Buprenorphine
 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | bew-pre-nor-feen |
| Trade names | Subutex, Sublocade, Brixadi, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a605002 |
| License data | |
| Pregnancy category | |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | Sublingual: 30%[13] Intranasal: 48%[14] Buccal: 65%[15][16] |
| Protein binding | 96% |
| Metabolism | Liver (CYP3A4, CYP2C8) |
| Onset of action | Within 30 min[17] |
| Elimination half-life | 37 hours (range 20–70 hours) |
| Duration of action | Up to 24 hrs[17] |
| Excretion | Bile duct and kidney |
| Identifiers | |
| |
JSmol) | |
| |
| |
| | |
Buprenorphine, sold under the brand name Subutex among others, is an
In the United States, the combination formulation of
Side effects may include
Buprenorphine was patented in 1965, and approved for medical use in the United States in 1981.[17][23] It is on the World Health Organization's List of Essential Medicines.[24] In addition to prescription as an analgesic it is a common medication used to treat opioid use disorders, such as addiction to heroin.[25] In 2020, it was the 186th most commonly prescribed medication in the United States, with more than 2.8 million prescriptions.[26][27] Buprenorphine may also be used recreationally for the high it can produce.[25] In the United States, buprenorphine is a schedule III controlled substance.[25]
Medical uses
Opioid use disorder

Buprenorphine is used to treat people with
Before starting buprenorphine, individuals are generally advised to wait long enough after their last dose of opioid until they have some withdrawal symptoms to allow for the medication to bind the receptors, since if taken too soon, buprenorphine can displace other opioids bound to the receptors and precipitate an acute withdrawal. The dose of buprenorphine is then adjusted until symptoms improve, and individuals remain on a maintenance dose of 8–16 mg.[29]: 99–100 [31] Because withdrawal is uncomfortable and a deterrent for many patients, many have begun to call for different means of treatment initiation.[32] Some providers have begun to use the Bernese method, also known as microdosing, in which very small doses of buprenorphine are given while patients are still using street opioids, and without precipitating withdrawal, with medicine levels slowly titrated upward.[33][34]
Buprenorphine versus methadone
Both buprenorphine and
Chronic pain
A transdermal patch is available for the treatment of chronic pain.[17] These patches are not indicated for use in acute pain, pain that is expected to last only for a short period of time, or pain after surgery, nor are they recommended for opioid addiction.[40]
Potency
With respect to equianalgesic dosing, when used sublingually, the potency of buprenorphine is about 40 to 70 times that of morphine.[41][42][43] When used as a transdermal patch, the potency of buprenorphine may be 100 to 115 times that of morphine.[41][44]
Adverse effects
Common adverse drug reactions associated with the use of buprenorphine, similar to those of other opioids, include nausea and vomiting, drowsiness, dizziness, headache, memory loss, cognitive and neural inhibition, perspiration, itchiness, dry mouth, shrinking of the pupils of the eyes (miosis), orthostatic hypotension, male ejaculatory difficulty, decreased libido, and urinary retention. Constipation and central nervous system (CNS) effects are seen less frequently than with morphine.[46] Central sleep apnea has also been reported as a side effect of long-term buprenorphine use.[47][48]
Respiratory effects
The most severe side effect associated with buprenorphine is respiratory depression (insufficient breathing).[17] It occurs more often in those who are also taking benzodiazepines or alcohol, or have underlying lung disease.[17] The usual reversal agents for opioids, such as naloxone, may be only partially effective, and additional efforts to support breathing may be required.[17] Respiratory depression may be less than with other opioids, particularly with chronic use.[31] In the setting of acute pain management, though, buprenorphine appears to cause the same rate of respiratory depression as other opioids such as morphine.[49] Central sleep apnea is possible with long-term use, possibly resolving with dose reduction.[47][48]
Buprenorphine dependence
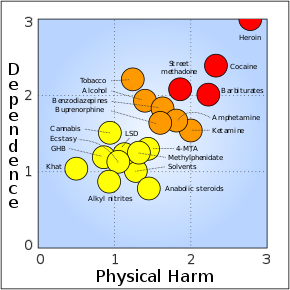
Buprenorphine treatment carries the risk of causing psychological or physiological (physical) dependencies. It has a slow onset of activity, with a long duration of action, and a long half-life of 24 to 60 hours. Once a patient has stabilised on the (buprenorphine) medication and programme, three options remain - continual use (buprenorphine-only medication), switching to a buprenorphine/naloxone combination, or a medically supervised withdrawal.[31]
Pain management
Achieving acute opioid
Pharmacology
Pharmacodynamics
| Site | Ki (nM) | Action | Species | Ref |
|---|---|---|---|---|
MOR |
0.7-2.3 0.081 |
Partial agonist | Human Monkey |
[53][54][55] [56] |
DOR |
2.9–6.1 0.82 |
Antagonist | Human Monkey |
[53][55][57] [56] |
KOR |
0.62–2.5 0.44 |
Antagonist | Human Monkey |
[53][55][57] [56] |
| NOP | 77.4 | Partial agonist | Human | [54][55][57] |
| σ1 | >100,000 | ND | ND | [58] |
| σ2 | ND | ND | ND | ND |
NMDA |
ND | ND | ND | ND |
| TLR4 | >10,000 | Agonist | Human | [59] |
| SERT | >100,000 | ND | Rat | [60] |
| NET | >100,000 | ND | Rat | [60] |
| DAT | ND | ND | ND | ND |
| VGSC | 33,000 (IC50) | Inhibitor | Rodent | [61] |
| Values are Ki (nM), unless otherwise noted. The smaller the value, the more strongly the drug binds to the site. | ||||
Opioid receptor modulator
Buprenorphine has been reported to possess these following
- μ-Opioid receptor (MOR): Very high affinity partial agonist:[62] at low doses, the MOR-mediated effects of buprenorphine are comparable to those of other narcotics, but these effects reach a "ceiling" as the receptor population is saturated.[57] This behavior is responsible for several unique properties: buprenorphine greatly reduces the effect of most other MOR agonists,[63] can cause precipitated withdrawal when used in actively opioid dependent persons,[63] and has a lower incidence of respiratory depression and fatal overdose relative to full MOR agonists.[64]
- Nociceptin receptor (NOP, ORL-1): Weak affinity, very weak partial agonist[62]
In simplified terms, buprenorphine can essentially be thought of as a nonselective, mixed
Although buprenorphine is a partial agonist of the MOR, human studies have found that it acts like a full agonist with respect to analgesia in opioid-intolerant individuals.
Buprenorphine is also known to bind to with high affinity and antagonize the putative
Full analgesic efficacy of buprenorphine requires both
The active metabolites of buprenorphine are not thought to be clinically important in its CNS effects.[74]
In positron emission tomography (PET) imaging studies, buprenorphine was found to decrease whole-brain MOR availability due to receptor occupancy by 41% (i.e., 59% availability) at 2 mg, 80% (i.e., 20% availability) at 16 mg, and 84% (i.e., 16% availability) at 32 mg.[79][80][81][82]
Other actions
Unlike some other opioids and opioid antagonists, buprenorphine binds only weakly to and possesses little if any activity at the sigma receptor.[83][84]
Buprenorphine also blocks voltage-gated sodium channels via the local anesthetic binding site, and this underlies its potent local anesthetic properties.[61]
Similarly to various other opioids, buprenorphine has also been found to act as an agonist of the toll-like receptor 4, albeit with very low affinity.[59]
Pharmacokinetics
Buprenorphine is
One of the major
The glucuronides of buprenorphine and norbuprenorphine are also biologically active, and represent major active metabolites of buprenorphine.[89] Buprenorphine-3-glucuronide has affinity for the MOR (Ki = 4.9 pM), DOR (Ki = 270 nM) and ORL-1 (Ki = 36 μM), and no affinity for the KOR. It has a small antinociceptive effect and no effect on respiration. Norbuprenorphine-3-glucuronide has no affinity for the MOR or DOR, but does bind to the KOR (Ki = 300 nM) and ORL-1 (Ki = 18 μM). It has a sedative effect but no effect on respiration.
Chemistry
Buprenorphine is a semisynthetic derivative of thebaine,[90] and is fairly soluble in water, as its hydrochloride salt.[91] It degrades in the presence of light.[91]
Detection in body fluids
Buprenorphine and norbuprenorphine may be quantified in blood or urine to monitor use or non-medical recreational use, confirm a diagnosis of poisoning, or assist in a medicolegal investigation. A significant overlap of drug concentrations exists in body fluids within the possible spectrum of physiological reactions ranging from asymptomatic to comatose. Therefore, having knowledge of both the route of administration of the drug and the level of tolerance to opioids of the individual is critical when results are interpreted.[92]
History
In 1969, researchers at Reckitt and Colman (now
Society and culture
Regulation
United States
In the United States, buprenorphine and buprenorphine with naloxone were approved for opioid use disorder by the Food and Drug Administration in October 2002.[96] The DEA rescheduled buprenorphine from a schedule V drug to a schedule III drug just before approval.[97] The ACSCN for buprenorphine is 9064, and being a schedule III substance, it does not have an annual manufacturing quota imposed by the DEA.[98] The salt in use is the hydrochloride, which has a free-base conversion ratio of 0.928.
In the years before buprenorphine/naloxone was approved, Reckitt Benckiser had lobbied Congress to help craft the Drug Addiction Treatment Act of 2000, which gave authority to the Secretary of Health and Human Services to grant a waiver to physicians with certain training to prescribe and administer schedule III, IV, or V narcotic drugs for the treatment of addiction or detoxification. Before this law was passed, such treatment was permitted only in clinics designed specifically for drug addiction.[99]
The waiver, which can be granted after the completion of an eight-hour course, was required for outpatient treatment of opioid addiction with buprenorphine from 2000 to 2021. Initially, the number of people each approved physician could treat was limited to 10. This was eventually modified to allow approved physicians to treat up to 100 people with buprenorphine for opioid addiction in an outpatient setting.[100] This limit was increased by the Obama administration, raising the number of patients to which doctors can prescribe to 275.[101] On 14 January 2021, the US Department of Health and Human Services announced that the waiver would no longer be required to prescribe buprenorphine to treat up to 30 people concurrently.[102]
New Jersey authorized paramedics to give buprenorphine to people at the scene after they have recovered from an overdose.[103]
Europe
In the European Union, Subutex and Suboxone, buprenorphine's high-dose sublingual tablet preparations, were approved for opioid use disorder treatment in September 2006.[104] In the Netherlands, buprenorphine is a list II drug of the Opium Law, though special rules and guidelines apply to its prescription and dispensation. In France, where buprenorphine prescription by general practitioners and dispensed by pharmacies has been permitted since the mid-1990s as a response to HIV and overdose risk. Deaths caused by heroin overdose were reduced by four-fifths between 1994 and 2002, and incidence of AIDS among people who inject drugs in France fell from 25% in the mid-1990s to 6% in 2010.[105]
Brand names
Buprenorphine is available under the trade names Cizdol, Brixadi (approved in the US by FDA for addiction treatment in 2023), Suboxone (with naloxone), Subutex (typically used for opioid use disorder), Zubsolv, Bunavail, Buvidal (approved in the UK, Europe and Australia for addiction treatment in 2018), Sublocade (approved in the US in 2018),
Research
Microdosing
There is some evidence that a buprenorphine microdosing regime, started before opioid withdrawal symptoms have started, can be effective in helping people transitioning away from opioid dependence.[109]
Depression
Some evidence supports the use of buprenorphine for depression.
Cocaine dependence
In combination with samidorphan or naltrexone (μ-opioid receptor antagonists), buprenorphine is under investigation for the treatment of cocaine dependence, and recently demonstrated effectiveness for this indication in a large-scale (n = 302) clinical trial (at a high buprenorphine dose of 16 mg, but not a low dose of 4 mg).[112][113]
Neonatal abstinence
Buprenorphine has been used in the treatment of the
Veterinary uses
Veterinarians administer buprenorphine for perioperative pain, particularly in cats, where its effects are similar to morphine. The drug's legal status and lower potential for human abuse makes it an attractive alternative to other opioids.[119]
It has veterinary medical use for treatment of pain in dogs and cats, as well as other animals.[120][121][122]
References
- ^ "Buprenorphine Use During Pregnancy". Drugs.com. 14 October 2019. Archived from the original on 10 November 2020. Retrieved 17 May 2020.
- ^ a b Australian Public Assessment Report for Buprenorphine (PDF) (Report). Therapeutic Goods Administration. November 2019. Archived (PDF) from the original on 20 March 2024.
- ISBN 9781455701506. Archivedfrom the original on 10 January 2023. Retrieved 16 February 2020.
- FDA. Retrieved 22 October 2023.
- ^ Anvisa (31 March 2023). "RDC Nº 784 - Listas de Substâncias Entorpecentes, Psicotrópicas, Precursoras e Outras sob Controle Especial" [Collegiate Board Resolution No. 784 - Lists of Narcotic, Psychotropic, Precursor, and Other Substances under Special Control] (in Brazilian Portuguese). Diário Oficial da União (published 4 April 2023). Archived from the original on 3 August 2023. Retrieved 16 August 2023.
- ^ "ARCHIVED - Report Stakeholder Workshop on a National Buprenorphine Program". Health Canada. 6 December 2004. Archived from the original on 26 March 2020. Retrieved 10 January 2020.
- ^ "Neurological therapies". Health Canada. 9 May 2018. Retrieved 13 April 2024.
- ^ "Subutex (buprenorphine sublingual tablets), CIII Initial U.S. Approval: 1981". DailyMed. Archived from the original on 27 May 2023. Retrieved 26 May 2023.
- ^ "Sublocade- buprenorphine solution". DailyMed. 15 March 2023. Archived from the original on 27 May 2023. Retrieved 26 May 2023.
- ^ "Butrans- buprenorphine patch, extended release". DailyMed. 26 June 2022. Archived from the original on 27 May 2023. Retrieved 26 May 2023.
- ^ "Brixadi- buprenorphine injection". DailyMed. 21 June 2023. Archived from the original on 26 June 2023. Retrieved 25 June 2023.
- ^ "FDA Approves New Buprenorphine Treatment Option for Opioid Use Disorder". U.S. Food and Drug Administration (Press release). 23 May 2023. Retrieved 26 May 2023.
- S2CID 31735116.
- S2CID 1286222.
- ^ "Buprenorphine / Naloxone Buccal Film (BUNAVAIL) C-III" (PDF). Pharmacy Benefits Management (PBM) Services. September 2014. Archived (PDF) from the original on 20 October 2020. Retrieved 10 February 2020.
- ^ "Bunavail (buprenorphine and naloxone buccal film), CIII Initial U.S. Approval: 2002". DailyMed. Archived from the original on 27 May 2023. Retrieved 26 May 2023.
- ^ a b c d e f g h i j k l m n o p q r s t "Buprenorphine Hydrochloride". drugs.com. American Society of Health-System Pharmacists. 26 January 2017. Archived from the original on 18 July 2017. Retrieved 17 March 2017.
- ^ "FDA approves first buprenorphine implant for treatment of opioid dependence". U.S. Food and Drug Administration (Press release). 26 May 2016. Archived from the original on 30 November 2017. Retrieved 12 December 2017.
- ^ PMID 33061915.
- PMID 22346191.
- ^ "Buprenorphine". The Substance Abuse and Mental Health Services Administration. 15 June 2015. Archived from the original on 26 August 2020. Retrieved 14 October 2020.
- ^ "Buprenorphine use while Breastfeeding". Drugs.com. Archived from the original on 10 November 2020. Retrieved 7 February 2021.
- ISBN 9783527607495. Archivedfrom the original on 10 January 2023. Retrieved 29 May 2020.
- hdl:10665/345533. WHO/MHP/HPS/EML/2021.02.
- ^ a b c "Buprenorphine". SAMHSA Center for Substance Abuse Treatment (CSAT). July 2019. Archived from the original on 20 August 2020. Retrieved 9 January 2020.
- ^ "The Top 300 of 2020". ClinCalc. Archived from the original on 12 February 2021. Retrieved 7 October 2022.
- ^ "Buprenorphine - Drug Usage Statistics". ClinCalc. Archived from the original on 11 October 2022. Retrieved 7 October 2022.
- ^ OCLC 1002302926.
- ^ OCLC 1002302926.
- ^ "Naloxone Hydrochloride". The American Society of Health-System Pharmacists. Archived from the original on 2 January 2015. Retrieved 2 January 2015.
- ^ a b c d "Buprenorphine". www.samhsa.gov. 31 May 2016. Archived from the original on 9 July 2021. Retrieved 3 December 2017.
- S2CID 245925947.
- PMID 27499655.
- S2CID 229721826.
- PMID 28220474.
- PMID 29112519.
Methadone is associated with increased risk of neonatal abstinence syndrome compared with buprenorphine in infants exposed in utero. This association is subject to minimal bias due to unmeasured confounding by severity of addiction.
- PMID 15204673.
- ^ Office of the Assistant Secretary for Health (OASH) (14 January 2021). "HHS Expands Access to Treatment for Opioid Use Disorder". HHS.gov. Archived from the original on 25 January 2022. Retrieved 5 January 2022.
- from the original on 14 October 2022. Retrieved 5 January 2022.
- ^ "Butrans Medication Guide". Butrans Medication Guide. Purdue Pharma L.P. Archived from the original on 14 July 2014. Retrieved 7 July 2014.
- ^ PMID 24995716.
- ^ "Drug Enforcement Administration (2005). "Ch. 4 Narcotics: Narcotics Treatment Drugs: Buprenorphine". Drugs of Abuse. U.S. Department of Justice. Archived from the original on 2 November 2006.
- ^ "Opioid Conversion Guide" (PDF). Department of Health, Government of Western Australia. February 2016. Archived (PDF) from the original on 18 April 2020. Retrieved 10 February 2020.
- PMID 26672499.
- S2CID 5903121.
- ISBN 3-13-134211-0
- ^ S2CID 251959885.
- ^ PMID 26312963.
- PMID 29576108.
- PMID 16418412.
- ^ Disha Mehta, Vinod Thomas, Jacinta Johnson, Brooke Scott, Sandra Cortina, Landon Berger. 2020 Continuation of Buprenorphine to Facilitate Postoperative Pain Management for Patients on Buprenorphine Opioid Agonist Therapy. 23;E163-E174. https://www.painphysicianjournal.com/current/pdf?article=NzAzMQ%3D%3D&journal=125 Archived 18 May 2023 at the Wayback Machine
- ^ Roth BL, Driscol J. "PDSP Ki Database". Psychoactive Drug Screening Program (PDSP). University of North Carolina at Chapel Hill and the United States National Institute of Mental Health. Archived from the original on 29 August 2021. Retrieved 14 August 2017.
- ^ PMID 9686407.
- ^ PMID 19713488.
- ^ PMID 24903063.
- ^ PMID 12409994.
- ^ PMID 18997874.
- ISBN 978-3-540-17471-4.
- ^ PMID 19679181.
- ^ PMID 7562497.
- ^ PMID 22504149.
- ^ PMID 31994020.
- ^ PMID 12481193.
- PMID 26672499.
- S2CID 214630021.
- PMID 32772054.
- PMID 19497337.
- ISBN 9780323445412. Archivedfrom the original on 14 January 2023. Retrieved 29 May 2020.
- PMID 572694.
- S2CID 8243410.
- ISBN 978-1-60547-277-5. Archivedfrom the original on 14 January 2023. Retrieved 14 March 2016.
- PMID 24484983.
- PMID 25518754.
- ^ S2CID 9977741.
- S2CID 54316989.
- S2CID 44036890.
- PMID 19077058.
- ^ Grinnell S et al. (2014): Buprenorphine analgesia requires exon 11-associated mu opioid receptor splice variants. The FASEB Journal
- ISBN 9780123983350.
- S2CID 27350905.
- S2CID 20773085.
- S2CID 46105421.
- ISBN 978-1-285-45717-8.
- ISBN 9780913595947.
- PMID 19773542.
- S2CID 11921738.
- PMID 11303059.
- ^ PMID 22739506.
- PMID 22037640.
- S2CID 19577410.
- ^ a b c "Buprenorphine". Martindale: The Complete Drug Reference. London, UK: Pharmaceutical Press. 14 January 2014. Archived from the original on 28 August 2021. Retrieved 6 April 2014.
- ISBN 978-0962652370.
- ^ "IMPORTANT SAFETY INFORMATION". Archived from the original on 18 March 2019. Retrieved 25 June 2016.
- S2CID 28395410.
- ^ Louis S. Harris, ed. (1998). Problems of Drug Dependence, 1998: Proceedings of the 66th Annual Scientific Meeting, The College on Problems of Drug Dependence, Inc (PDF). NIDA Research Monograph 179. Archived from the original (PDF) on 3 December 2016. Retrieved 5 August 2012.
- ^ McCormick CG (8 October 2002). "Subutex and Suboxone Approval Letter]" (PDF). Letter to Reckitt Benckiser. U.S. Food and Drug Administration.
- ^ 67 FR 62354, 7 October 2002
- ^ "Quotas – Conversion Factors for Controlled Substances". Deadiversion.usdoj.gov. Archived from the original on 2 March 2016. Retrieved 7 November 2016.
- ^ "Drug Addiction Treatment Act of 2000". SAMHSA, U.S. Department of Health & Human Services. Archived from the original on 4 March 2013.
- ^ "The National Alliance of Advocates for Buprenorphine Treatment". naabt.org. Archived from the original on 12 November 2020. Retrieved 19 May 2013.
- ^ "Obama administration's change on buprenorphine policy". Business Insider. 6 July 2016. Archived from the original on 18 March 2020. Retrieved 7 November 2016.
- ^ "HHS Expands Access to Treatment for Opioid Use Disorder". US Deptartment of Health and Human Services (Press release). 14 January 2021. Archived from the original on 14 January 2021. Retrieved 14 January 2021.
- ^ "In national first, N.J. program will let paramedics administer buprenorphine". STAT. 26 June 2019. Archived from the original on 3 October 2019. Retrieved 21 November 2019.
- ^ "Suboxone EU Approval". Ema.europa.eu. Archived from the original on 24 December 2016. Retrieved 7 November 2016.
- PMID 24623988.
- ^ "FDA approves first once-monthly buprenorphine injection, a medication-assisted treatment option for opioid use disorder". U.S. Food and Drug Administration (Press release). 30 November 2017. Archived from the original on 3 December 2017. Retrieved 5 December 2017.
- ^ "Indivior drug to fight opioid addiction approved by U.S. FDA". Reuters. 2017. Archived from the original on 5 December 2017. Retrieved 5 December 2017.
- ^ "Sublocade Now Available for Moderate-to-Severe Opioid Use Disorder". MPR. 1 March 2018. Archived from the original on 23 September 2019. Retrieved 23 September 2019.
- S2CID 229721826.
- PMID 28483102.
- S2CID 4633923.
- PMID 26948856.
- ^ "Alkermes Presents Positive Clinical Data of ALKS 5461 at 52nd Annual New Clinical Drug Evaluation Unit Meeting". Reuters. 2012. Archived from the original on 24 September 2015. Retrieved 30 June 2017.
- PMID 18694901.
- PMID 23036249.
- ^ Clinical trial number NCT00521248 for "Buprenorphine for the Treatment of Neonatal Abstinence Syndrome" at ClinicalTrials.gov
- S2CID 13772333.
Currently, methadone and buprenorphine are both widely used as the backbone of MAT [medication-assisted treatment]. The distinguishing outcomes in studies among these two opioid agonists are that infants exposed to buprenorphine in clinical trials required shorter treatment duration, less medication to treat the NAS symptoms and experienced shorter hospitalizations compared to infants exposed to methadone. A caveat to these findings is that some of the supporting data were based on using buprenorphine in combination with naloxone instead of buprenorphine as a single agent.
- PMID 22768012.
- ^ Martinez M (May 2014). "Options in perioperative analgesia: buprenorphine v. methadone". Veterinary Practice. Archived from the original on 19 January 2022. Retrieved 19 January 2022.
- ^ Claude A (June 2015). "Buprenorphine" (PDF). cliniciansbrief.com. Archived from the original (PDF) on 16 May 2017. Retrieved 25 February 2017.
- ISBN 9781118685907. Archivedfrom the original on 1 May 2023. Retrieved 25 December 2021.
- PMID 32448336.
External links
- McGray D (1 April 2005). "The bitter pill". Wired.
- Wood G (7 May 2013). "Subu Must Die – How a nation of junkies went cold turkey". New Republic.
