Cerebrospinal fluid leak
| Cerebrospinal fluid leak | |
|---|---|
| Other names | CSF leak |
 | |
| Circulation of CSF | |
 | |
| The meninges of the central nervous system impacted by CSF leak | |
| Specialty | Neurology |
A cerebrospinal fluid leak (CSF leak or CSFL) is a medical condition where the
A cerebrospinal fluid leak can be either cranial or spinal, and these are two different disorders.
Any CSF leak is most often characterized by orthostatic headaches, which worsen when standing, and improve when lying down. Other symptoms can include neck pain or stiffness, nausea, vomiting, dizziness, fatigue, and a metallic taste in the mouth. A CT myelography scan can identify the site of a cerebrospinal fluid leakage. Once identified, the leak can often be repaired by an epidural blood patch, an injection of the patient's own blood at the site of the leak, a fibrin glue injection, or surgery.
A spontaneous CSF leak is a rare condition, affecting at least one in 20,000 people and many more who go undiagnosed every year. On average, the condition develops at age 42, and women are twice as likely to be affected. Some people with a sCSF leak have a chronic leak despite repeated patching attempts, leading to long-term disability due to pain and being unable to be upright, and surgery is often needed. The symptoms of a spontaneous CSF leak were first described by German
Classification
Cerebrospinal fluid leaks are classified into two distinct disorders: cranial leaks, and spinal leaks.[10][11] Where there has been no preceding surgery or medical procedure that may have caused a CSF leak it is called a spontaneous CSF leak (sCSF leak).[12]
Cranial leak
Cranial leaks occur in the head, and in some of these cases, CSF can leak from one side of the nose, or from the ear.
Spinal leak
The vast majority of CSF leaks are spinal.
Spontaneous intracranial hypotension
Spontaneous intracranial hypotension (SIH) refers to lower than normal CSF volume due to a leak of CSF at the level of the spine.[18]
Spontaneous intracranial hypotension (SIH) is an important cause of longstanding headaches. Other symptoms can include nausea, blurred vision, coma, and dementia. SIH is typically secondary to a spontaneous spinal CSF leak.[17][14] Cranial CSF leaks do not cause SIH.[19] While this symptom can be referred to as intracranial hypotension, the intracranial pressure may be normal, with the underlying issue instead being low CSF volume, in this case a sCSFL may be referred to as CSF hypovolemia.[20][21][22][23]
Signs and symptoms
Spinal SCF leaks
| Nerve | Function | Symptoms |
|---|---|---|
| optic (2) |
optic nerve crossing |
blurred and or double vision |
| chorda tympani (Branch of 7) |
taste | taste distortion |
| facial (7) |
facial nerve | facial weakness and numbness |
| vestibulocochlear (8) |
hearing, balance |
hearing and balance problems |
| glossopharyngeal (9) |
taste | taste distortion |
The most common symptom of a spinal CSF leak is a fast-onset, extremely painful orthostatic headache.[23][25] This headache is usually made worse by standing and typically becomes prominent throughout the day, with the pain becoming less severe when lying down.[26] Orthostatic headaches can become chronic and disabling to the point of incapacitation.[23][27][28][29] Some people will develop headaches that begin in the afternoon. This is known as second-half-of-the-day headache. This may be an initial presentation of a spontaneous CSF leak or appear after treatment such as an epidural patch, and likely indicates a slow spinal CSF leak.[30] While high CSF pressure can make lying down unbearable, low CSF pressure due to a leak can be relieved by lying flat on the back.[31]
About 50% of people with a spinal CSFL experience neck pain or stiffness, nausea, and vomiting.[32]
Other symptoms of a CSF leak include
Aural symptoms are also present in many cases of intracranial hypotension due to CSF leak; including muffled hearing, pulsatile tinnitus, hearing loss.
Movement disorders are uncommon in spontaneous CSF leaks but occasionally can be one of the major components of the clinical presentation.[35]
Some cases of chronic intracranial hypotension due to CSF leak may present as personality changes, altered behaviors and impairment of executive functions, similar to behavioral-variant frontotemporal dementia as the frontal and temporal lobes are affected by downward sagging due to reduced intra-cranial pressures.[34]
An untreated CSF leak can result in coma or death as late stage findings as the brainstem herniates through the skull base or foramen magnum .[36][34]
Cranial CSF leaks
Cranial leaks occur in the skull. Symptoms often include a watery discharge including CSF from one side of the nose, or from the ear. There may also be a metallic taste in the mouth.[12]
Causes
A spontaneous spinal CSF leak refers to any CSF leak that has not been preceded by a surgical or other medical procedure.[12][29][37] Later evidence suggests that these leaks result from either a discogenic pathology, such as microspur, osteophyte or spinal disc herniation that pierces the dura like a knife, connective tissue disorder (which can often lead to discogenic pathology), or spinal drainage problems.[38][39]
A cerebrospinal fluid leak can be a rare complication of an anterior cervical discectomy and fusion. One study suggested a CSF leak to follow from 0.5% of operations.[40] Another study suggests a CSF leak to follow from 1% of operations. In most of these cases repair is successful.[41]
Discogenic causes
The most common cause of an intractable sCSF leak is
Connective tissue theory
Various scientists and physicians have suggested that sCSFLs may be the result of an underlying
Up to two thirds of those affected demonstrate some type of generalized connective tissue disorder.[24][43] Marfan syndrome, Ehlers–Danlos syndrome, and autosomal dominant polycystic kidney disease are the three most common connective tissue disorders associated with sCSFLs.[24] Roughly 20% of patients with a sCSFL exhibit features of Marfan syndrome, including tall stature, hollowed chest (pectus excavatum), joint hypermobility and arched palate. However, no other Marfan syndrome presentations are shown.[24]
Spinal drainage theory
Some studies have proposed that issues with the spinal venous drainage system may cause a CSF leak.[45] According to this theory, dural holes and intracranial hypotension are symptoms caused by low venous pressure in the epidural space. When leg muscles pump blood towards the heart, and pressure in the inferior vena cava vein becomes negative, the network of epidural veins is overdrained, causing CSF to be aspirated into the epidural space. True leaks can form at weak points in the spinal meninges. Therefore, the observed CSF hypotension is a result of CSF hypovolemia and reduced epidural venous pressure.[45]
Other causes
Cranial CSF leaks result from
CSF leaks can result from a lumbar puncture procedure.[50][51][52][53]
Complications
Several complications can occur as a result of sCSFLS including decreased cranial pressure, brain herniation, infection, blood pressure problems, transient paralysis, and coma. The primary and most serious complication of a spontaneous cerebrospinal fluid leak is spontaneous intracranial hypotension, where pressure in the brain is severely decreased.[23][42][54] This complication leads to the hallmark symptom of severe orthostatic headaches.[24][54]
People with cranial CSF leaks, the rarer form, have a 10% risk of developing meningitis per year.
Low CSF volume can cause the cerebellar tonsil position to descend, which can be mistaken for Chiari malformation; however when the CSF leak is repaired the tonsil position often returns to normal (as seen in upright MRI) in this "pseudo-Chiari" condition.[58] A further, albeit rare, complication of CSF leak is transient
There are documented cases of reversible frontotemporal dementia and coma.[61] Coma due to a CSF leak has been successfully treated by using blood patches and/or fibrin glue and placing the person in the Trendelenburg position.[62] Empty sella syndrome, a bony structure that surround the pituitary gland, occurs in CSF leak patients.[46][63]
Pathophysiology
Cerebrospinal fluid is produced by the choroid plexus in the ventricles of the brain and contained by the dura and arachnoid layers of the meninges.[23][42][64] The brain floats in CSF, which also transports nutrients to the brain and spinal cord. As holes form in the spinal dura mater, CSF leaks out into the surrounding space. The CSF is then absorbed into the spinal epidural venous plexus or soft tissues around the spine.[24][65] Due to the sterile conditions of the soft tissues around the spine, there is no risk of meningitis.[24]
Brain sagging
Lack of CSF pressure and volume can allow the brain to sag and descend through the
Diagnosis
Diagnosis of CSF leakage can be done by various imaging techniques, chemical
A clinical exam is often used as a means to diagnose CSF leaks. Improved patient response to conservative treatment may further define a positive diagnosis. The lack of clinician awareness of the signs -symptoms and ailments- of a CSF leak is the greatest challenge to proper diagnosis and treatment, in particular: the loss of the orthostatic characteristic of headache and that every chronic CSF leaker will have a unique symptom set that as a whole contributes to the underlying condition, and diagnosis of, a CSF leak.
The primary place of first complaint to a physician is a hospital emergency room.
CT
Diagnosis of a cerebrospinal fluid leak is performed through a combination of
MRI
There is disagreement over whether MRI should be the diagnostic tool of choice.
An alternate method of locating the site of a CSF leak is to use
Contrast-enhanced brain MRI with sagittal reformats can assess for the following:[6][8]
- Subdural fluid collections
- Enhancement of the meninges
- Engorgement of venous structures
- Pituitary swelling
- Sagging of the brain
For suspected spinal CSF leaks, spine imaging can be used to guide treatment.[8]
Assay
Fluid dripping from the nose (CSF rhinorrhoea) or ears (CSF otorrhea) should be collected and tested for the protein beta-2 transferrin which would be highly accurate in identifying CS fluid and diagnosing a cranial CSF leak.[71][55][72]
CSF analysis

Patients with CSF leaks have been noted to have very low or even negative opening pressures during lumbar puncture. However, patients with confirmed CSF leaks may also demonstrate completely normal opening pressures. In 18–46% of cases, the CSF pressure is measured within the normal range.[24][73][74][75] Analysis of spinal fluid may demonstrate lymphocytic pleocytosis and elevated protein content or xanthochromia. This is hypothesized to be due to increased permeability of dilated meningeal blood vessels and a decrease of CSF flow in the lumbar subarachnoid space.[24]
Myelography
A myelogram can be used to more precisely identify the location of a CSF leak by injecting a dye to further enhance the imaging. However, CSF leaks are frequently not visible on imaging.[citation needed]
For patients with recalcitrant spontaneous intracranial hypotension and no leak found on conventional spinal imaging, digital subtraction myelography, CT myelography and dynamic myelography (a modified conventional myelography technique) should be considered to rule out a CSF-venous fistula.[76][7] In addition, presence of a hyperdense paraspinal vein should be investigated in imaging as it is highly suggestive of a CSF venous fistula.[77]
Treatment
Symptomatic treatment usually involves
Epidural blood patch
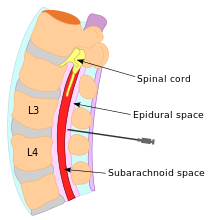
The treatment of choice for this condition is the surgical application of epidural blood patches,
Fibrin glue sealant
If blood patches alone do not succeed in closing the dural tears, placement of percutaneous fibrin glue can be used in place of blood patching, raising the effectiveness of forming a clot and arresting CSF leakage.[11][24][82]
Surgical drain technique
In extreme cases of intractable CSF leak, a surgical lumbar drain has been used.[83][84][85] This procedure is believed to decrease spinal CSF volume while increasing intracranial CSF pressure and volume.[83] This procedure restores normal intracranial CSF volume and pressure while promoting the healing of dural tears by lowering the pressure and volume in the dura.[83][85] This procedure has led to positive results leading to relief of symptoms for up to one year.[83][84]
Neurosurgical repair
Surgery to treat a CSF-venous fistula in CSF leak patients is highly effective.[86] Neurosurgery is available to directly repair leaking meningeal diverticula. The areas of dura leak can be tied together in a process called ligation and then a metal clip can be placed in order to hold the ligation closed.[24] Alternatively, a small compress called a pledget can be placed over the dura leak and then sealed with gel foam and fibrin glue.[24] Primary suturing is rarely able to repair a CSF leak, and in some patients exploration of the dura may be required to properly locate all sites of CSF leak.[24]
Adjunct measures
The use of
Prognosis
Long-term outcomes for people with sCSFLS remain poorly studied.[24] Symptoms may resolve in as little as two weeks, or persist for months.[32] Less commonly, patients may have unremitting symptoms for many years.[23][32][42][57] People with chronic sCSFLS may be disabled and unable to work.[24][28] Recurrent CSF leak at an alternate site after recent repair is common.[88]
Epidemiology
A 1994 community-based study indicated that two out of every 100,000 people with a sCSF, while a 2004
Studies have shown that sCSF leaks runs in families. It is suspected that genetic similarity in families includes weakness in the dura mater which leads to a sCSFL.[24][92] Large scale population-based studies have not yet been conducted.[42] While a majority of sCSF leaks continue to be undiagnosed or misdiagnosed, an actual increase in occurrence is unlikely.[42]
History
Spontaneous CSF leaks have been described by notable physicians and reported in medical journals dating back to the early 1900s.[93][94] German neurologist Georg Schaltenbrand reported in 1938 and 1953 what he termed "aliquorrhea", a condition marked by very low, unobtainable, or even negative CSF pressures. The symptoms included orthostatic headaches and other features that are now recognized as spontaneous intracranial hypotension. A few decades earlier, the same syndrome had been described in French literature as "hypotension of spinal fluid" and "ventricular collapse". In 1940, Henry Woltman of the Mayo Clinic wrote about "headaches associated with decreased intracranial pressure". The full clinical manifestations of intracranial hypotension and CSF leaks were described in several publications reported between the 1960s and early 1990s.[94] Modern reports of spontaneous CSF leak have been reported to medical journals since the late 1980s.[95]
Research
In three small studies of 1-2 patients with recurrent CSF leaks where repeated blood patches failed to form clots and relieve symptoms, the patients received temporary but complete resolution of symptoms with an epidural saline infusion.[98][99] The saline infusion temporarily restores the volume necessary for a patient to avoid SIH until the leak can be repaired properly.[24] Intrathecal saline infusion is used in urgent cases such as intractable pain or decreased consciousness.[24]
The gene
See also
References
- ^ MedlinePlus Encyclopedia: CSF leak
- PMID 35326296.
- ^ Cerebrospinal Fluid Leak Imaging at eMedicine
- PMID 29261908.
- ^ a b "Are all CSF leaks similar?". Spinal CSF Leak Foundation. 29 April 2018.
- ^ S2CID 5430158.
- ^ PMID 29023155.
- ^ S2CID 202812955.
- PMID 22929030.
- PMID 18710972.
- ^ S2CID 39157001.
- ^ a b c d "CSF leak (Cerebrospinal fluid leak) - Symptoms and causes". Mayo Clinic. Retrieved 16 January 2024.
- S2CID 201748704.
- ^ PMID 33393980.
- S2CID 44300449.
- PMID 35738670.
- ^ PMID 37676440.
- S2CID 247111571.
- S2CID 86400418.
- ISBN 978-0-86577-909-9. Retrieved 18 December 2009.
- ISBN 978-0-7817-4811-7. Retrieved 8 November 2010.
- PMID 10560599.
- ^ PMID 16859269.
- ^ S2CID 40813766.
- ^ PMID 17901290.
- PMID 19012477.
- ^ PMID 19495908.
- ^ S2CID 33678574.
- ^ ISBN 978-0-07-141620-7.
- S2CID 43308694.
- ^ "CSF Leak: A Curable Cause of Headache". www.cedars-sinai.edu. Archived from the original on 2018-08-01. Retrieved 2018-08-01.
- ^ S2CID 22162918.
- ^ S2CID 13544316.
- ^ S2CID 244829127.
- S2CID 3100453.
- ^ "Headache Secondary to Intracranial Hypotension, Schievink, W and Deline, C". www.researchgate.net. Retrieved 2018-09-22.
- S2CID 43132714.
- ^ .
- ^ PMID 31226967.
- PMID 32309668.
- S2CID 20105020.
- ^ PMID 16705110.
- ^ S2CID 21554078.
- S2CID 32994607.
- ^ S2CID 207609670.
- ^ S2CID 35820893.
- S2CID 39030096.
- S2CID 10793428.
- PMID 20157378.
- S2CID 71403201.
- ^ "Iatrogenic CSF Leaks from Lumbar Punctures – a commentary". 20 February 2015.
- ^ "Cerebrospinal Fluid (CSF) Leak: Symptoms & Treatment".
- ^ "Cerebrospinal Fluid Leak (CSF Leak) FAQ".
- ^ S2CID 30963142.
- ^ PMID 17767107.
- S2CID 24434779.
- ^ S2CID 36869290.
- ^ a b "Spontaneous Spinal Cerebrospinal Fluid Leaks: Diagnosis".
- S2CID 42704428.
- PMID 18726726.
- PMID 19378725.
- S2CID 2457796.
- S2CID 5350377.
- ISBN 978-3-13-142101-2. Retrieved 8 November 2010.
- PMID 16934734.
- ^ PMID 18071632.
- PMID 14676045.
- S2CID 19223351.
- ^ S2CID 9553904.
- S2CID 22189395.
- PMID 29455884.
- ^ "CSF Otorrhea: Practice Essentials, Epidemiology, Etiology". 28 November 2023. Retrieved 13 January 2024.
- S2CID 35100816.
- S2CID 43332925.
- ISBN 978-3-13-110886-9. Retrieved 8 November 2010.
- PMID 26849709.
- PMID 29217497.
- S2CID 19577501.
- PMID 18380287.
- S2CID 8388459.
- PMID 18809524.
- PMID 15200130.
- ^ S2CID 25817793.
- ^ PMID 2760094.
- ^ S2CID 6165146.
- PMID 31134267.
- PMID 25918919.
- PMID 14609162.
- S2CID 9548722.
- S2CID 19720469.
- PMID 19199465.
- PMID 19921558.
- PMID 13036182.
- ^ PMID 16859267.
- PMID 2709124.
- PMID 10638928.
- S2CID 43200053.
- PMID 19010507.
- S2CID 9552160.
- PMID 11883832.
