Spinal nerve
| Spinal nerve | |
|---|---|
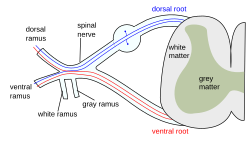 The formation of the spinal nerve from the posterior and anterior roots | |
| Details | |
| Identifiers | |
| Latin | nervus spinalis |
| MeSH | D013127 |
| TA98 | A14.2.00.027 |
| TA2 | 6143 |
| FMA | 5858 |
| Anatomical terms of neuroanatomy | |
A spinal nerve is a
Structure


Each spinal nerve is a mixed nerve, formed from the combination of nerve root fibers from its dorsal and ventral roots. The dorsal root is the afferent sensory root and carries sensory information to the brain. The ventral root is the efferent motor root and carries motor information from the brain. The spinal nerve emerges from the spinal column through an opening (intervertebral foramen) between adjacent vertebrae. This is true for all spinal nerves except for the first spinal nerve pair (C1), which emerges between the occipital bone and the atlas (the first vertebra).[3] Thus the cervical nerves are numbered by the vertebra below, except spinal nerve C8, which exists below vertebra C7 and above vertebra T1. The thoracic, lumbar, and sacral nerves are then numbered by the vertebra above. In the case of a lumbarized S1 vertebra (also known as L6) or a sacralized L5 vertebra, the nerves are typically still counted to L5 and the next nerve is S1.
Outside the vertebral column, the nerve divides into branches. The dorsal ramus contains nerves that serve the posterior portions of the trunk carrying visceral motor, somatic motor, and somatic sensory information to and from the skin and muscles of the back (
Some anterior rami merge with adjacent anterior rami to form a
Regional nerves
Cervical nerves

The cervical nerves are the spinal nerves from the cervical vertebrae in the cervical segment of the spinal cord. Although there are seven cervical vertebrae (C1–C7), there are eight cervical nerves C1–C8. C1–C7 emerge above their corresponding vertebrae, while C8 emerges below the C7 vertebra. Everywhere else in the spine, the nerve emerges below the vertebra with the same name.
The posterior distribution includes the suboccipital nerve (C1), the greater occipital nerve (C2) and the third occipital nerve (C3). The anterior distribution includes the cervical plexus (C1–C4) and brachial plexus (C5–T1).
The cervical nerves innervate the sternohyoid, sternothyroid and omohyoid muscles.
A loop of nerves called ansa cervicalis is part of the cervical plexus.
Thoracic nerves
The thoracic nerves are the twelve spinal nerves emerging from the thoracic vertebrae. Each thoracic nerve T1–T12 originates from below each corresponding
Anterior divisions
The intercostal nerves come from thoracic nerves T1–T11, and run between the ribs. At T2 and T3, further branches form the intercostobrachial nerve. The subcostal nerve comes from nerve T12, and runs below the twelfth rib.
Posterior divisions
The medial branches (ramus medialis) of the posterior branches of the upper six thoracic nerves run between the
The medial branches of the lower six are distributed chiefly to the multifidus and
Lumbar nerves

The lumbar nerves are the five spinal nerves emerging from the lumbar vertebrae. They are divided into posterior and anterior divisions.
Posterior divisions
The medial branches of the posterior divisions of the lumbar nerves run close to the articular processes of the vertebrae and end in the multifidus muscle.
The laterals supply the erector spinae muscles.
The upper three give off cutaneous nerves which pierce the aponeurosis of the
Anterior divisions
The anterior divisions of the lumbar nerves (rami anteriores) increase in size from above downward. They are joined, near their origins, by
The first and second, and sometimes the third and fourth lumbar nerves are each connected with the lumbar part of the sympathetic trunk by a white ramus communicans.
The nerves pass obliquely outward behind the psoas major, or between its
The first three and the greater part of the fourth are connected together in this situation by anastomotic loops, and form the lumbar plexus.
The smaller part of the fourth joins with the fifth to form the lumbosacral trunk, which assists in the formation of the sacral plexus. The fourth nerve is named the furcal nerve, from the fact that it is subdivided between the two plexuses.
Sacral nerves

The sacral nerves are the five pairs of spinal nerves which exit the
There are five paired sacral nerves, half of them arising through the sacrum on the left side and the other half on the right side. Each nerve emerges in two divisions: one division through the
The nerves divide into branches and the branches from different nerves join with one another, some of them also joining with lumbar or coccygeal nerve branches. These anastomoses of nerves form the sacral plexus and the lumbosacral plexus. The branches of these plexus give rise to nerves that supply much of the hip, thigh, leg and foot.[7][8]
The sacral nerves have both
Coccygeal nerves
The bilateral coccygeal nerves, Co, are the 31st pair of spinal nerves. It arises from the conus medullaris, and its ventral ramus helps form the coccygeal plexus. It does not divide into a medial and lateral branch. Its fibers are distributed to the skin superficial and posterior to the coccyx bone via the anococcygeal nerve of the coccygeal nerve plexus.
Function

| Level | Motor function |
|---|---|
| C1–C6 | flexors
|
| C1–T1 | extensors
|
| C3, C4, C5 | Supply diaphragm (mostly C4) |
| C5, C6 | Move shoulder, raise arm (deltoid); flex elbow (biceps) |
| C6 | externally rotate ( supinate ) the arm
|
| C6, C7 | pronate wrist
|
| C7, C8 | Flex wrist; supply small muscles of the hand |
| T1–T6 | |
L1
|
Abdominal muscles |
L4
|
Flex hip joint
|
L4
|
quadriceps femoris )
|
L5, S1
|
tibialis anterior); Extend toes
|
| Extend leg at the hip (gluteus maximus); flex foot and flex toes |
Spinal plexuses
A
Clinical significance
The muscles that one particular spinal root supplies are that nerve's
There are several procedures used in sacral nerve stimulation for the treatment of various related disorders.
Sciatica is generally caused by the compression of lumbar nerves L4, or L5 or sacral nerves S1, S2, or S3, or by compression of the sciatic nerve itself
Additional Images
-
A portion of the spinal cord, showing its right lateral surface. The dura is opened and arranged to show the nerve roots.
-
Distribution of the cutaneous nerves. Ventral aspect.
-
Distribution of the cutaneous nerves. Dorsal aspect.
-
The spinal cord with dura cut open, showing the exits of the spinal nerves.
-
The spinal cord showing how the anterior and posterior roots join in the spinal nerves.
-
A longer view of the spinal cord.
-
Projections of the spinal cord into the nerves (red motor, blue sensory).
-
Projections of the spinal cord into the nerves (red motor, blue sensory).
-
Schematic diagram of cervical plexus.
- Dissection images
-
Cerebrum. Inferior view. Deep dissection.
-
Cerebrum. Inferior view. Deep dissection.
-
Spinal nerves. Spinal cord and vertebral canal. Deep dissection.
See also
References
- ^ PMID 31194375.
- ^ "A Neurosurgeon's Overview of the Anatomy of the Spine and Peripheral Nervous System". www.aans.org. Retrieved 21 December 2023.
- ^ ISBN 9780071222075.
- ^ 1. Anatomy, descriptive and surgical: Gray's anatomy. Gray, Henry. Philadelphia : Courage Books/Running Press, 1974
- ^ 2. Clinically Oriented Anatomy. Moore, Keith L. Philadelphia : Wolters Kluwer Health/Lippincott Williams & Wilkins, 2010 (6th ed)
- ^ 1. Anatomy, descriptive and surgical: Gray's anatomy. Gray, Henry. Philadelphia : Courage Books/Running Press, 1974
- ^ 1. Anatomy, descriptive and surgical: Gray's anatomy. Gray, Henry. Philadelphia : Courage Books/Running Press, 1974
- ^ 3. Human Neuroanatomy. Carpenter, Malcolm B. Baltimore : Williams & Wilkins Co., 1976 (7th ed)
- ^ 3. Human Neuroanatomy. Carpenter, Malcolm B. Baltimore : Williams & Wilkins Co., 1976 (7th ed)
- Blumenfeld H. 'Neuroanatomy Through Clinical Cases'. Sunderland, Mass: Sinauer Associates; 2002.
- Drake RL, Vogl W, Mitchell AWM. 'Gray's Anatomy for Students'. New York: Elsevier; 2005:69-70.
- Ropper AH, Samuels MA. 'Adams and Victor's Principles of Neurology'. Ninth Edition. New York: McGraw Hill; 2009.