Renin Inhibitors as Antihypertensive Drugs". Pharmaxchange. Archived from the original on 7 December 2010.
- PMID 15723979.
- PMID 8730917.
- S2CID 15175992.
- S2CID 15949.
Further reading
- Banic A, Sigurdsson GH, Wheatley AM (1993). "Influence of age on the cardiovascular response during graded haemorrhage in anaesthetized rats". Res Exp Med (Berl). 193 (5): 315–321. S2CID 37700794.
External links
- Renin-Angiotensin+System at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
