Sudden arrhythmic death syndrome
| Sudden arrhythmic death syndrome | |
|---|---|
| Other names | Sudden adult death syndrome (SADS), bed death, sudden unexpected/unexplained death syndrome (SUDS), sudden unexpected/unexplained nocturnal death syndrome (SUNDS), Sudden Death Syndrome, Sudden Death, Delayed Death |
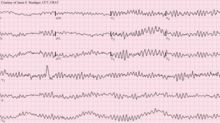 | |
| A type of a deadly ventricular arrhythmia - Ventricular fibrillation pattern seen on an ECG | |
| Specialty | Cardiology |
| Causes |
|
| Risk factors | Family history of heart disease[1], Asian ancestry[2], Primary arrhythmia, atherosclerosis[3], type 1 diabetes[4] |
| Frequency | 14.9 per 100,000 people in Japan 110.8 per 100,000 people in United States[5] |
Sudden arrhythmic death syndrome (SADS) is a sudden unexpected death of adolescents and adults caused by, as the name implies, a cardiac arrest. However, the exact cause of the cardiac arrest, and thus the exact cause of death, may not be found. These deaths occur mainly during sleep or at rest.[6] One type of conduction defect known as Brugada syndrome can be responsible.[7][8]
The syndrome is rare in most areas around the world but occurs in populations that are culturally and genetically distinct. It was first noted in 1977 among southeast Asian Hmong refugees in the United States and Canada.[9][10] The syndrome was again noted in Singapore when a retrospective review of records showed that 230 otherwise healthy Thai foreign workers living in Singapore died suddenly of unexplained causes between 1982 and 1990.[11]
Causes
Sudden death of a young person can be caused by heart disease (including
In young people with type 1 diabetes, unexplained deaths could be due to nighttime hypoglycemia triggering abnormal heart rhythms or cardiac autonomic neuropathy, damage to nerves that control the function of the heart.[4]
Medical examiners have taken into account various factors, such as nutrition, toxicology, heart disease, metabolism, and genetics. Although there is no real known definite cause, extensive research showed victims aged 18 or older were found to have had a
In the Philippines, sudden adult death syndrome (or in their term, bangungot) is mainly caused by the Brugada syndrome.[13]
Diagnosis
By definition, the diagnosis can only occur post-mortem after other causes are ruled out.
Prevention
A 2011 retrospective cohort study using demographic and autopsy data for a 10-year period comprising 15.2 million person-years of active surveillance suggested prevention of sudden death in young adults should focus on evaluation for causes known to be associated with SCD (e.g., primary arrhythmia) among persons less than 35 years old, and emphasise atherosclerotic coronary disease in those older.[3]
A 2003 study found that the only proven way to prevent SADS is with an implantable cardioverter-defibrillator. Oral beta-blockers such as propranolol are ineffective.[14]
Epidemiology
In 1980, a reported pattern of sudden deaths was brought to the attention of the
In a 2008 study it was found that over half of SADS deaths could be attributed to inherited heart disease: unexplained premature sudden deaths in family, long QT syndrome, Brugada syndrome, arrhythmogenic right ventricular cardiomyopathy and others.[1]
A national SADS study in England, funded by the British Heart Foundation, reported results in a 2007 journal article published in Health.[15] The study surveyed 117 coroners' jurisdictions in England. Researchers found that deaths from SADS reported by these coroners occurred "predominantly in young males". There were 500 cases a year in England, eight times more than had previously been estimated. Families are more at risk of SADS if they have a genetic cardiac disease. The study recommended that affected families should undergo "specialised cardiological evaluation".[15]
Asia
Southeast Asian immigrants, who were mostly fleeing the
History

Laotian Hmongs were chosen for the study because they had one of the highest sudden death rates in the United States while sleeping. They were originally from Southern China and the highlands of North Vietnam, Laos, and Thailand. The location that was picked for this study was in
An interview was arranged with the next of kin who lived with them, witnessed the death, or found the body. The interviews were open ended and allowed the person who was next of kin to describe what they witnessed and what preceding events they thought were relevant to the victim's death. The interviewers also collected information such as illness history, the circumstances of the death, demographic background, and history of any sleep disturbances. A genealogy was then created which included all the relatives and their vital status and/or circumstances of death.[2]
Society, culture, superstition
During the 1970s and 1980s, when an outbreak of this syndrome began, many Southeast Asians were not able to worship properly due to the Laotian Civil War. Hmong people believe that when they do not worship properly, do not perform religious rituals properly or forget to sacrifice, the ancestor spirits or the village spirits do not protect them, thus allowing evil spirits to reach them. These attacks induce a nightmare that leads to sleep paralysis, in which the victim is conscious and experiencing pressure on the chest.[16] It is also common to have a REM state that is out of sequence, where there is a mix of brain states that are normally held separate.[16] After the war, the United States government scattered the Hmong refugees across the U.S. in 53 different cities.[16] Once these nightmare visitations began, a shaman was recommended for psychic protection from the spirits of their sleep.[16] However, scattered across 53 different cities, these victims had no access to a shaman who could protect them.
Hmong people believed that rejecting the role of becoming a
The study author suggested that the Hmong who died were killed by their own beliefs in the spiritual world, otherwise known as Nocturnal pressing spirit attacks. In Indonesia it is called digeuton, which translates to "pressed on" in English.[16] In China it is called bèi guǐ yā (traditional Chinese: 被鬼壓; simplified Chinese: 被鬼压) which translates to "crushed by a ghost" in English.[16] The Dutch call the presence a nachtmerrie, the night-mare.[16] The "merrie" comes from the Middle Dutch mare, an incubus who "lies on people's chests, suffocating them". This phenomenon is known among the Hmong people of Laos,[19] who ascribe these deaths to a malign spirit, dab tsuam (pronounced "dah chua"), said to take the form of a jealous woman.
Bangungot is depicted in the Philippines as a mythological creature called batibat or bangungot.[20] This hag-like creature sits on the victim's face or chest so as to immobilize and suffocate him. When this occurs, the victim is usually experiencing sleep paralysis.
This phenomenon inspired the
English names
| Name | Acronym | Notes |
|---|---|---|
| sudden unexpected death syndrome | SUDS | |
| sudden unexplained death syndrome | SUDS | |
| sudden unexpected nocturnal death syndrome | SUNDS | |
| sudden unexplained nocturnal death syndrome | SUNDS | |
| sudden adult death syndrome | SADS | (parallel in form with SIDS )
|
| sudden arrhythmia death syndrome | SADS | |
| sudden arrhythmic death syndrome | SADS | |
| sudden arrhythmic cardiac death syndrome | — | |
| bed death | — |
Names in other languages
| Term | Language | Notes |
|---|---|---|
| lai tai | Thai | Thai: ใหลตาย; meaning "sleep and die"[17][21] |
| bangungot or urom | Filipino | The term originated from the Tagalog word meaning "to rise and moan in sleep".[22] It is also the Tagalog word for nightmare. |
| dab tsog | Hmong[19] | dab tsog means "ghost" |
| dolyeonsa | Korean | Korean: 돌연사; meaning literally "sudden death" |
| pokkuri disease | Japanese[23] | |
| jathoom[citation needed] | Arabic | جاثوم |
| albarsty (Kyrgyz: албарсты) | Kyrgyz |
See also
- Brugada syndrome
- Night hag
- Sleep paralysis
- Sudden infant death syndrome
- Sudden unexpected death in epilepsy
- Sudden unexplained death in childhood
- Yunnan sudden death syndrome
References
- ^ PMID 18508782.
- ^ PMID 3618851.
- ^ PMID 21903060.
- ^ a b "Dead in bed syndrome - a term used to describe the sudden unexplained deaths of young people with type 1 diabetes". Diabetes. 10 June 2022 [Originally written 15 January 2019].
- S2CID 203506307.
- ^ Also known as SUDS. See: Reddy PR, Reinier K, Singh T, Mariani R, Gunson K, Jui J, Chugh SS. Physical activity as a trigger of sudden cardiac arrest: The Oregon Sudden Unexpected Death Study. Int J Cardiol. 2008
- ^ "Brugada Syndrome". NORD (National Organization for Rare Disorders). 2016. Retrieved 28 October 2017.
- ^ "Brugada syndrome". Genetics Home Reference. Retrieved 28 October 2017.
- PMID 6796814.
- PMID 3110586.
- S2CID 46669256.
- ^ a b c Elijah R Behr (2010). When a young person dies suddenly (PDF) (4 ed.). Cardiac Risk in the Young - CRY. Archived from the original on 20 July 2014.
- ^ Tessa R. Salazar (19 June 2004). "Bangungot' in family? See a heart specialist". Inquirer News Service. Archived from the original on 30 June 2004.
- PMID 12695290.
- ^ PMID 17237131. Retrieved 5 June 2022.
- ^ a b c d e f g h Madrigal, Alexis C. (14 September 2011). "The Dark Side of the Placebo Effect: When Intense Belief Kills". The Atlantic. Retrieved 24 April 2016.
- PMID 8449651.
- ^ PMID 7660175.
- ^ "BATIBAT | BANGUNGOT - Frightened To Death By Nightmares • THE ASWANG PROJECT". THE ASWANG PROJECT. 16 February 2016. Retrieved 17 February 2021.
- PMID 17124999.
- PMID 9758125. Archived from the original(PDF) on 30 September 2015.
- PMID 966364.
Further reading
- Agence France Presse (8 April 2002). "Sleeping death syndrome terrorises young men". The Borneo Post.
- Center for Disease Control (23 September 1988). "Sudden Unexplained Death Syndrome Among Southeast Asian Refugees". MMWR.
