Spinal cord injury
| Spinal cord injury | |
|---|---|
vasopressors[1] | |
| Frequency | c. 12,000 per year (USA)[2] |
A spinal cord injury (SCI) is damage to the
In the majority of cases the damage results from
Efforts to prevent SCI include individual measures such as using safety equipment, societal measures such as safety regulations in sports and traffic, and improvements to equipment. Treatment starts with
In the United States, about 12,000 people a year survive a spinal cord injury.
Classification

|

|
| The effects of injury depend on the level along the spinal column (left). A dermatome is an area of the skin that sends sensory messages to a specific spinal nerve (right).
| |
| |
| Spinal nerves exit the spinal cord between each pair of vertebrae. | |
Spinal cord injury can be
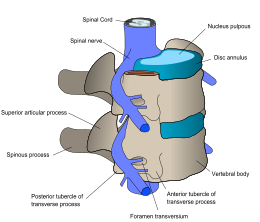
At each level of the spinal column, spinal nerves branch off from either side of the spinal cord and exit between a pair of vertebrae, to innervate a specific part of the body. The area of skin innervated by a specific spinal nerve is called a dermatome, and the group of muscles innervated by a single spinal nerve is called a myotome. The part of the spinal cord that was damaged corresponds to the spinal nerves at that level and below. Injuries can be cervical 1–8 (C1–C8), thoracic 1–12 (T1–T12), lumbar 1–5 (L1–L5),[9] or sacral (S1–S5).[10] A person's level of injury is defined as the lowest level of full sensation and function.[11] Paraplegia occurs when the legs are affected by the spinal cord damage (in thoracic, lumbar, or sacral injuries), and tetraplegia occurs when all four limbs are affected (cervical damage).[12]
SCI is also classified by the degree of impairment. The International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI), published by the American Spinal Injury Association (ASIA), is widely used to document sensory and motor impairments following SCI.[13] It is based on neurological responses, touch and pinprick sensations tested in each dermatome, and strength of the muscles that control key motions on both sides of the body.[14] Muscle strength is scored on a scale of 0–5 according to the table on the right, and sensation is graded on a scale of 0–2: 0 is no sensation, 1 is altered or decreased sensation, and 2 is full sensation.[15] Each side of the body is graded independently.[15]
| Muscle strength[16] | ASIA Impairment Scale for classifying spinal cord injury[14][17] | ||
|---|---|---|---|
| Grade | Muscle function | Grade | Description |
| 0 | No muscle contraction | A | Complete injury. No motor or sensory function is preserved in the sacral segments S4 or S5. |
| 1 | Muscle flickers | B | Sensory incomplete. Sensory but not motor function is preserved below the level of injury, including the sacral segments. |
| 2 | Full range of motion, gravity eliminated | C | Motor incomplete. Motor function is preserved below the level of injury, and more than half of muscles tested below the level of injury have a muscle grade less than 3 (see muscle strength scores, left). |
| 3 | Full range of motion, against gravity | D | Motor incomplete. Motor function is preserved below the level of injury and at least half of the key muscles below the neurological level have a muscle grade of 3 or more. |
| 4 | Full range of motion against resistance | E | Normal. No motor or sensory deficits, but deficits existed in the past. |
| 5 | Normal strength | ||
Complete and incomplete injuries
| Complete | Incomplete | |
|---|---|---|
| Tetraplegia | 18.3% | 34.1% |
| Paraplegia | 23.0% | 18.5% |
In a "complete" spinal injury, all functions below the injured area are lost, whether or not the spinal cord is severed.[10] An "incomplete" spinal cord injury involves preservation of motor or sensory function below the level of injury in the spinal cord.[19] To be classed as incomplete, there must be some preservation of sensation or motion in the areas innervated by S4 to S5,[20] e.g. voluntary external anal sphincter contraction.[19] The nerves in this area are connected to the very lowest region of the spinal cord, and retaining sensation and function in these parts of the body indicates that the spinal cord is only partially damaged. Incomplete injury by definition includes a phenomenon known as sacral sparing: some degree of sensation is preserved in the sacral dermatomes, even though sensation may be more impaired in other, higher dermatomes below the level of the lesion.[21] Sacral sparing has been attributed to the fact that the sacral spinal pathways are not as likely as the other spinal pathways to become compressed after injury due to the lamination of fibers within the spinal cord.[21]
Spinal cord injury without radiographic abnormality
Central cord syndrome

Anterior spinal artery syndrome
Anterior spinal artery syndrome also known as anterior spinal cord syndrome, due to damage to the front portion of the spinal cord or reduction in the blood supply from the anterior spinal artery, can be caused by fractures or dislocations of vertebrae or herniated disks.[26] Below the level of injury, motor function, pain sensation, and temperature sensation are lost, while sense of touch and proprioception (sense of position in space) remain intact.[29][27] These differences are due to the relative locations of the spinal tracts responsible for each type of function.
Brown-Séquard syndrome
Brown-Séquard syndrome occurs when the spinal cord is injured on one side much more than the other.[30] It is rare for the spinal cord to be truly hemisected (severed on one side), but partial lesions due to penetrating wounds (such as gunshot or knife wounds) or fractured vertebrae or tumors are common.[31] On the ipsilateral side of the injury (same side), the body loses motor function, proprioception, and senses of vibration and touch.[30] On the contralateral (opposite side) of the injury, there is a loss of pain and temperature sensations.If the injury is above pyramidal decussation there is contralateral hemiplagia, at the level of decussation there is completed motor loss on both sides and below pyramidal decussation there is ipsilateral hemiplagia.
[28][30]Spinothalamic tracts are in charge for pain and temperature sensation and because these tracts cross to the opposite side and above the spinal cord there is loss on the contralateral side.[32]
Posterior spinal artery syndrome
Conus medullaris and cauda equina syndromes
Signs and symptoms
| Level | Motor Function |
|---|---|
| C1–C6 | Neck flexors
|
| C1–T1 | Neck extensors
|
| C3, C4, C5 | Supply diaphragm (mostly C4 )
|
| C5, C6 | Move shoulder, raise arm (deltoid); flex elbow (biceps) |
| C6 | externally rotate ( supinate ) the arm
|
| C6, C7 | pronate wrist
|
| C7, T1 | Flex wrist; supply small muscles of the hand |
| T1–T6 | |
L1
|
Abdominal muscles |
L4
|
Flex thigh |
L4
|
quadriceps femoris )
|
L5, S1
|
tibialis anterior); Extend toes
|
| Extend leg at the Plantar flex foot and flex toes
|
The specific parts of the body affected by loss of function are determined by the level of injury. Some signs, such as bowel and bladder dysfunction can occur at any level. Neurogenic bladder involves a compromised ability to empty the bladder and is a common symptom of spinal cord injury. This can lead to high pressures in the bladder that can damage the kidneys.[44]
Lumbosacral
The effects of injuries at or above the
Thoracic
In addition to the problems found in lower-level injuries, thoracic (chest height) spinal lesions can affect the muscles in the trunk. Injuries at the level of T1 to T8 result in inability to control the abdominal muscles. Trunk stability may be affected; even more so in higher level injuries.[46] The lower the level of injury, the less extensive its effects. Injuries from T9 to T12 result in partial loss of trunk and abdominal muscle control. Thoracic spinal injuries result in paraplegia, but function of the hands, arms, and neck are not affected.[47]
One condition that occurs typically in lesions above the T6 level is autonomic dysreflexia (AD), in which the blood pressure increases to dangerous levels, high enough to cause potentially deadly stroke.[9][48] It results from an overreaction of the system to a stimulus such as pain below the level of injury, because inhibitory signals from the brain cannot pass the lesion to dampen the excitatory sympathetic nervous system response.[6] Signs and symptoms of AD include anxiety, headache, nausea, ringing in the ears, blurred vision, flushed skin, and nasal congestion.[6] It can occur shortly after the injury or not until years later.[6]
Other autonomic functions may also be disrupted. For example, problems with body temperature regulation mostly occur in injuries at T8 and above.[45] Another serious complication that can result from lesions above T6 is neurogenic shock, which results from an interruption in output from the sympathetic nervous system responsible for maintaining muscle tone in the blood vessels.[6][48] Without the sympathetic input, the vessels relax and dilate.[6][48] Neurogenic shock presents with dangerously low blood pressure, low heart rate, and blood pooling in the limbs—which results in insufficient blood flow to the spinal cord and potentially further damage to it.[49]
Cervical spine
Spinal cord injuries at the cervical (neck) level result in full or partial
| Level | Motor Function | Respiratory function |
|---|---|---|
| C1–C4 | Full paralysis of the limbs | Cannot breathe without mechanical ventilation |
| C5 | Paralysis of the wrists, hands, and triceps
|
Difficulty coughing, may need help clearing secretions |
| C6 | Paralysis of the wrist flexors, triceps, and hands | |
| C7–C8 | Some hand muscle weakness, difficulty grasping and releasing |
Complications
Complications of spinal cord injuries include pulmonary edema, respiratory failure, neurogenic shock, and paralysis below the injury site.
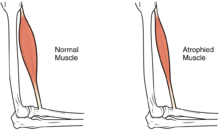
In the long term, the loss of muscle function can have additional effects from disuse, including
People with SCI are at especially high risk for respiratory and cardiovascular problems, so hospital staff must be watchful to avoid them.
Another potentially deadly threat to respiration is
Urinary tract infection (UTI) is another risk that may not display the usual symptoms (pain, urgency, and frequency); it may instead be associated with worsened spasticity.
An estimated 24–45% of people with SCI have disorders of
Causes

Spinal cord injuries are most often caused by
In the US,
SCI can also be of a nontraumatic origin. Nontraumatic lesions cause anywhere from 30 to 80% of all SCI;
Prevention
Vehicle-related SCI is prevented with measures including societal and individual efforts to reduce
Diagnosis
A person's presentation in context of trauma or non-traumatic background determines suspicion for a spinal cord injury. The features are namely paralysis, sensory loss, or both at any level. Other symptoms may include incontinence.[90]
A radiographic evaluation using an
Neurological evaluations to help determine the degree of impairment are performed initially and repeatedly in the early stages of treatment; this determines the rate of improvement or deterioration and informs treatment and prognosis.[93][94] The ASIA Impairment Scale outlined above is used to determine the level and severity of injury.[10]
Management
Prehospital treatment
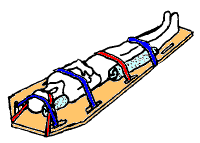
The first stage in the management of a suspected spinal cord injury is geared toward basic life support and preventing further injury: maintaining airway, breathing, and circulation and restricting further motion of the spine.[24] In the emergency setting, most people who has been subjected to forces strong enough to cause SCI are treated as though they have instability in the spinal column and have
A rigid
Modern trauma care includes a step called clearing the cervical spine, ruling out spinal cord injury if the patient is fully conscious and not under the influence of drugs or alcohol, displays no neurological deficits, has no pain in the middle of the neck and no other painful injuries that could distract from neck pain.[35] If these are all absent, no spinal motion restriction is necessary.[98]
If an unstable spinal column injury is moved, damage may occur to the spinal cord.
Early hospital treatment
Initial care in the hospital, as in the prehospital setting, aims to ensure adequate airway, breathing, cardiovascular function, and spinal motion restriction.
If the
The CAMPER Trial led by Dr Kwon and subsequent studies by the UCSF TRACK-SCI group (Dhall) have shown that spinal cord perfusion pressure (SCPP) goals are more closely associated with better neurologic recovery than MAP goals. Some institutions have adopted these SCPP goals and lumbar CSF drain placement as a standard of care.
The
Surgery may be necessary, e.g. to relieve excess pressure on the cord, to stabilize the spine, or to put vertebrae back in their proper place.[106] In cases involving instability or compression, failing to operate can lead to worsening of the condition.[106] Surgery is also necessary when something is pressing on the cord, such as bone fragments, blood, material from ligaments or intervertebral discs,[110] or a lodged object from a penetrating injury.[89] Although the ideal timing of surgery is still debated, studies have found that earlier surgical intervention (within 12 hours of injury) is associated with better outcomes.[111] This type of surgery is often referred to as "Ultra-Early", coined by Burke et al. at UCSF. Sometimes a patient has too many other injuries to be a surgical candidate this early.[106] Surgery is controversial because it has potential complications (such as infection), so in cases where it is not clearly needed (e.g. the cord is being compressed), doctors must decide whether to perform surgery based on aspects of the patient's condition and their own beliefs about its risks and benefits.[112] Recent large-scale studies have shown that patients who do undergo earlier surgery (within 12–24 hours) experience significantly lower rates of life-threatening complications and spend less time in hospital and critical care.[113][114] However, in cases where a more conservative approach is chosen, bed rest, cervical collars, motion restriction devices, and optionally traction are used.[115] Surgeons may opt to put traction on the spine to remove pressure from the spinal cord by putting dislocated vertebrae back into alignment, but herniation of intervertebral disks may prevent this technique from relieving pressure.[116] Gardner-Wells tongs are one tool used to exert spinal traction to reduce a fracture or dislocation and to reduce motion to the affected areas.[117]
Rehabilitation


SCI patients often require extended treatment in specialized spinal unit or an
In the acute phase physical therapists focus on the patient's respiratory status, prevention of indirect complications (such as pressure ulcers), maintaining range of motion, and keeping available musculature active.[119]
For people whose injuries are high enough to interfere with breathing, there is great emphasis on airway clearance during this stage of recovery.
The amount of functional recovery and independence achieved in terms of activities of daily living, recreational activities, and employment is affected by the level and severity of injury.[123] The Functional Independence Measure (FIM) is an assessment tool that aims to evaluate the function of patients throughout the rehabilitation process following a spinal cord injury or other serious illness or injury.[124] It can track a patient's progress and degree of independence during rehabilitation.[124] People with SCI may need to use specialized devices and to make modifications to their environment in order to handle activities of daily living and to function independently. Weak joints can be stabilized with devices such as ankle-foot orthoses (AFOs) or knee-ankle-foot orthoses (KAFOs), but walking may still require a lot of effort.[125] Increasing activity will increase chances of recovery.[126]
For treatment of paralysis levels in the lower thoracic spine or lower, starting therapy with an orthosis is promising from the intermediate phase (2–26 weeks after the incident).[127][128][129] In patients with complete paraplegia (ASIA A), this applies to lesion heights between T12 and S5. In patients with incomplete paraplegia (ASIA B-D), orthoses are even suitable for lesion heights above T12. In both cases, however, a detailed muscle function test must be carried out to precisely plan the construction with an orthosis.[130]
Prognosis
Spinal cord injuries generally result in at least some
People with nontraumatic causes of SCI have been found to be less likely to develop complete injuries and some complications such as pressure sores and deep vein thrombosis, and to have shorter hospital stays.[12] Their scores on functional tests were better than those of people with traumatic SCI upon hospital admission, but when they were tested upon discharge, those with traumatic SCI had improved such that both groups' results were the same.[12] In addition to the completeness and level of the injury, age and concurrent health problems affect the extent to which a person with SCI will be able to live independently and to walk.[9] However, in general people with injuries to L3 or below will likely be able to walk functionally, T10 and below to walk around the house with bracing, and C7 and below to live independently.[9] New therapies are beginning to provide hope for better outcomes in patients with SCI, but most are in the experimental/translational stage.[4]
One important predictor of motor recovery in an area is presence of sensation there, particularly pain perception.[39] Most motor recovery occurs in the first year post-injury, but modest improvements can continue for years; sensory recovery is more limited.[133] Recovery is typically quickest during the first six months.[134] Spinal shock, in which reflexes are suppressed, occurs immediately after the injury and resolves largely within three months but continues resolving gradually for another 15.[135]
Sexual dysfunction after spinal injury is common. Problems that can occur include erectile dysfunction, loss of ability to ejaculate, insufficient lubrication of the vagina, and reduced sensation and impaired ability to orgasm.[55] Despite this, many people learn ways to adapt their sexual practices so they can lead satisfying sex lives.[136]
Although life expectancy has improved with better care options, it is still not as good as the uninjured population. The higher the level of injury, and the more complete the injury, the greater the reduction in life expectancy.[84] Mortality is very elevated within a year of injury.[84]
Epidemiology
Breakdown of age at time of injury in the US from 1995–1999.[137]
Worldwide, the number of new cases since 1995 of SCI ranges from 10.4 to 83 people per million per year.[106] This wide range of numbers is probably partly due to differences among regions in whether and how injuries are reported.[106] In North America, about 39 people per every million incur SCI traumatically each year, and in Western Europe, the incidence is 16 per million.[138][139] In the United States, the incidence of spinal cord injury has been estimated to be about 40 cases per 1 million people per year or around 12,000 cases per year.[140] In China, the incidence is approximately 60,000 per year.[141] The estimated
SCI is present in about 2% of all cases of blunt force trauma.
Males account for four out of five traumatic spinal cord injuries.[25] Most of these injuries occur in men under 30 years of age.[10] The average age at the time of injury has slowly increased from about 29 years in the 1970s to 41.[25] In Pakistan, spinal cord injury is more common in males (92.68%) as compared to females in the 20-30 years of age group with a median age of 40 years, although people from 12-70 years of age suffered from spinal cord injury [73] Rates of injury are at their lowest in children, at their highest in the late teens to early twenties, then get progressively lower in older age groups; however rates may rise in the elderly.[144] In Sweden between 50 and 70% of all cases of SCI occur in people under 30, and 25% occur in those over 50.[74] While SCI rates are highest among people age 15–20,[145] fewer than 3% of SCIs occur in people under 15.[146] Neonatal SCI occurs in one in 60,000 births, e.g. from breech births or injuries by forceps.[147] The difference in rates between the sexes diminishes in injuries at age 3 and younger; the same number of girls are injured as boys, or possibly more.[148] Another cause of pediatric injury is child abuse such as shaken baby syndrome.[147] For children, the most common cause of SCI (56%) is vehicle crashes.[149] High numbers of adolescent injuries are attributable in a large part to traffic accidents and sports injuries.[150] For people over 65, falls are the most common cause of traumatic SCI.[5] The elderly and people with severe arthritis are at high risk for SCI because of defects in the spinal column.[151] In nontraumatic SCI, the gender difference is smaller, the average age of occurrence is greater, and incomplete lesions are more common.[79]
History

SCI has been known to be devastating for millennia; the ancient Egyptian Edwin Smith Papyrus from 2500 BC, the first known description of the injury, says it is "not to be treated".[152] Hindu texts dating back to 1800 BC also mention SCI and describe traction techniques to straighten the spine.[152] The Greek physician Hippocrates, born in the fifth century BC, described SCI in his Hippocratic Corpus and invented traction devices to straighten dislocated vertebrae.[153] But it was not until Aulus Cornelius Celsus, born 30 BC, noted that a cervical injury resulted in rapid death that the spinal cord itself was implicated in the condition.[152] In the second century AD the Greek physician Galen experimented on monkeys and reported that a horizontal cut through the spinal cord caused them to lose all sensation and motion below the level of the cut.[154] The seventh-century Greek physician Paul of Aegina described surgical techniques for treatment of broken vertebrae by removing bone fragments, as well as surgery to relieve pressure on the spine.[152] Little medical progress was made during the Middle Ages in Europe; it was not until the Renaissance that the spine and nerves were accurately depicted in human anatomy drawings by Leonardo da Vinci and Andreas Vesalius.[154]
In 1762, Andre Louis, a surgeon, removed a bullet from the lumbar spine of a patient, who regained motion in the legs.[154] In 1829, Gilpin Smith, a surgeon, performed a successful laminectomy that improved the patient's sensation.[155] However, the idea that SCI was untreatable remained predominant until the early 20th century.[156] In 1934, the mortality rate in the first two years after injury was over 80%, mostly due to infections of the urinary tract and pressure sores,[157] the latter of which were believed to be intrinsic to SCI rather than a result of continuous bedrest.[158] It was not until the second half of the century that breakthroughs in imaging, surgery, medical care, and rehabilitation medicine contributed to a substantial improvement in SCI care.[156] The relative incidence of incomplete compared to complete injuries has improved since the mid-20th century, due mainly to the emphasis on faster and better initial care and stabilization of spinal cord injury patients.[159] The creation of emergency medical services to professionally transport people to the hospital is given partial credit for an improvement in outcomes since the 1970s.[160] Improvements in care have been accompanied by increased life expectancy of people with SCI; survival times have improved by about 2000% since 1940.[161] In 2015/2016 23% of people in nine spinal injury centres in England had their discharge delayed because of disputes about who should pay for the equipment they needed.[162]
Research directions
Scientists are investigating various avenues for treatment of spinal cord injury. Therapeutic research is focused on two main areas:
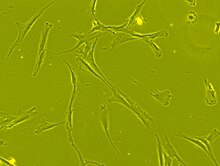
Another type of approach is tissue engineering, using
One avenue being explored to allow paralyzed people to walk and to aid in rehabilitation of those with some walking ability is the use of wearable powered robotic exoskeletons.[166] The devices, which have motorized joints, are put on over the legs and supply a source of power to move and walk.[166] Several such devices are already available for sale, but investigation is still underway as to how they can be made more useful.[166]
Preliminary studies of epidural spinal cord stimulators for motor complete injuries have demonstrated some improvement,[167] and in some cases to enable walking to some degree bypassing the injury.[168][169]
In 2014
There have been a number of advances in technological spinal cord injury treatment, including the use of implants that provided a "digital bridge" between the brain and the spinal cord. In a study published in May 2023 in the journal Nature, researchers in Switzerland described such implants which allowed a 40-year old man, paralyzed from the hips down for 12 years, to stand, walk and ascend a steep ramp with only the assistance of a walker. More than a year after the implant was inserted, he has retained these abilities and was walking with crutches even when the implant was switched off.[172]
See also
References
- ^ ISBN 9780996826235.
- ^ a b c "Spinal Cord Injury Facts and Figures at a Glance" (PDF). 2012. Archived from the original (PDF) on 28 June 2018. Retrieved 16 May 2018.
- PMID 33066029.
- ^ PMID 29800461.
- ^ PMID 26240569.
- ^ a b c d e f Newman, Fleisher & Fink 2008, p. 348.
- ^ a b Newman, Fleisher & Fink 2008, p. 335.
- (PDF) from the original on 2015-12-08.
- ^ a b c d e Cifu & Lew 2013, p. 197.
- ^ a b c d e f g h i j k Office of Communications and Public Liaison, National Institute of Neurological Disorders and Stroke, ed. (2013). Spinal Cord Injury: Hope Through Research. National Institutes of Health. Archived from the original on 2015-11-19.
- ^ Miller & Marini 2012, p. 138.
- ^ a b c d e Field-Fote 2009, p. 5.
- S2CID 12799339.
- ^ a b "Standard Neurological Classification of Spinal Cord Injury" (PDF). American Spinal Injury Association & ISCOS. Archived from the original on June 18, 2011. Retrieved 5 November 2015.
{{cite web}}: CS1 maint: unfit URL (link) - ^ a b Weiss 2010, p. 307.
- ^ Harvey 2008, p. 7.
- ^ Teufack, Harrop & Ashwini 2012, p. 67.
- ^ Field-Fote 2009, pp. 7–8.
- ^ PMID 17321849.
- ^ Sabharwal 2014, p. 840.
- ^ PMID 4009195.
- ^ a b c Peitzman et al. 2012, p. 288.
- ^ Peitzman et al. 2012, pp. 288–89.
- ^ a b c Peitzman et al. 2012, p. 289.
- ^ a b c d e f Sabharwal 2014, p. 839.
- ^ a b c Snell 2010, p. 170.
- ^ a b c Namdari, Pill & Mehta 2014, p. 297.
- ^ a b Marx, Walls & Hockberger 2013, p. 1420.
- ^ a b Field-Fote 2009, p. 9.
- ^ a b c d e f Field-Fote 2009, p. 10.
- ^ Snell 2010, p. 171.
- )
- ^ Roos 2012, pp. 249–50.
- ^ Ilyas & Rehman 2013, p. 389.
- ^ a b c Peitzman et al. 2012, p. 294.
- ^ Snell 2010, p. 167.
- ^ a b c d Marx, Walls & Hockberger 2013, p. 1422.
- ^ a b Bashir 2022.
- ^ a b c d e Field-Fote 2009, p. 11.
- ^ Augustine 2011, p. 199.
- ^ Sabharwal 2013, p. 39.
- ^ Snell 2010, p. 169.
- ^ Augustine 2011, p. 200.
- PMID 26003248
- ^ a b Weiss 2010, p. 313.
- ^ Weiss 2010, pp. 311, 313.
- ^ Weiss 2010, p. 311.
- ^ S2CID 10504.
- ^ a b Holtz & Levi 2010, p. 63.
- ^ Sabharwal 2013, pp. 53–54.
- ^ Sabharwal 2014, p. 843.
- ^ a b c Holtz & Levi 2010, p. 70.
- ^ Weiss 2010, p. 314–15.
- ^ Field-Fote 2009, p. 17.
- ^ PMID 22925747.
- ^ ISBN 978-1-4587-6331-0. Archivedfrom the original on 2014-07-07.
- ^ Weiss 2010, p. 315.
- ^ Frontera, Silver & Rizzo 2014, p. 407.
- S2CID 1143205.
- ^ a b Field-Fote 2009, p. 16.
- ^ a b Field-Fote 2009, p. 15.
- PMID 21651382.
- ^ Sabharwal 2013, p. 26.
- ^ Field-Fote 2009, p. 13.
- ^ a b c Holtz & Levi 2010, p. 69.
- S2CID 145246983.
- ^ Sabharwal 2013, p. 27.
- ^ PMID 17640451.
- ^ Augustine 2011, p. 198.
- ^ Clark West, Stefan Roosendaal, Joost Bot and Frank Smithuis. "Spine injury – TLICS Classification". Radiology Assistant. Archived from the original on 2017-10-27. Retrieved 2017-10-26.
{{cite web}}: CS1 maint: multiple names: authors list (link) - PMID 3990933.
- ^ Sabharwal 2013, pp. 24–25.
- ^ a b Bashir 2017, p. 48.
- ^ a b c Holtz & Levi 2010, p. 10.
- ^ Sabharwal 2013, p. 34.
- ^ Brown et al. 2008, p. 1132.
- ^ PMID 26343846.
- ^ Frontera, Silver & Rizzo 2014, p. 39.
- ^ PMID 24659962.
- PMID 11346833.
- PMID 23318556.
- ^ Sabharwal 2013, p. 24.
- PMID 20486810.
- ^ a b c Fulk, Behrman & Schmitz 2013, p. 890.
- ^ Moore 2006, pp. 530–31.
- ^ a b Sabharwal 2013, p. 31.
- ^ a b Sabharwal 2013, p. 32.
- ^ Sabharwal 2013, p. 33.
- ^ a b c d Wyatt et al. 2012, p. 384.
- ^ "How is SCI diagnosed?". National Institute of Child Health and Human Development. 2016. Retrieved 2019-01-01.
- ^ Holtz & Levi 2010, p. 78.
- ^ DeKoning 2014, p. 389.
- ^ Holtz & Levi 2010, pp. 64–65.
- ^ a b Sabharwal 2013, p. 55.
- ^ a b Sabharwal 2013, p. 38.
- ^ Augustine 2011, p. 207.
- ^ a b Cameron et al. 2014.
- ^ a b Sabharwal 2013, p. 37.
- PMID 23458580.
- ^ PMID 20175667.
- ^ a b Sabharwal 2013, p. 53.
- ^ a b Bigelow & Medzon 2011, p. 173.
- ^ DeKoning 2014, p. 373.
- ^ ISBN 9781292170848.
- ^ a b Holtz & Levi 2010, pp. 63–64.
- ^ S2CID 8087959.
- S2CID 202671826.
- ^ Bigelow & Medzon 2011, pp. 167, 176.
- ^ PMID 28658409.
- ^ Holtz & Levi 2010, p. 65.
- PMID 30496474.
- ^ Holtz & Levi 2010, pp. 65–69.
- S2CID 232244800.
- S2CID 236990438.
- ^ Holtz & Levi 2010, p. 67.
- ^ Bigelow & Medzon 2011, p. 177.
- S2CID 3183490.
- PMID 12431287.
- ^ Fulk G; Schmitz T; Behrman A (2007). "Traumatic Spinal Cord Injury". In O'Sullivan S; Schmitz T (eds.). Physical Rehabilitation (5th ed.). Philadelphia: F.A. Davis. pp. 937–96.
- ^ PMID 21061895.
- ^ PMID 16867197. Archived from the originalon 2022-02-12. Retrieved 2014-07-14.
- PMID 14508412.
- ^ Weiss 2010, p. 306.
- ^ PMID 20437324.
- PMID 22773254.
- .
- ^ James W. Rowland, Gregory W. J. Hawryluk. "Current status of acute spinal cord injury pathophysiology and emerging therapies: promise on the horizon". JNS Journal of Neurosurgery. 25: 2, 6.[permanent dead link]
- S2CID 30220082.
- ^ Steven C. Kirshblum, Michael M. Priebe. "Spinal Cord Injury Medicine. 3. Rehabilitation Phase After Acute Spinal Cord Injury". Spinal Cord Injury Medicine. 88.
- ISBN 978-3-437-46431-7.
- ^ a b Peitzman et al. 2012, p. 293.
- ^ PMID 1787981.
- ^ Field-Fote 2009, p. 8.
- ^ Yakura, J.S. (Dec 22, 1996). "Recovery following spinal cord injury". American Rehabilitation. Retrieved 5 November 2015.
- ^ Cortois & Charvier 2015, p. 236.
- ^ Elliott 2010.
- ISBN 978-0-309-16520-4. Archivedfrom the original on 6 November 2017.
- PMID 26724625.
- ^ PMID 23820516.
- ^ "Spinal Cord Injury Facts". Foundation for Spinal Cord Injury Prevention, Care & Cure. June 2009. Archived from the original on 2 November 2015. Retrieved 5 November 2015.
- S2CID 206158809.
- ^ PMID 25278785.
- ^ Field-Fote 2009, p. 3.
- PMID 22270188.
- ^ Pellock & Myer 2013, p. 124.
- ^ Hammell 2013, p. 274.
- ^ a b Sabharwal 2013, p. 388.
- S2CID 8040837.
- ^ Augustine 2011, p. 197.
- ^ PMID 25678991.
- ^ Augustine 2011, pp. 197–98.
- ^ PMID 15264783.
- ^ Holtz & Levi 2010, pp. 3–4.
- ^ a b c Holtz & Levi 2010, p. 5.
- ^ Holtz & Levi 2010, p. 6.
- ^ a b Morganti-Kossmann, Raghupathi & Maas 2012, p. 229.
- ^ Fallah, Dance & Burns 2012, p. 235.
- PMID 11609092.
- PMID 11805601.
- ^ Sabharwal 2013, p. 35.
- ^ Holtz & Levi 2010, p. 7.
- ^ "Revealed: Patients stranded in hospital for months as officials 'squabble' over equipment". Health Service Journal. 12 January 2018. Retrieved 15 February 2018.
- S2CID 23121381.
- ^ Wirth, Edward (September 14, 2016). "Initial Clinical Trials of hESC-Derived Oligodendrocyte Progenitor Cells in Subacute Spinal Cord Injury" (PDF). ISCoS Meeting presentation. Asterias Biotherapeutics. Archived (PDF) from the original on September 21, 2016. Retrieved September 14, 2016.
- ^ "Asterias Biotherapeutics Announces Positive Efficacy Data in Patients with Complete Cervical Spinal Cord Injuries Treated with AST-OPC1". asteriasbiotherapeutics.com. Archived from the original on 2016-09-20. Retrieved 2016-09-15.
- ^ PMID 26463355.
- PMID 25646771.
- ^ "Paralysed man with severed spine walks thanks to implant". BBC News. 2022-02-07. Retrieved 2022-02-11.
- TheGuardian.com. 20 October 2014.
- ^ Bashir, F. "What Is Cauda Equina Syndrome: Causes, Sign, Symptoms, Diagnosis, Treatment And Prognosis". FCP Medical. Retrieved 22 July 2022.
- ^ Whang, Oliver (24 May 2023). "Brain Implants Allow Paralyzed Man to Walk Using His Thoughts". The New York Times. Archived from the original on 2023-07-26.
Bibliography
- Adams JG (5 September 2012). Emergency Medicine: Clinical Essentials. Elsevier Health Sciences. ISBN 978-1-4557-3394-1.
- Augustine JJ (21 November 2011). "Spinal trauma". In Campbell JR (ed.). International Trauma Life Support for Emergency Care Providers. Pearson Education. ISBN 978-0-13-300408-3.
- Bigelow S, Medzon R (16 June 2011). "Injuries of the spine: Nerve". In Legome E, Shockley LW (eds.). Trauma: A Comprehensive Emergency Medicine Approach. Cambridge University Press. ISBN 978-1-139-50072-2.
- Brown J, Wyatt JP, Illingworth RN, Clancy MJ, Munro P (6 June 2008). Oxford American Handbook of Emergency Medicine. Oxford University Press. ISBN 978-0-19-977948-2.
- Cameron P, Jelinek G, Kelly AM, Brown AF, Little M (1 April 2014). Textbook of Adult Emergency Medicine: Expert Consult. Elsevier Health Sciences UK. ISBN 978-0-7020-5438-9.
- Cifu DK, Lew HL (10 September 2013). Handbook of Polytrauma Care and Rehabilitation. Demos Medical Publishing. ISBN 978-1-61705-100-5.
- Cortois F, Charvier K (21 May 2015). "Sexual dysfunction in patients with spinal cord lesions". In Vodusek DB, Boller F (eds.). Neurology of Sexual and Bladder Disorders: Handbook of Clinical Neurology. Elsevier Science. ISBN 978-0-444-63254-8.
- DeKoning EP (10 January 2014). "Cervical spine injuries". In Sherman, S., Weber, J., Schindlbeck, M., Patwari, R. (eds.). Clinical Emergency Medicine. McGraw-Hill Education. ISBN 978-0-07-179461-9.
- Elliott S (19 March 2010). "Sexual dysfunction in women with spinal cord injury". In Bono CM, Cardenas DD, Frost FS (eds.). Spinal Cord Medicine, Second Edition: Principles & Practice. Demos Medical Publishing. pp. 429–38. ISBN 978-1-935281-77-1.
- Field-Fote E (26 March 2009). "Spinal cord injury: An overview". In Field-Fote E (ed.). Spinal Cord Injury Rehabilitation. F.A. Davis. ISBN 978-0-8036-2319-4.
- Fallah A, Dance D, Burns AS (29 October 2012). "Rehabilitation of the individual with spinal cord injury". In Fehlings, M.G., Vaccaro, A.R., Maxwell B. (eds.). Essentials of Spinal Cord Injury: Basic Research to Clinical Practice. Thieme. ISBN 978-1-60406-727-9.
- Frontera WR, Silver JK, Rizzo TD (5 September 2014). Essentials of Physical Medicine and Rehabilitation. Elsevier Health Sciences. ISBN 978-0-323-22272-3.
- Fulk GD, Behrman AL, Schmitz TJ (23 July 2013). "Traumatic Spinal Cord Injury". In O'Sullivan S, Schmitz T (eds.). Physical Rehabilitation. F.A. Davis. ISBN 978-0-8036-4058-0.
- Hammell KW (11 December 2013). Spinal Cord Injury Rehabilitation. Springer. ISBN 978-1-4899-4451-1.
- Harvey L (2008). Management of Spinal Cord Injuries: A Guide for Physiotherapists. Elsevier Health Sciences. ISBN 978-0-443-06858-4.
- Holtz A, Levi R (6 July 2010). Spinal Cord Injury. Oxford University Press. ISBN 978-0-19-970681-5.
- Ilyas A, Rehman S (31 March 2013). Contemporary Surgical Management of Fractures and Complications. JP Medical Ltd. ISBN 978-93-5025-964-1.
- Marx J, Walls R, Hockberger R (1 August 2013). Rosen's Emergency Medicine: Concepts and Clinical Practice. Elsevier Health Sciences. ISBN 978-1-4557-4987-4.
- Miller E, Marini I (24 February 2012). "Sexuality and spinal cord injury counseling implications". In Marini I, Stebnicki MA (eds.). The Psychological and Social Impact of Illness and Disability, 6th Edition. Springer Publishing Company. ISBN 978-0-8261-0655-1.
- Moore K (2006). Clinically Oriented Anatomy. Lippincott Williams & Wilkins. ISBN 978-0-7817-3639-8.
- Morganti-Kossmann C, Raghupathi R, Maas A (19 July 2012). Traumatic Brain and Spinal Cord Injury: Challenges and Developments. Cambridge University Press. ISBN 978-1-107-00743-7.
- Namdari S, Pill S, Mehta S (21 October 2014). Orthopedic Secrets. Elsevier Health Sciences. ISBN 978-0-323-17285-1.
- Newman MF, Fleisher LA, Fink MP (2008). Perioperative Medicine: Managing for Outcome. Elsevier Health Sciences. ISBN 978-1-4160-2456-9.
- Peitzman AB, Fabian TC, Rhodes M, Schwab CW, Yealy DM (2012). The Trauma Manual: Trauma and Acute Care Surgery. Lippincott Williams & Wilkins. ISBN 978-1-4511-1679-3.
- Pellock JM, Myer EC (22 October 2013). Neurologic Emergencies in Infancy and Childhood. Elsevier Science. ISBN 978-1-4831-9392-2.
- Roos KL (7 March 2012). Emergency Neurology. Springer Science & Business Media. ISBN 978-0-387-88585-8.
- Sabharwal S (10 December 2013). Essentials of Spinal Cord Medicine. Demos Medical Publishing. ISBN 978-1-61705-075-6.
- Sabharwal S (5 September 2014). "Spinal cord injury (Cervical)". In Frontera WR, Silver JK, Rizzo TD (eds.). Essentials of Physical Medicine and Rehabilitation. Elsevier Health Sciences. ISBN 978-0-323-22272-3.
- Shah KH, Egan D, Quaas J (17 February 2012). Essential Emergency Trauma. Lippincott Williams & Wilkins. ISBN 978-1-4511-5318-7.
- Snell, R.S. (2010). "The spinal cord and the ascending and descending tracts". Clinical Neuroanatomy. Lippincott Williams & Wilkins. ISBN 978-0-7817-9427-5.
- Teufack S, Harrop JS, Ashwini DS (29 October 2012). "Spinal Cord Injury Classification". In Fehlings MG, Vaccaro AR, Maxwell B (eds.). Essentials of Spinal Cord Injury: Basic Research to Clinical Practice. Thieme. ISBN 978-1-60406-727-9.
- Weiss JM (15 March 2010). "Spinal cord injury". In Weiss, L.D., Weiss, J.M., Pobre, T. (eds.). Oxford American Handbook of Physical Medicine and Rehabilitation. Oxford University Press, USA. ISBN 978-0-19-970999-1.
- Wyatt JP, Illingworth RN, Graham CA, Hogg K, Robertson C, Clancy M (9 February 2012). Oxford Handbook of Emergency Medicine. OUP Oxford. ISBN 978-0-19-101605-9.
External links
- Spinal cord injury at Curlie
- Lorach, Henri; et al. (2023). "Walking naturally after spinal cord injury using a brain–spine interface". Nature. 618 (7963): 126–133. S2CID 258889735.


