Myocardial infarction
| Myocardial infarction | |
|---|---|
| Other names | Acute myocardial infarction (AMI), heart attack |
| Prognosis | STEMI 10% risk of death (developed world)[8] |
| Frequency | 15.9 million (2015)[10] |
A myocardial infarction (MI), commonly known as a heart attack, occurs when
Other symptoms may include
Most MIs occur due to
Treatment of an MI is time-critical.
Worldwide, about 15.9 million myocardial infarctions occurred in 2015.[10] More than 3 million people had an ST elevation MI, and more than 4 million had an NSTEMI.[18] STEMIs occur about twice as often in men as women.[19] About one million people have an MI each year in the United States.[3] In the developed world, the risk of death in those who have had a STEMI is about 10%.[8] Rates of MI for a given age have decreased globally between 1990 and 2010.[20] In 2011, an MI was one of the top five most expensive conditions during inpatient hospitalizations in the US, with a cost of about $11.5 billion for 612,000 hospital stays.[21]
Terminology
Myocardial infarction (MI) refers to tissue death (
The phrase "heart attack" is often used non-specifically to refer to myocardial infarction. An MI is different from—but can cause—cardiac arrest, where the heart is not contracting at all or so poorly that all vital organs cease to function, thus leading to death.[25] It is also distinct from heart failure, in which the pumping action of the heart is impaired. However, an MI may lead to heart failure.[26]
Signs and symptoms
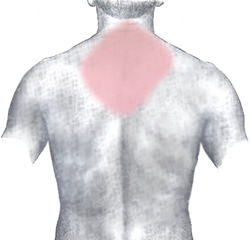
Chest pain that may or may not radiate to other parts of the body is the most typical and significant symptom of myocardial infarction. It might be accompanied by other symptoms such as sweating.[27]
Pain
Typically, chest pain because of ischemia, be it unstable angina or myocardial infarction, lessens with the use of
Other
Chest pain may be accompanied by
Other less common symptoms include weakness,
Absence
"Silent" myocardial infarctions can happen without any symptoms at all.
Risk factors
The most prominent risk factors for myocardial infarction are older age, actively
Many risk factors for myocardial infarction are potentially modifiable, with the most important being
Diet
There is varying evidence about the importance of
Genetics
Family history of
Other
The risk of having a myocardial infarction increases with older age, low physical activity, and low socioeconomic status.[45] Heart attacks appear to occur more commonly in the morning hours, especially between 6AM and noon.[56] Evidence suggests that heart attacks are at least three times more likely to occur in the morning than in the late evening.[57] Shift work is also associated with a higher risk of MI.[58] One analysis has found an increase in heart attacks immediately following the start of daylight saving time.[59]
Women who use
Endometriosis in women under the age of 40 is an identified risk factor.[62]
Air pollution is also an important modifiable risk. Short-term exposure to air pollution such as carbon monoxide, nitrogen dioxide, and sulfur dioxide (but not ozone) has been associated with MI and other acute cardiovascular events.[63] For sudden cardiac deaths, every increment of 30 units in Pollutant Standards Index correlated with an 8% increased risk of out-of-hospital cardiac arrest on the day of exposure.[64] Extremes of temperature are also associated.[65]
A number of acute and chronic
Calcium deposits in the coronary arteries can be detected with CT scans. Calcium seen in coronary arteries can provide predictive information beyond that of classical risk factors.[69] High blood levels of the amino acid homocysteine is associated with premature atherosclerosis;[70] whether elevated homocysteine in the normal range is causal is controversial.[71]
In people without evident
Mechanism
Atherosclerosis
The most common cause of a myocardial infarction is the rupture of an atherosclerotic plaque on an artery supplying heart muscle.[41][73] Plaques can become unstable, rupture, and additionally promote the formation of a blood clot that blocks the artery; this can occur in minutes. Blockage of an artery can lead to tissue death in tissue being supplied by that artery.[74] Atherosclerotic plaques are often present for decades before they result in symptoms.[74]
The gradual buildup of
Other causes
Atherosclerotic disease is not the only cause of myocardial infarction, but it may exacerbate or contribute to other causes. A myocardial infarction may result from a heart with a limited blood supply subject to increased oxygen demands, such as in fever,
Tissue death

If impaired blood flow to the heart lasts long enough, it triggers a process called the
Cells in the area with the worst blood supply, just below the inner surface of the heart (endocardium), are most susceptible to damage.[78][79] Ischemia first affects this region, the subendocardial region, and tissue begins to die within 15–30 minutes of loss of blood supply.[80] The dead tissue is surrounded by a zone of potentially reversible ischemia that progresses to become a full-thickness transmural infarct.[77][80] The initial "wave" of infarction can take place over 3–4 hours.[74][77] These changes are seen on gross pathology and cannot be predicted by the presence or absence of Q waves on an ECG.[79] The position, size and extent of an infarct depends on the affected artery, totality of the blockage, duration of the blockage, the presence of collateral blood vessels, oxygen demand, and success of interventional procedures.[28][73]
Tissue death and
Injury to the myocardium also occurs during re-perfusion. This might manifest as ventricular arrhythmia. The re-perfusion injury is a consequence of the calcium and sodium uptake from the cardiac cells and the release of oxygen radicals during reperfusion. No-reflow phenomenon—when blood is still unable to be distributed to the affected myocardium despite clearing the occlusion—also contributes to myocardial injury. Topical endothelial swelling is one of many factors contributing to this phenomenon.[82]
Diagnosis
Criteria
A myocardial infarction, according to current consensus, is defined by elevated cardiac
- Symptoms relating to ischemia
- Changes on an electrocardiogram (ECG), such as ST segment changes, new left bundle branch block, or pathologic Q waves
- Changes in the motion of the heart wall on imaging
- Demonstration of a thrombus on angiogram or at autopsy.
Types
A myocardial infarction is usually clinically classified as an ST-elevation MI (STEMI) or a non-ST elevation MI (NSTEMI). These are based on
- Spontaneous MI related to plaque erosion and/or rupture fissuring, or dissection
- MI related to ischemia, such as from increased oxygen demand or decreased supply, e.g., coronary artery spasm, coronary embolism, anemia, arrhythmias, high blood pressure, or low blood pressure
- Sudden unexpected cardiac death, including cardiac arrest, where symptoms may suggest MI, an ECG may be taken with suggestive changes, or a blood clot is found in a coronary artery by angiography and/or at autopsy, but where blood samples could not be obtained, or at a time before the appearance of cardiac biomarkers in the blood
- Associated with coronary angioplasty or stents
- Associated with percutaneous coronary intervention (PCI)
- Associated with stent thrombosis as documented by angiography or at autopsy
- Associated with CABG
- Associated with spontaneous coronary artery dissection in young, fit women
Cardiac biomarkers
There are many different biomarkers used to determine the presence of cardiac muscle damage. Troponins, measured through a blood test, are considered to be the best,[19] and are preferred because they have greater sensitivity and specificity for measuring injury to the heart muscle than other tests.[73] A rise in troponin occurs within 2–3 hours of injury to the heart muscle, and peaks within 1–2 days. The level of the troponin, as well as a change over time, are useful in measuring and diagnosing or excluding myocardial infarctions, and the diagnostic accuracy of troponin testing is improving over time.[73] One high-sensitivity cardiac troponin can rule out a heart attack as long as the ECG is normal.[84][85]
Other tests, such as
Electrocardiogram

ECG readouts product a waveform with different labelled features.

Imaging
Noninvasive imaging plays an important role in the diagnosis and characterisation of myocardial infarction.
Medical societies and professional guidelines recommend that the physician confirm a person is at high risk for Chronic Coronary Syndrome before conducting diagnostic non-invasive imaging tests to make a diagnosis,[91][93][90] as such tests are unlikely to change management and result in increased costs.[91] Patients who have a normal ECG and who are able to exercise, for example, most likely do not merit routine imaging.[91]
-
Poor movement of the heart due to an MI as seen on ultrasound[94]
-
Pulmonary edema due to an MI as seen on ultrasound[94]
Differential diagnosis
There are many causes of
Prevention
There is a large crossover between the lifestyle and activity recommendations to prevent a myocardial infarction, and those that may be adopted as
Primary prevention
Lifestyle
Physical activity can reduce the risk of cardiovascular disease, and people at risk are advised to engage in 150 minutes of moderate or 75 minutes of vigorous intensity aerobic exercise a week.[99] Keeping a healthy weight, drinking alcohol within the recommended limits, and quitting smoking reduce the risk of cardiovascular disease.[99]
Substituting
Public health measures may also act at a population level to reduce the risk of myocardial infarction, for example by reducing unhealthy diets (excessive salt, saturated fat, and trans-fat) including food labeling and marketing requirements as well as requirements for catering and restaurants and stimulating physical activity. This may be part of regional cardiovascular disease prevention programs or through the health impact assessment of regional and local plans and policies.[102]
Most guidelines recommend combining different preventive strategies. A 2015 Cochrane Review found some evidence that such an approach might help with
Medication
Statins, drugs that act to lower blood cholesterol, decrease the incidence and mortality rates of myocardial infarctions.[104] They are often recommended in those at an elevated risk of cardiovascular diseases.[99]
Aspirin has been studied extensively in people considered at increased risk of myocardial infarction. Based on numerous studies in different groups (e.g. people with or without diabetes), there does not appear to be a benefit strong enough to outweigh the risk of excessive bleeding.
Secondary prevention
There is a large crossover between the lifestyle and activity recommendations to prevent a myocardial infarction, and those that may be adopted as
Medications
Following a heart attack, nitrates, when taken for two days, and ACE-inhibitors decrease the risk of death.[111] Other medications include:
Aspirin is continued indefinitely, as well as another antiplatelet agent such as clopidogrel or ticagrelor ("dual antiplatelet therapy" or DAPT) for up to twelve months.[109] If someone has another medical condition that requires anticoagulation (e.g. with warfarin) this may need to be adjusted based on risk of further cardiac events as well as bleeding risk.[109] In those who have had a stent, more than 12 months of clopidogrel plus aspirin does not affect the risk of death.[112]
Beta blocker therapy such as metoprolol or carvedilol is recommended to be started within 24 hours, provided there is no acute heart failure or heart block.[19][86] The dose should be increased to the highest tolerated.[109] Contrary to most guidelines, the use of beta blockers does not appear to affect the risk of death,[113][114] possibly because other treatments for MI have improved. When beta blocker medication is given within the first 24–72 hours of a STEMI no lives are saved. However, 1 in 200 people were prevented from a repeat heart attack, and another 1 in 200 from having an abnormal heart rhythm. Additionally, for 1 in 91 the medication causes a temporary decrease in the heart's ability to pump blood.[115]
Statin therapy has been shown to reduce mortality and subsequent cardiac events and should be commenced to lower LDL cholesterol. Other medications, such as ezetimibe, may also be added with this goal in mind.[73]
Other
A
First aid
Taking aspirin helps to reduce the risk of mortality in people with myocardial infarction.[118]
Management
A myocardial infarction requires immediate medical attention. Treatment aims to preserve as much heart muscle as possible, and to prevent further complications.
Pain
The pain associated with myocardial infarction is often treated with
Antithrombotics
There is varying evidence on the mortality benefits in NSTEMI. A 2014 review of P2Y12 inhibitors such as clopidogrel found they do not change the risk of death when given to people with a suspected NSTEMI prior to PCI,[123] nor do heparins change the risk of death.[124] They do decrease the risk of having a further myocardial infarction.[73][124]

Angiogram
Primary percutaneous coronary intervention (PCI) is the treatment of choice for STEMI if it can be performed in a timely manner, ideally within 90–120 minutes of contact with a medical provider.[73][125] Some recommend it is also done in NSTEMI within 1–3 days, particularly when considered high-risk.[73] A 2017 review, however, did not find a difference between early versus later PCI in NSTEMI.[126]
PCI involves small probes, inserted through peripheral blood vessels such as the
Fibrinolysis
If PCI cannot be performed within 90 to 120 minutes in STEMI then fibrinolysis, preferably within 30 minutes of arrival to hospital, is recommended.
Other
In the past, high flow oxygen was recommended for everyone with a possible myocardial infarction.[86] More recently, no evidence was found for routine use in those with normal oxygen levels and there is potential harm from the intervention.[132][133][134][135][136] Therefore, oxygen is currently only recommended if oxygen levels are found to be low or if someone is in respiratory distress.[28][86]
If despite thrombolysis there is significant cardiogenic shock, continued severe chest pain, or less than a 50% improvement in ST elevation on the ECG recording after 90 minutes, then rescue PCI is indicated emergently.[137][138]
Those who have had
Rehabilitation and exercise
In the short-term, exercise-based cardiovascular rehabilitation programs may reduce the risk of a myocardial infarction, reduces a large number of hospitalizations from all causes, reduces hospital costs, improves
Prognosis
The prognosis after myocardial infarction varies greatly depending on the extent and location of the affected heart muscle, and the development and management of complications.[16] Prognosis is worse with older age and social isolation.[16] Anterior infarcts, persistent ventricular tachycardia or fibrillation, development of heart blocks, and left ventricular impairment are all associated with poorer prognosis.[16] Without treatment, about a quarter of those affected by MI die within minutes and about forty percent within the first month.[16] Morbidity and mortality from myocardial infarction has, however, improved over the years due to earlier and better treatment:[30] in those who have a STEMI in the United States, between 5 and 6 percent die before leaving the hospital and 7 to 18 percent die within a year.[19]
It is unusual for babies to experience a myocardial infarction, but when they do, about half die.[143] In the short-term, neonatal survivors seem to have a normal quality of life.[143]
Complications
Complications may occur immediately following the myocardial infarction or may take time to develop.
Heart failure may develop as a long-term consequence, with an impaired ability of heart muscle to pump, scarring, and an increase in the size of the existing muscle. Aneurysm of the left ventricle myocardium develops in about 10% of MI and is itself a risk factor for heart failure, ventricular arrhythmia, and the development of clots.[16]
Risk factors for complications and death include age,
Epidemiology
Myocardial infarction is a common presentation of coronary artery disease. The World Health Organization estimated in 2004, that 12.2% of worldwide deaths were from ischemic heart disease;[147] with it being the leading cause of death in high- or middle-income countries and second only to lower respiratory infections in lower-income countries.[147] Worldwide, more than 3 million people have STEMIs and 4 million have NSTEMIs a year.[18] STEMIs occur about twice as often in men as women.[19]
Rates of death from ischemic heart disease (IHD) have slowed or declined in most high-income countries, although cardiovascular disease still accounted for one in three of all deaths in the US in 2008.[148] For example, rates of death from cardiovascular disease have decreased almost a third between 2001 and 2011 in the United States.[149]
In contrast, IHD is becoming a more common cause of death in the developing world. For example, in
Social determinants of health
Social determinants such as neighborhood disadvantage, immigration status, lack of social support, social isolation, and access to health services play an important role in myocardial infarction risk and survival.[151][152][153][154] Studies have shown that low socioeconomic status is associated with an increased risk of poorer survival. There are well-documented disparities in myocardial infarction survival by socioeconomic status, race, education, and census-tract-level poverty.[155]
Race: In the U.S.
Socioeconomic status: Among individuals who live in the low-socioeconomic (SES) areas, which is close to 25% of the US population, myocardial infarctions (MIs) occurred twice as often compared with people who lived in higher SES areas.[158]
Immigration status: In 2018 many lawfully present
Health care access: Lack of health insurance and financial concerns about accessing care were associated with delays in seeking emergency care for acute myocardial infarction which can have significant, adverse consequences on patient outcomes.[160]
Education: Researchers found that compared to people with
Society and culture
Depictions of heart attacks in popular media often include collapsing or loss of consciousness which are not common symptoms; these depictions contribute to widespread misunderstanding about the symptoms of myocardial infarctions, which in turn contributes to people not getting care when they should.[162]
Legal implications
At
References
- ^ a b c d e f "What Are the Signs and Symptoms of Coronary Heart Disease?". www.nhlbi.nih.gov. September 29, 2014. Archived from the original on 24 February 2015. Retrieved 23 February 2015.
- ^ "Heart Attack Symptoms in Women". American Heart Association.
- ^ a b c d e f "What Is a Heart Attack?". www.nhlbi.nih.gov. December 17, 2013. Archived from the original on 19 February 2015. Retrieved 24 February 2015.
- ^ a b "Heart Attack or Sudden Cardiac Arrest: How Are They Different?". www.heart.org. Jul 30, 2014. Archived from the original on 24 February 2015. Retrieved 24 February 2015.
- ^ PMID 25453985.
- ^ ISBN 978-92-4-156437-3. Archived(PDF) from the original on 2014-08-17.
- ^ a b c "How Is a Heart Attack Diagnosed?". www.nhlbi.nih.gov. December 17, 2013. Archived from the original on 24 February 2015. Retrieved 24 February 2015.
- ^ PMID 22922416.
- ^ PMID 20956226.
- ^ PMID 27733282.
- PMID 22000678.
- ^ PMID 21497307.
- ^ "What Causes a Heart Attack?". www.nhlbi.nih.gov. December 17, 2013. Archived from the original on 18 February 2015. Retrieved 24 February 2015.
- PMID 18279535.
- ^ "Electrocardiogram". NHLBI, NIH. 9 December 2016. Archived from the original on 11 April 2017. Retrieved 10 April 2017.
- ^ ISBN 978-0-7020-3085-7.
- PMID 21873419.
- ^ PMID 18707987.
- ^ PMID 23247304.
- PMID 24573351.
- ^ Torio C (August 2013). "National Inpatient Hospital Costs: The Most Expensive Conditions by Payer, 2011". HCUP. Archived from the original on 14 March 2017. Retrieved 1 May 2017.
- ^ Morrow & Braunwald 2016, pp. 1–3; Dwight 2016, p. 41.
- ^ Morrow & Braunwald 2016, pp. 1–3.
- ^ PMID 22923432.
- ^ Blumenthal & Margolis 2007, pp. 4–5.
- ^ Morrow & Bohula 2016, p. 295.
- ^ Morrow 2016, pp. 59–61.
- ^ OCLC 923181481.
- ^ a b c Morrow 2016, pp. 59–60.
- ^ OCLC 923181481.
- PMID 27475013.
- PMID 17208083.
- ^ Allison & Murphy 2012, p. 197; Morrow 2016, p. 60.
- PMID 18071161.
- ^ "Heart Attack Symptoms, Risk, and Recovery". CDC.gov. U.S. Department of Health & Human Services. Retrieved July 20, 2021.
- PMID 22000678.
- PMID 16027643.
- PMID 12122387.
- ^ Ashton R, Raman D. "Dyspnea". www.clevelandclinicmeded.com. Cleveland Clinic. Archived from the original on 11 July 2017. Retrieved 24 May 2017.
- ISBN 978-1-4698-1668-5. Archivedfrom the original on 2017-07-28.
- ^ PMID 19004841.
- S2CID 12567614.
- ISBN 978-0-7817-4733-2.
- ^ Gaziano & Gaziano 2016, p. 11-22.
- ^ PMID 22555213.
- PMID 16697342.
- ^ PMID 22981903.
- PMID 22818936.
- S2CID 27925226.
- ^ PMID 32827219.
- ^ PMID 24723079.
- PMID 26268692.
- ^ "Scientific Report of the 2015 Dietary Guidelines Advisory Committee" (PDF). health.gov. Feb 2015. p. 17. Archived from the original (PDF) on 2016-05-03. Retrieved 2015-03-05.
- PMID 22041278.
- ^ PMID 22129254.
- PMID 16860887.
- S2CID 43626425.
- PMID 22835925.
- S2CID 205040478.
- PMID 26310586.
- PMID 28487435.
- PMID 27025928.
- PMID 22337682.
- S2CID 52282745.
- S2CID 51705159.
- ^ PMID 23030426.
- PMID 23016720.
- PMID 24485156.
- PMID 21145688.
- S2CID 8714058.
- S2CID 8734056.
- PMID 28158518.
- ^ S2CID 33523662.
- ^ ISBN 978-0-7020-3085-7.
- PMID 20065951.
- PMID 26705388.
- ^ PMID 16009313.
- PMID 21169398.
- ^ a b Bolooki HM, Askari A (August 2010). "Acute Myocardial Infarction". www.clevelandclinicmeded.com. Archived from the original on 28 April 2017. Retrieved 24 May 2017.
- ^ ISBN 978-0-470-65594-8.
- PMID 24188218.
- ISBN 978-0-323-35943-6.
- PMID 30165617.
- PMID 28418520.
- PMID 29127948.
- ^ PMID 25249585.
- PMID 24731654.
- ^ ISBN 978-0-7020-3085-7.
- OCLC 923181481.
- ^ PMID 32860058.
- ^ a b c d "American College of Cardiology". www.choosingwisely.org. Choosing Wisely. 28 February 2017. Archived from the original on 28 July 2017. Retrieved 24 May 2017.
- PMID 20542817.
- National Institute for Health and Clinical Excellence. Clinical guideline cg94: Unstable angina and NSTEMI. London, 2010.
- ^ a b "UOTW #36 – Ultrasound of the Week". Ultrasound of the Week. 5 February 2015. Archived from the original on 9 May 2017. Retrieved 27 May 2017.
- ^ ISBN 978-0-7020-3085-7.
- PMID 16199332.
- ^ "Assessment of fatigue". BMJ Best Practice. 17 August 2016. Archived from the original on 28 August 2021. Retrieved 6 June 2017.
- PMID 27686519.
- ^ National Institute for Health and Clinical Excellence. Clinical guideline 181: Lipid modification: cardiovascular risk assessment and the modification of blood lipids for the primary and secondary prevention of cardiovascular disease. London, 2014.
- PMID 24993125.
- S2CID 17366251.
- ^ McPherson K, et al. (June 2010). "Prevention of cardiovascular disease – NICE public health guidance 25". London: National Institute for Health and Care Excellence. Archived from the original on 2014-03-29.
- PMID 21249647.
- PMID 23440795.
- PMID 19482214.
- PMID 24074752.
- S2CID 28350632.
- S2CID 30838065.
- ^ National Institute for Health and Clinical Excellence. Clinical guideline 172: Secondary prevention in primary and secondary care for patients following a myocardial infarction. London, 2013.
- PMID 25503364.
- PMID 19821384.
- PMID 25467565.
- PMID 24927909.
- PMID 31845756.
- ^ Newman D (19 August 2010). "Beta Blockers for Acute Heart Attack (Myocardial Infarction)". TheNNT.com. Archived from the original on 22 December 2015. Retrieved 11 December 2015.
- PMID 26891235.
- PMID 26472854.
- PMID 27502078.
- PMID 20530163.
- ^ Reeder G (27 December 2016). "Nitrates in the management of acute coronary syndrome". www.uptodate.com. Archived from the original on 28 July 2017. Retrieved 24 May 2017.
- S2CID 23759756.
- PMID 27264228.
- PMID 25954988.
- ^ PMID 24972265.
- PMID 24902975.
- S2CID 4489347.
- PMID 20802248.
- S2CID 46847680.
- S2CID 21955018.
- PMID 26472989.
- PMID 25208209.
- PMID 27991651.
- PMID 28844200.
- PMID 29355510.
- S2CID 4472549.
- ^ Singh A, Hussain S, Antony B (2020). "How Much Evidence Is Needed to Conclude against the Use of Oxygen Therapy in Acute Myocardial Infarction?". Res Pract Thromb Haemost. 4 (Suppl 1). Retrieved 28 July 2020.
- ISBN 978-1-4443-9387-3.
- ISBN 978-93-5025-073-0.
- PMID 29799995.
- S2CID 4277993.
- S2CID 25806176.
- PMID 34741536.
- ^ S2CID 20779415.
- S2CID 10268606.
- PMID 17032691.
- PMID 16698331.
- ^ ISBN 978-92-4-156371-0.
- PMID 22215894.
- PMID 25520374.
From 2001 to 2011, death rates attributable to CVD declined 30.8%.
- S2CID 27117207.
- PMID 25011538.
- PMID 11413176.
- PMID 26369354.
- PMID 26585783.
- PMID 18621776.
- PMID 25418513.
- PMID 17227980. Retrieved 2023-11-16.
- PMID 32459344.
- ^ "Health Coverage of Immigrants". KFF. 2020-03-18. Retrieved 2021-04-09.
- PMID 20388895.
- PMID 31476920.
- PMID 11410572.
- ^ Workers' Compensation FAQ Archived 2007-07-11 at the Wayback Machine. Prairie View A&M University. Retrieved November 22, 2006.
- ^ SIGNIFICANT DECISIONS Subject Index Archived 2006-12-06 at the Wayback Machine. Board of Industrial Insurance Appeals. Retrieved November 22, 2006.
- ^ "Classification of Drivers' Licenses Regulations". Nova Scotia Registry of Regulations. May 24, 2000. Archived from the original on April 20, 2007. Retrieved April 22, 2007.
Sources
- Allison TG, Murphy JG (6 December 2012). "Stress Test Selection". In Murphy JG, Lloyd MA, Brady PA, Olsen LJ, Shields RC (eds.). Mayo Clinic Cardiology: Concise Textbook. OUP US. pp. 196–202. ISBN 978-0-19-991571-2.
- Blumenthal RS, Margolis S (2007). Heart Attack Prevention 2007. Johns Hopkins Health. ISBN 978-1-933087-47-4.
- Dwight J (16 June 2016). "Chest pain, breathlessness, fatigue". In Warrell D, Cox T, Firth J, Dwight J (eds.). Oxford Textbook of Medicine: Cardiovascular Disorders. Oxford University Press. pp. 39–47. ISBN 978-0-19-871702-7.
- Gaziano TA, Gaziano JM (15 September 2016). "Global Evolving Epidemiology, Natural History, and Treatment Trends of Myocardial Infarction". In Morrow DA (ed.). Myocardial Infarction: A Companion to Braunwald's Heart Disease. Elsevier. pp. 11–21. ISBN 978-0-323-35943-6.
- Morrow DA, Bohula EA (15 September 2016). "Heart Failure and Cardiogenic Shock After Myocardial Infarction". In Morrow DA (ed.). Myocardial Infarction: A Companion to Braunwald's Heart Disease. Elsevier. pp. 295–313. ISBN 978-0-323-35943-6.
- Morrow DA, Braunwald E (15 September 2016). "Classification and Diagnosis of Acute Coronary Syndromes". In Morrow DA (ed.). Myocardial Infarction: A Companion to Braunwald's Heart Disease. Elsevier. pp. 1–10. ISBN 978-0-323-35943-6.
- Morrow DA (15 September 2016). "Clinical Approach to Suspected Acute Myocardial Infarction". In Morrow DA (ed.). Myocardial Infarction: A Companion to Braunwald's Heart Disease. Elsevier. pp. 55–65. ISBN 978-0-323-35943-6.
Further reading
- Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, et al. (March 2016). "2015 ACC/AHA/SCAI Focused Update on Primary Percutaneous Coronary Intervention for Patients With ST-Elevation Myocardial Infarction: An Update of the 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention and the 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Society for Cardiovascular Angiography and Interventions". Circulation. 133 (11): 1135–47. PMID 26490017.
- Min Cho, S., et al. (2021). "Machine learning compared with conventional statistical models for predicting myocardial infarction readmission and mortality: a systematic review". Canadian Journal of Cardiology. 37 (8). Elsevier: 1207–1214. S2CID 232141652.
External links
- Myocardial infarction at Curlie
- American Heart Association's Heart Attack web site — Information and resources for preventing, recognizing, and treating a heart attack.
- TIMI Score for UA/NSTEMI Archived 2016-11-05 at the Wayback Machine and STEMI Archived 2009-03-19 at the Wayback Machine
- HEART Score for Major Cardiac Events Archived 2016-10-28 at the Wayback Machine
- "Heart Attack". MedlinePlus. U.S. National Library of Medicine.