SARS-CoV-2
| Severe acute respiratory syndrome coronavirus 2 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|

| |||||||||||
| Colourised transmission electron micrograph of SARS-CoV-2 virions with visible coronae | |||||||||||
| |||||||||||
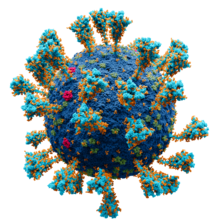
Model of the external structure of the SARS-CoV-2 virion[1]
| |||||||||||
| Virus classification | |||||||||||
| (unranked): | Virus | ||||||||||
| Realm: | Riboviria | ||||||||||
| Kingdom: | Orthornavirae | ||||||||||
| Phylum: | Pisuviricota | ||||||||||
| Class: | Pisoniviricetes | ||||||||||
| Order: | Nidovirales | ||||||||||
| Family: | Coronaviridae | ||||||||||
| Genus: | Betacoronavirus | ||||||||||
| Subgenus: | Sarbecovirus | ||||||||||
| Species: | Severe acute respiratory syndrome–related coronavirus | ||||||||||
| Virus: | Severe acute respiratory syndrome coronavirus 2
| ||||||||||
| Notable variants | |||||||||||
| Synonyms | |||||||||||
| |||||||||||
| Part of a series on the |
| COVID-19 pandemic |
|---|
 |
|
|
|
Severe acute respiratory syndrome coronavirus 2 (SARS‑CoV‑2)
SARS‑CoV‑2 is a strain of the species
Terminology

During the initial outbreak in Wuhan, China, various names were used for the virus; some names used by different sources included "the coronavirus" or "Wuhan coronavirus".[27][28] In January 2020, the World Health Organization (WHO) recommended "2019 novel coronavirus" (2019-nCoV)[5][29] as the provisional name for the virus. This was in accordance with WHO's 2015 guidance[30] against using geographical locations, animal species, or groups of people in disease and virus names.[31][32]
On 11 February 2020, the International Committee on Taxonomy of Viruses adopted the official name "severe acute respiratory syndrome coronavirus 2" (SARS‑CoV‑2).[33] To avoid confusion with the disease SARS, the WHO sometimes refers to SARS‑CoV‑2 as "the COVID-19 virus" in public health communications[34][35] and the name HCoV-19 was included in some research articles.[8][9][10] Referring to COVID-19 as the "Wuhan virus" has been described as dangerous by WHO officials, and as xenophobic by many journalists and academics.[36][37][38]
Infection and transmission
This section has multiple issues. Please help improve it or discuss these issues on the talk page. (Learn how and when to remove these template messages)
|
Human-to-human
The degree to which the virus is infectious during the incubation period is uncertain, but research has indicated that the pharynx reaches peak viral load approximately four days after infection[61][62] or in the first week of symptoms and declines thereafter.[63] The duration of SARS-CoV-2 RNA shedding is generally between 3 and 46 days after symptom onset.[64]
A study by a team of researchers from the University of North Carolina found that the nasal cavity is seemingly the dominant initial site of infection, with subsequent aspiration-mediated virus-seeding into the lungs in SARS‑CoV‑2 pathogenesis.[65] They found that there was an infection gradient from high in proximal towards low in distal pulmonary epithelial cultures, with a focal infection in ciliated cells and type 2 pneumocytes in the airway and alveolar regions respectively.[65]
Studies have identified a range of animals—such as cats, ferrets, hamsters, non-human primates, minks, tree shrews, raccoon dogs, fruit bats, and rabbits—that are susceptible and permissive to SARS-CoV-2 infection.[66][67][68] Some institutions have advised that those infected with SARS‑CoV‑2 restrict their contact with animals.[69][70]
Asymptomatic and presymptomatic transmission
On 1 February 2020, the World Health Organization (WHO) indicated that "transmission from asymptomatic cases is likely not a major driver of transmission".[71] One meta-analysis found that 17% of infections are asymptomatic, and asymptomatic individuals were 42% less likely to transmit the virus.[72]
However, an epidemiological model of the beginning of the
Reinfection
There is uncertainty about reinfection and long-term immunity.[76] It is not known how common reinfection is, but reports have indicated that it is occurring with variable severity.[76]
The first reported case of reinfection was a 33-year-old man from Hong Kong who first tested positive on 26 March 2020, was discharged on 15 April 2020 after two negative tests, and tested positive again on 15 August 2020 (142 days later), which was confirmed by whole-genome sequencing showing that the viral genomes between the episodes belong to different clades.[77] The findings had the implications that herd immunity may not eliminate the virus if reinfection is not an uncommon occurrence and that vaccines may not be able to provide lifelong protection against the virus.[77]
Another case study described a 25-year-old man from Nevada who tested positive for SARS‑CoV‑2 on 18 April 2020 and on 5 June 2020 (separated by two negative tests). Since genomic analyses showed significant genetic differences between the SARS‑CoV‑2 variant sampled on those two dates, the case study authors determined this was a reinfection.[78] The man's second infection was symptomatically more severe than the first infection, but the mechanisms that could account for this are not known.[78]
Reservoir and origin

No
The first known infections from SARS‑CoV‑2 were discovered in Wuhan, China.
For a virus recently acquired through a cross-species transmission, rapid evolution is expected.[88] The mutation rate estimated from early cases of SARS-CoV-2 was of 6.54×10−4 per site per year.[86] Coronaviruses in general have high genetic plasticity,[89] but SARS-CoV-2's viral evolution is slowed by the RNA proofreading capability of its replication machinery.[90] For comparison, the viral mutation rate in vivo of SARS-CoV-2 has been found to be lower than that of influenza.[91]
Research into the natural reservoir of the virus that caused the

Bats are considered the most likely natural reservoir of SARS‑CoV‑2.[86][97] Differences between the bat coronavirus and SARS‑CoV‑2 suggest that humans may have been infected via an intermediate host;[84] although the source of introduction into humans remains unknown.[98][79]
Although the role of
Phylogenetics and taxonomy
Genomic organisation of isolate Wuhan-Hu-1, the earliest sequenced sample of SARS-CoV-2 | |
| NCBI genome ID | 86693 |
|---|---|
| Genome size | 29,903 bases |
| Year of completion | 2020 |
| Genome browser (UCSC) | |
SARS‑CoV‑2 belongs to the broad family of viruses known as
Like the SARS-related coronavirus implicated in the 2003 SARS outbreak, SARS‑CoV‑2 is a member of the subgenus
A distinguishing feature of SARS‑CoV‑2 is its incorporation of a polybasic site cleaved by furin,[102][112] which appears to be an important element enhancing its virulence.[113] It was suggested that the acquisition of the furin-cleavage site in the SARS-CoV-2 S protein was essential for zoonotic transfer to humans.[114] The furin protease recognizes the canonical peptide sequence RX[R/K] R↓X where the cleavage site is indicated by a down arrow and X is any amino acid.[115][116] In SARS-CoV-2 the recognition site is formed by the incorporated 12 codon nucleotide sequence CCT CGG CGG GCA which corresponds to the amino acid sequence P RR A.[117] This sequence is upstream of an arginine and serine which forms the S1/S2 cleavage site (P RR A R↓S) of the spike protein.[118] Although such sites are a common naturally-occurring feature of other viruses within the Subfamily Orthocoronavirinae,[117] it appears in few other viruses from the Beta-CoV genus,[119] and it is unique among members of its subgenus for such a site.[102] The furin cleavage site PRRAR↓ is highly similar to that of the feline coronavirus, an alphacoronavirus 1 strain.[120]
Viral genetic sequence data can provide critical information about whether viruses separated by time and space are likely to be epidemiologically linked.
On 11 February 2020, the
In July 2020, scientists reported that a more infectious SARS‑CoV‑2 variant with spike protein variant G614 has replaced D614 as the dominant form in the pandemic.[127][128]
Coronavirus genomes and subgenomes encode six open reading frames (ORFs).[129] In October 2020, researchers discovered a possible overlapping gene named ORF3d, in the SARS‑CoV‑2 genome. It is unknown if the protein produced by ORF3d has any function, but it provokes a strong immune response. ORF3d has been identified before, in a variant of coronavirus that infects pangolins.[130][131]
Phylogenetic tree
A phylogenetic tree based on whole-genome sequences of SARS-CoV-2 and related coronaviruses is:[132][133]
| SARS‑CoV‑2 related coronavirus | |
|
SARS-CoV-1 , 79% to SARS-CoV-2
| |
Variants
This section needs to be updated. (April 2023) |

There are many thousands of variants of SARS-CoV-2, which can be grouped into the much larger
Several notable variants of SARS-CoV-2 emerged in late 2020. The
- P681H.
- An E484K mutation in some lineage B.1.1.7 virions has been noted and is also tracked by various public health agencies.
- An
- K417N, E484K and N501Y.
- Gamma: Lineage P.1 emerged in Brazil in November 2020, also with evidence of increased transmissibility and virulence, alongside changes to antigenicity. Similar concerns about vaccine efficacy have been raised. Notable mutations also include K417N, E484K and N501Y.
- Delta: Lineage B.1.617.2 emerged in India in October 2020. There is also evidence of increased transmissibility and changes to antigenicity.
- Omicron: Lineage B.1.1.529 emerged in Botswana in November 2021.
Other notable variants include 6 other WHO-designated variants under investigation and Cluster 5, which emerged among mink in Denmark and resulted in a mink euthanasia campaign rendering it virtually extinct.[145]
Virology
Virus structure
Each SARS-CoV-2
Genome
As of early 2022, about 7 million SARS-CoV-2 genomes had been sequenced and deposited into public databases and another 800,000 or so were added each month.[151] By September 2023, the GISAID EpiCoV database contained more than 16 million genome sequences.[152]
SARS-CoV-2 has a linear,
Replication cycle
Virus infections start when viral particles bind to host surface cellular receptors.
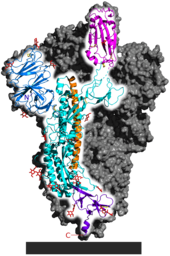
Initial spike protein priming by
SARS‑CoV‑2 produces at least three
Treatment and drug development
Very few drugs are known to effectively inhibit SARS‑CoV‑2.
Epidemiology
Retrospective tests collected within the Chinese surveillance system revealed no clear indication of substantial unrecognized circulation of SARS‑CoV‑2 in Wuhan during the latter part of 2019.[86]
A meta-analysis from November 2020 estimated the basic reproduction number () of the virus to be between 2.39 and 3.44.
| Variant | R0 | Source |
|---|---|---|
| Reference/ancestral strain | ~2.8 | [177] |
| Alpha (B.1.1.7) | (40-90% higher than previous variants) | [178] |
| Delta (B.1.617.2) | ~5 (3-8) | [179] |
There have been about 96,000 confirmed cases of infection in mainland China.[180] While the proportion of infections that result in confirmed cases or progress to diagnosable disease remains unclear,[181] one mathematical model estimated that 75,815 people were infected on 25 January 2020 in Wuhan alone, at a time when the number of confirmed cases worldwide was only 2,015.[182] Before 24 February 2020, over 95% of all deaths from COVID-19 worldwide had occurred in Hubei province, where Wuhan is located.[183][184] As of 10 March 2023, the percentage had decreased to 0.047%.[180]
As of 10 March 2023, there were 676,609,955 total confirmed cases of SARS‑CoV‑2 infection.[180] The total number of deaths attributed to the virus was 6,881,955.[180]
See also
- 3C-like protease (NS5)
References
- ^ Solodovnikov A, Arkhipova V (29 July 2021). "Достоверно красиво: как мы сделали 3D-модель SARS-CoV-2" [Truly beautiful: how we made the SARS-CoV-2 3D model] (in Russian). N+1. Archived from the original on 30 July 2021. Retrieved 30 July 2021.
- ^ Zimmer C (26 February 2021). "The Secret Life of a Coronavirus – An oily, 100-nanometer-wide bubble of genes has killed more than two million people and reshaped the world. Scientists don't quite know what to make of it". The New York Times. Archived from the original on 27 February 2021. Retrieved 28 February 2021.
- hdl:10665/330376. WHO/2019-nCoV/Surveillance/v2020.1.
- ^ a b "Healthcare Professionals: Frequently Asked Questions and Answers". United States Centers for Disease Control and Prevention (CDC). 11 February 2020. Archived from the original on 14 February 2020. Retrieved 15 February 2020.
- ^ "About Novel Coronavirus (2019-nCoV)". United States Centers for Disease Control and Prevention (CDC). 11 February 2020. Archived from the original on 11 February 2020. Retrieved 25 February 2020.
- ^ Harmon A (4 March 2020). "We Spoke to Six Americans with Coronavirus". The New York Times. Archived from the original on 13 March 2020. Retrieved 16 March 2020.
- ^ PMID 32314559.
- ^ PMID 32284615.
- ^ PMID 32182409.
- ^ "hCoV-19 Database". China National GeneBank. Archived from the original on 17 June 2020. Retrieved 2 June 2020.
- ^ Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV). World Health Organization (WHO). 30 January 2020. Archived from the original on 31 January 2020. Retrieved 30 January 2020.
- ^ WHO Director-General's opening remarks at the media briefing on COVID-19 – 11 March 2020. World Health Organization (WHO). 11 March 2020. Archived from the original on 11 March 2020. Retrieved 12 March 2020.
- ^ Rigby J, Satija B (5 May 2023). "WHO declares end to COVID global health emergency". Reuters. Retrieved 6 May 2023.
- PMID 32696264.
- ^ PMID 31986261.
- ^ "New coronavirus stable for hours on surfaces". National Institutes of Health (NIH). NIH.gov. 17 March 2020. Archived from the original on 23 March 2020. Retrieved 4 May 2020.
- ^ PMID 33116300.
- hdl:10665/330991.
- ^ S2CID 214574620.
- ^ PMID 33175914.
- ^ "COVID-19 variants: What's the concern?". Mayo Clinic. 27 August 2022. Retrieved 10 October 2022.
- ^ "How Coronavirus Spreads Archived 3 April 2020 at the Wayback Machine", Centers for Disease Control and Prevention, Retrieved 14 May 2021.
- ^ "Coronavirus disease (COVID-19): How is it transmitted? Archived 15 October 2020 at the Wayback Machine", World Health Organization
- ^ PMID 32142651.
- PMID 32841605.
- ^ Huang P (22 January 2020). "How Does Wuhan Coronavirus Compare with MERS, SARS and the Common Cold?". NPR. Archived from the original on 2 February 2020. Retrieved 3 February 2020.
- ^ S2CID 213064026.
- hdl:10665/330775.
- ^ "World Health Organization Best Practices for the Naming of New Human Infectious Diseases" (PDF). WHO. May 2015. Archived (PDF) from the original on 12 February 2020.
- ^ "Novel coronavirus named 'Covid-19': WHO". TODAYonline. Archived from the original on 21 March 2020. Retrieved 11 February 2020.
- ^ "The coronavirus spreads racism against—and among—ethnic Chinese". The Economist. 17 February 2020. Archived from the original on 17 February 2020. Retrieved 17 February 2020.
- ^ "Naming the coronavirus disease (COVID-2019) and the virus that causes it". World Health Organization. Archived from the original on 28 February 2020. Retrieved 14 December 2020.
ICTV announced "severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)" as the name of the new virus on 11 February 2020. This name was chosen because the virus is genetically related to the coronavirus responsible for the SARS outbreak of 2003. While related, the two viruses are different.
- ^ Hui M (18 March 2020). "Why won't the WHO call the coronavirus by its name, SARS-CoV-2?". Quartz. Archived from the original on 25 March 2020. Retrieved 26 March 2020.
- ^ "Naming the coronavirus disease (COVID-2019) and the virus that causes it". World Health Organization. Archived from the original on 28 February 2020. Retrieved 14 December 2020.
From a risk communications perspective, using the name SARS can have unintended consequences in terms of creating unnecessary fear for some populations. ... For that reason and others, WHO has begun referring to the virus as "the virus responsible for COVID-19" or "the COVID-19 virus" when communicating with the public. Neither of these designations is [sic] intended as replacements for the official name of the virus as agreed by the ICTV.
- ^ "Standing Up to Hate and Bias Related to COVID-19". National Education Association. 5 June 2020.
It's racist and it creates xenophobia," University of California at Berkeley Asian American studies lecturer Harvey Dong told The Washington Post. "It's a very dangerous situation."
- ^ Gstalter M (19 March 2020). "WHO official warns against calling it 'Chinese virus,' says 'there is no blame in this'". The Hill. Retrieved 15 September 2022.
Ryan is not the first WHO official to push back against the phrase. Director-General Tedros Adhanom Ghebreyesus said earlier this month that the term is "painful to see" and "more dangerous than the virus itself."
- PMID 32837171.
- PMID 32087334.
- ^ Kessler G (17 April 2020). "Trump's false claim that the WHO said the coronavirus was 'not communicable'". The Washington Post. Archived from the original on 17 April 2020. Retrieved 17 April 2020.
- ^ Kuo L (21 January 2020). "China confirms human-to-human transmission of coronavirus". The Guardian. Archived from the original on 22 March 2020. Retrieved 18 April 2020.
- ^ "How COVID-19 Spreads". U.S. Centers for Disease Control and Prevention (CDC). 27 January 2020. Archived from the original on 28 January 2020. Retrieved 29 January 2020.
- ^ Edwards E (25 January 2020). "How does coronavirus spread?". NBC News. Archived from the original on 28 January 2020. Retrieved 13 March 2020.
- PMID 32294341.
- PMID 32404416.
- S2CID 220500293.
Investigators have demonstrated that speaking and coughing produce a mixture of both droplets and aerosols in a range of sizes, that these secretions can travel together for up to 27 feet, that it is feasible for SARS-CoV-2 to remain suspended in the air and viable for hours, that SARS-CoV-2 RNA can be recovered from air samples in hospitals, and that poor ventilation prolongs the amount of time that aerosols remain airborne.
- ^ Rettner R (21 January 2021). "Talking is worse than coughing for spreading COVID-19 indoors". Live Science. Retrieved 10 October 2022.
In one modeled scenario, the researchers found that after a short cough, the number of infectious particles in the air would quickly fall after 1 to 7 minutes; in contrast, after speaking for 30 seconds, only after 30 minutes would the number of infectious particles fall to similar levels; and a high number of particles were still suspended after one hour. In other words, a dose of virus particles capable of causing an infection would linger in the air much longer after speech than a cough. (In this modeled scenario, the same number of droplets were admitted during a 0.5-second cough as during the course of 30 seconds of speech.)
- S2CID 231643585.
- ^ Mandavilli A (4 July 2020). "239 Experts With One Big Claim: The Coronavirus Is Airborne – The W.H.O. has resisted mounting evidence that viral particles floating indoors are infectious, some scientists say. The agency maintains the research is still inconclusive". The New York Times. Archived from the original on 17 November 2020. Retrieved 5 July 2020.
- ^ Tufekci Z (30 July 2020). "We Need to Talk About Ventilation". The Atlantic. Archived from the original on 17 November 2020. Retrieved 8 September 2020.
- S2CID 220470431.
- PMID 33229462.
- ^ PMID 32296168.
- PMID 20497390.
- PMID 32289025.
- ^ "Getting your workplace ready for COVID-19" (PDF). World Health Organization. 27 February 2020. Archived (PDF) from the original on 2 March 2020. Retrieved 3 March 2020.
- ^ Yong E (20 March 2020). "Why the Coronavirus Has Been So Successful". The Atlantic. Archived from the original on 20 March 2020. Retrieved 20 March 2020.
- ^ Gibbens S (18 March 2020). "Why soap is preferable to bleach in the fight against coronavirus". National Geographic. Archived from the original on 2 April 2020. Retrieved 2 April 2020.
- PMID 32004427.
- PMID 32379329.
- PMID 32235945.
- S2CID 214094598.
- PMID 32213337.
- PMID 33248470.
- ^ PMID 32526206.
- PMID 33539765.
- ^ "Questions and Answers on the COVID-19: OIE – World Organisation for Animal Health". www.oie.int. Archived from the original on 31 March 2020. Retrieved 16 April 2020.
- ^ Goldstein J (6 April 2020). "Bronx Zoo Tiger Is Sick with the Coronavirus". The New York Times. Archived from the original on 9 April 2020. Retrieved 10 April 2020.
- ^ "USDA Statement on the Confirmation of COVID-19 in a Tiger in New York". United States Department of Agriculture. 5 April 2020. Archived from the original on 15 April 2020. Retrieved 16 April 2020.
- ^ "If You Have Animals—Coronavirus Disease 2019 (COVID-19)". Centers for Disease Control and Prevention (CDC). 13 April 2020. Archived from the original on 1 April 2020. Retrieved 16 April 2020.
- hdl:10665/330777.
- PMID 33214725.
- PMID 32179701.
- Daily Telegraph, Thursday 28 May 2020, page 2 column 1, which refers to the medical journal Thorax; Thorax May 2020 article COVID-19: in the footsteps of Ernest Shackleton Archived 30 May 2020 at the Wayback Machine
- PMID 32770170.
- ^ S2CID 221501940.
- ^ S2CID 221308584.
- ^ PMID 33058797.
- ^ PMID 34480864.
- ^ PMID 32015507.
- ^ Eschner K (28 January 2020). "We're still not sure where the Wuhan coronavirus really came from". Popular Science. Archived from the original on 30 January 2020. Retrieved 30 January 2020.
- PMID 31986264.
- ^ PMID 32007143.
- ^ PMID 32127703.
- PMID 32351056.
- ^ a b c d e Joint WHO-China Study Team (30 March 2021). WHO-convened global study of origins of SARS-CoV-2: China Part. Geneva, Switzerland: World Health Organization. Retrieved 31 May 2023.
- S2CID 244403410.
- PMID 34289344.
- PMID 32402329.
- PMID 32853546.
- PMID 34535792.
- S2CID 246902858.
- S2CID 237626322.
- ^ "Newly Discovered Bat Viruses Give Hints to Covid's Origins". The New York Times. 14 October 2021.
- ^ "Bat coronavirus isolate RaTG13, complete genome". National Center for Biotechnology Information (NCBI). 10 February 2020. Archived from the original on 15 May 2020. Retrieved 5 March 2020.
- ^ "The 'Occam's Razor Argument' Has Not Shifted in Favor of a Lab Leak". Snopes.com. Snopes. 16 July 2021. Retrieved 18 July 2021.
- PMID 32007145.
- ISBN 978-1-988234-54-0. Archivedfrom the original on 12 May 2021. Retrieved 12 May 2021.
- S2CID 218557880.
- PMID 33101254.
- ^ "Why it's so tricky to trace the origin of COVID-19". Science. National Geographic. 10 September 2021.
- ^ PMID 33024307.
- S2CID 226988090.
- ^ PMID 33116300.
- ^ PMID 31978945.
- ^ "Phylogeny of SARS-like betacoronaviruses". nextstrain. Archived from the original on 20 January 2020. Retrieved 18 January 2020.
- PMID 30791586.
- ^ PMID 33864026.
- S2CID 237099659.
- ^ a b "CoV2020". GISAID EpifluDB. Archived from the original on 12 January 2020. Retrieved 12 January 2020.
- PMID 32330414.
- S2CID 245430230.
- PMID 33666147.
- ^ PMID 34611326.
- PMID 31406574.
- PMID 32787225.
- ^ PMID 32057769.
- PMID 32197085.
- PMID 33340798.
- PMID 32912998.
- ^ "Initial genome release of novel coronavirus". Virological. 11 January 2020. Archived from the original on 12 January 2020. Retrieved 12 January 2020.
- ^ a b Bedford T, Neher R, Hadfield N, Hodcroft E, Ilcisin M, Müller N. "Genomic analysis of nCoV spread: Situation report 2020-01-30". nextstrain.org. Archived from the original on 15 March 2020. Retrieved 18 March 2020.
- PMID 32359479.
- ^ "Genomic epidemiology of novel coronavirus – Global subsampling". Nextstrain. 25 October 2021. Archived from the original on 20 April 2020. Retrieved 26 October 2021.
- PMID 32123347.
- ^ "New, more infectious strain of COVID-19 now dominates global cases of virus: study". medicalxpress.com. Archived from the original on 17 November 2020. Retrieved 16 August 2020.
- PMID 32697968.
- PMID 32580969.
- ^ Dockrill P (11 November 2020). "Scientists Just Found a Mysteriously Hidden 'Gene Within a Gene' in SARS-CoV-2". ScienceAlert. Archived from the original on 17 November 2020. Retrieved 11 November 2020.
- PMID 33001029.
- ^ PMID 34147139.
- ^ PMID 33563978.
- PMID 33219796.
- ^ PMID 32416074.
- S2CID 214683303.
- S2CID 256822274.
- ^ PMID 34753934.
- PMID 32416074.
- PMID 32015507.
- S2CID 246902858.
- PMID 32742035.
We detected in total 65776 variants with 5775 distinct variants.
- PMID 32794443.
- ^ World Health Organization (27 November 2021). "Tracking SARS-CoV-2 variants". World Health Organization. Archived from the original on 6 June 2021. Retrieved 28 November 2021.
- ^ "SARS-CoV-2 mink-associated variant strain – Denmark". WHO. 3 December 2020. Archived from the original on 31 December 2020. Retrieved 30 December 2020.
- PMID 33236021.
- ^ PMID 32292689.
- ^ PMID 32075877.
- ^ Mandelbaum RF (19 February 2020). "Scientists Create Atomic-Level Image of the New Coronavirus's Potential Achilles Heel". Gizmodo. Archived from the original on 8 March 2020. Retrieved 13 March 2020.
- PMID 35311562.
- ^ "GISAID - gisaid.org". gisaid.org. Retrieved 16 September 2023.
- PMID 32159237.
- ^ PMID 32928234.
- ^ PMID 32704018.
- PMID 32687176.
- PMID 32431949.
- PMID 32275855.
- PMID 32009228.
- PMID 32094589.
- PMID 32094589.
- ^ El Sahly HM. "Genomic Characterization of the 2019 Novel Coronavirus". The New England Journal of Medicine. Archived from the original on 17 February 2020. Retrieved 9 February 2020.
- ^ "Novel coronavirus structure reveals targets for vaccines and treatments". National Institutes of Health (NIH). 2 March 2020. Archived from the original on 1 April 2020. Retrieved 3 April 2020.
- S2CID 214725955.
- PMID 33164751.
- ^ "Anatomy of a Killer: Understanding SARS-CoV-2 and the drugs that might lessen its power". The Economist. 12 March 2020. Archived from the original on 14 March 2020. Retrieved 14 March 2020.
- BMJ. Archived(PDF) from the original on 13 June 2020. Retrieved 25 May 2020.
- PMID 34285133.
- ^ Fact sheet for healthcare providers: Emergency Use Authorization for Paxlovid (PDF). Pfizer. 22 December 2021. Archived from the original on 23 December 2021.
- ^ "Paxlovid EPAR". European Medicines Agency (EMA). 24 January 2022. Retrieved 3 February 2022. Text was copied from this source which is copyright European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- ^ Oral COVID-19 antiviral, Paxlovid, approved by UK regulator. Medicines and Healthcare products Regulatory Agency. 31 December 2021.
- ^ Health Canada authorizes Paxlovid for patients with mild to moderate COVID-19 at high risk of developing serious disease. Health Canada. 17 January 2022. Retrieved 24 April 2022.
- ^ FDA Authorizes First Oral Antiviral for Treatment of COVID-19. U.S. Food and Drug Administration (FDA). 22 December 2021. Retrieved 22 December 2021.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ Whipple T (23 October 2021). "Moonshot is the spanner in the Covid-19 works the country needs". The Times. Retrieved 5 November 2021.
- PMID 32109273.
- PMID 33587929.
- PMID 32052846.
- PMID 33658326.
- PMID 34369565.
- ^ a b c d "COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU)". ArcGIS. Johns Hopkins University. Retrieved 10 March 2023.
- ^ Branswell H (30 January 2020). "Limited data on coronavirus may be skewing assumptions about severity". STAT. Archived from the original on 1 February 2020. Retrieved 13 March 2020.
- PMID 32014114.
- ^ Boseley S, McCurry J (30 January 2020). "Coronavirus deaths leap in China as countries struggle to evacuate citizens". The Guardian. Archived from the original on 6 February 2020. Retrieved 10 March 2020.
- ^ Paulinus A (25 February 2020). "Coronavirus: China to repay Africa in safeguarding public health". The Sun. Archived from the original on 9 March 2020. Retrieved 10 March 2020.
Further reading
- Bar-On YM, Flamholz A, Phillips R, Milo R (April 2020). "SARS-CoV-2 (COVID-19) by the numbers". eLife. 9. PMID 32228860.
- Brüssow H (May 2020). "The Novel Coronavirus - A Snapshot of Current Knowledge". Microbial Biotechnology. 13 (3): 607–612. PMID 32144890.
- Cascella M, Rajnik M, Aleem A, Dulebohn S, Di Napoli R (January 2020). "Features, Evaluation and Treatment Coronavirus (COVID-19)". StatPearls. from the original on 6 April 2020. Retrieved 4 April 2020.
- Laboratory testing for coronavirus disease 2019 (COVID-19) in suspected human cases (Report). hdl:10665/331329.
- Zoumpourlis V, Goulielmaki M, Rizos E, Baliou S, Spandidos DA (October 2020). "[Comment] The COVID‑19 pandemic as a scientific and social challenge in the 21st century". Molecular Medicine Reports (Review). 22 (4): 3035–3048. PMID 32945405.
External links
- "Coronavirus Disease 2019 (COVID-19)". Centers for Disease Control and Prevention (CDC). 11 February 2020.
- "Coronavirus disease (COVID-19) Pandemic". World Health Organization (WHO).
- "SARS-CoV-2 (Severe acute respiratory syndrome coronavirus 2) Sequences". National Center for Biotechnology Information (NCBI).
- "COVID-19 Resource Centre". The Lancet.
- "Coronavirus (Covid-19)". The New England Journal of Medicine.
- "Covid-19: Novel Coronavirus Outbreak". Wiley. Archived from the original on 24 September 2020. Retrieved 13 February 2020.
- "SARS-CoV-2". Virus Pathogen Database and Analysis Resource.
- "SARS-CoV-2 related protein structures". Protein Data Bank.


