Monoamine oxidase inhibitor
| Monoamine oxidase inhibitor | |
|---|---|
N06AF | |
| Mechanism of action | Enzyme inhibitor |
| Biological target | Monoamine oxidase enzymes: MAO-A and/or MAO-B |
| External links | |
| MeSH | D008996 |
| Legal status | |
| In Wikidata | |
Monoamine oxidase inhibitors (MAOIs) are a class of drugs that inhibit the activity of one or both monoamine oxidase enzymes: monoamine oxidase A (MAO-A) and monoamine oxidase B (MAO-B). They are best known as effective antidepressants, especially for treatment-resistant depression and atypical depression.[1] They are also used to treat panic disorder, social anxiety disorder, Parkinson's disease, and several other disorders.
Reversible inhibitors of monoamine oxidase A (RIMAs) are a subclass of MAOIs that selectively and reversibly inhibit the MAO-A enzyme. RIMAs are used clinically in the treatment of depression and dysthymia. Due to their reversibility, they are safer in single-drug overdose than the older, irreversible MAOIs,[2] and weaker in increasing the monoamines important in depressive disorder.[3] RIMAs have not gained widespread market share in the United States.

Medical uses
MAOIs have been found to be effective in the treatment of
MAOIs can also be used in the treatment of Parkinson's disease by targeting MAO-B in particular (therefore affecting
MAOIs appear to be particularly indicated for
Newer MAOIs such as selegiline (typically used in the treatment of Parkinson's disease) and the reversible MAOI moclobemide provide a safer alternative[19] and are now sometimes used as first-line therapy.
Side effects
Hypertensive crisis
People taking MAOIs generally need to change their diets to limit or avoid foods and beverages containing
RIMAs are displaced from MAO-A in the presence of
Drug interactions
The most significant risk associated with the use of MAOIs is the potential for
Tryptophan supplements can be consumed with MAOIs, but can result in transient serotonin syndrome.[28]
MAOIs should not be combined with other psychoactive substances (antidepressants, painkillers, stimulants, including prescribed, OTC and illegally acquired drugs, etc.) except under expert care. Certain combinations can cause lethal reactions; common examples including
While safer than general MAOIs, RIMAs still possess significant and potentially serious drug interactions with many common drugs; in particular, they can cause
Ocular
Withdrawal
MAOIs, as with most antidepressant medication, may not alter the course of the disorder in a significant, permanent way, so it is possible that discontinuation can return the patient to the pre-treatment state.[37] This consideration complicates prescribing between an MAOI and an SSRI, because it is necessary to clear the system completely of one drug before starting another. One physician organization recommends the dose to be tapered down over a minimum of four weeks, followed by a two-week washout period.[38] The result is that a depressed patient will have to bear the depression without chemical help during the drug-free interval. This may be preferable to risking the effects of an interaction between the two drugs.[38]
Mechanism of action
MAOIs act by inhibiting the activity of
Reversibility
The early MAOIs covalently bound to the monoamine oxidase enzymes, thus inhibiting them irreversibly; the bound enzyme could not function and thus enzyme activity was blocked until the cell made new enzymes. The enzymes turn over approximately every two weeks. A few newer MAOIs, a notable one being
Harmaline found in Peganum harmala, Banisteriopsis caapi, and Passiflora incarnata is a reversible inhibitor of monoamine oxidase A (RIMA).[40]
Selectivity
In addition to reversibility, MAOIs differ by their selectivity of the MAO enzyme subtype. Some MAOIs inhibit both MAO-A and MAO-B equally, other MAOIs have been developed to target one over the other.
MAO-A inhibition reduces the breakdown of primarily serotonin, norepinephrine, and dopamine; selective inhibition of MAO-A allows for tyramine to be metabolised via MAO-B.[41] Agents that act on serotonin if taken with another serotonin-enhancing agent may result in a potentially fatal interaction called serotonin syndrome or with irreversible and unselective inhibitors (such as older MAOIs), of MAO a hypertensive crisis as a result of tyramine food interactions is particularly problematic with older MAOIs. Tyramine is broken down by MAO-A and MAO-B, therefore inhibiting this action may result in its excessive build-up, so diet must be monitored for tyramine intake.
MAO-B inhibition reduces the breakdown mainly of dopamine and phenethylamine so there are no dietary restrictions associated with this. MAO-B would also metabolize tyramine, as the only differences between dopamine, phenethylamine, and tyramine are two phenylhydroxyl groups on carbons 3 and 4. The 4-OH would not be a steric hindrance to MAO-B on tyramine.[42] Selegiline is selective for MAO-B at low doses, but non-selective at higher doses.
History
The knowledge of MAOIs began with the serendipitous discovery that iproniazid was a potent MAO inhibitor (MAOI).[43] Originally intended for the treatment of tuberculosis, in 1952, iproniazid's antidepressant properties were discovered when researchers noted that the depressed patients given iproniazid experienced a relief of their depression. Subsequent in vitro work led to the discovery that it inhibited MAO and eventually to the monoamine theory of depression. MAOIs became widely used as antidepressants in the early 1950s. The discovery of the 2 isoenzymes of MAO has led to the development of selective MAOIs that may have a more favorable side-effect profile.[44]
The older MAOIs' heyday was mostly between the years 1957 and 1970.
A transdermal patch form of the MAOI
List of MAO inhibiting drugs
Marketed MAOIs
- Nonselective MAO-A/MAO-B inhibitors
- Hydrazine (antidepressant)
- Isocarboxazid (Marplan)
- Hydracarbazine
- Phenelzine (Nardil, Nardelzine)
- Non-hydrazines
- Tranylcypromine (Parnate, Jatrosom)
- Hydrazine (antidepressant)
- Selective MAO-A inhibitors
- Bifemelane (Alnert, Celeport) (available in Japan)
- Methylene blue (Urelene blue, Provayblue, Proveblue)
- Moclobemide (Aurorix, Manerix, Moclamine)
- Pirlindole (Pirazidol) (available in Russia)
- Selective MAO-B inhibitors
- Rasagiline (Azilect)
- Selegiline (Deprenyl, Eldepryl, Emsam, Zelapar)
- Safinamide (Xadago)
Linezolid is an antibiotic drug with weak, reversible MAO-inhibiting activity.[49]
The antibiotic furazolidone also has MAO-inhibiting activity [50]
The Food and Drug Administration (FDA) has approved these MAOIs to treat depression:[52]
- Isocarboxazid (Marplan)
- Phenelzine (Nardil)
- Selegiline (Emsam)
- Tranylcypromine (Parnate)
MAOIs that have been withdrawn from the market
- Nonselective MAO-A/MAO-B inhibitors
- Hydrazines
- Benmoxin (Nerusil, Neuralex)
- Iproclozide (Sursum)
- Iproniazid (Marsilid, Iprozid, Ipronid, Rivivol, Propilniazida)
- Mebanazine (Actomol)
- Nialamide (Niamid)
- Octamoxin (Ximaol, Nimaol)
- Pheniprazine (Catron)
- Phenoxypropazine (Drazine)
- Pivalylbenzhydrazine(Tersavid)
- Safrazine (Safra) (discontinued worldwide except for Japan)
- Non-hydrazines
- Caroxazone (Surodil, Timostenil)
- Hydrazines
- Selective MAO-A inhibitors
- Minaprine (Cantor)
- Toloxatone (Humoryl)
List of RIMAs
Marketed pharmaceuticals
- Moclobemide (Aurorix, Manerix, Moclamine)
Other pharmaceuticals
- Brofaromine (Consonar)
- Caroxazone (Surodil, Timostenil)
- Eprobemide (Befol)[53]
- Methylene blue
- Metralindole (Inkazan)
- Minaprine (Cantor)
- Pirlindole (Pirazidol)
Naturally occurring RIMAs in plants
Research compounds
- Amiflamine (FLA-336)
- Befloxatone (MD-370,503)
- Cimoxatone (MD-780,515)
- Esuprone
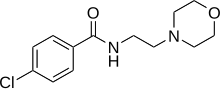
- Sercloremine (CGP-4718-A)
- Tetrindole
- CX157 (TriRima)
See also
References
- ^ Cristancho, Mario A. (20 November 2012). "Atypical Depression in the 21st Century: Diagnostic and Treatment Issues". Psychiatric Times. Archived from the original on 2 December 2013. Retrieved 23 November 2013.
- PMID 12968990.
- ^ "Neuroscience Education Institute > Activities > 2012CurbConsultPosted". www.neiglobal.com.
- PMID 3542985.
- PMID 1558463.
- S2CID 45341667.
- PMID 9862558.
- PMID 10232298.
- PMID 6375621.
- PMID 6388524.
- PMID 8124322.
- PMID 3900362.
- PMID 3282482.
- S2CID 10001735.
- PMID 8489326.
- S2CID 36232956.
- S2CID 31997372.
- PMID 19629023.
- ^ S2CID 30319319.
- )
- S2CID 52823188.
- from the original on 7 July 2017.
- ^ a b Mosher, Clayton James, and Scott Akins. Drugs and Drug Policy : The Control of Consciousness Alteration. Thousand Oaks, Calif.: Sage, 2007.[page needed]
- ^ a b Stahl S (2011). Case Studies: Stahl's Essential Psychopharmacology.
- PMID 10063483.
- ^ FDA. "EMSAM Medication Guide" (PDF). Food and Drug Administration. Archived (PDF) from the original on 10 October 2015.
- PMID 8313392.
- S2CID 37959124.
- ^ Pharmacology from H.P. Rang, M.M. Dale, J.M. Ritter, P.K. Moore, year 2003, chapter 38
- ^ "MHRA PAR Dextromethorphan hydrobromide, p. 12" (PDF). Archived (PDF) from the original on 10 May 2017.
- S2CID 235796130.)
{{cite journal}}: CS1 maint: multiple names: authors list (link - ^ PMID 11343627.
- ^ PMID 8943061.
- ^ S2CID 33217880.
- ISBN 978-0-7020-5572-0978-0-7020-5573-7 p. 332
- S2CID 14286356.
- PMID 18540740.
- ^ a b "Switching patients from phenelzine to other antidepressants". Royal Australian and New Zealand College of Psychiatrists. 11 May 2020. Retrieved 25 May 2020.
- PMID 19890267.
- ISBN 9780896037960.
- ^ PMID 9432289.
- PMID 17573034.
- PMID 21772661.
- S2CID 21625538.
- S2CID 46742172.
- PMID 7905288.
- PMID 8490690.
- ^ "FDA Approves Emsam (Selegiline) as First Drug Patch for Depression" (Press release). U.S. Food and Drug Administration. 28 February 2006. Archived from the original on 21 November 2009. Retrieved 19 November 2009.
- PMID 16652315.
- S2CID 35868007.
- PMID 22197611.
- ^ "An option if other antidepressants haven't helped". Mayo Clinic. Retrieved 9 December 2021.
- S2CID 29121452.
- PMID 19168123.
