Taenia saginata
| Taenia saginata | |
|---|---|
| |
| Scientific classification | |
| Domain: | Eukaryota |
| Kingdom: | Animalia |
| Phylum: | Platyhelminthes |
| Class: | Cestoda |
| Order: | Cyclophyllidea |
| Family: | Taeniidae |
| Genus: | Taenia |
| Species: | T. saginata
|
| Binomial name | |
| Taenia saginata Goeze, 1782
| |
Taenia saginata (synonym Taeniarhynchus saginatus), commonly known as the beef tapeworm, is a
T. saginata has a strong resemblance to the other human tapeworms, such as
Description
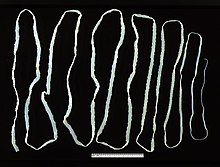
T. saginata is the largest of species in the
T. saginata does not have a
Life cycle
Intermediate host
Cattle acquire the embryonated eggs, the oncospheres, when they eat contaminated food. Oncospheres enter the
Definitive host

Humans contract infective cysticerci by eating raw or undercooked meat. Once reaching the
Genome
Epidemiology
The disease is relatively common in Africa, some parts of Eastern Europe, the Philippines, and Latin America.[2] There is also a widespread occurrence of the parasite throughout East, Southeast, and South Asia.[8] This parasite is found anywhere where beef is eaten, including countries such as the United States, with strict federal sanitation policies. In the US, the incidence of infection is low, but 25% of cattle sold are still infected.[6] However, not all slaughterhouses are federally inspected.[9] The total global infection is estimated to be between 40 and 60 million.[1] It is most prevalent in Sub-Saharan Africa and the Middle East.[7]
Religious beliefs may also play a role in infection rates. In India, Muslims can have a higher rate of infection compared to Hindus, who do not eat beef.[9]
Infection
Symptoms
T. saginata infection is usually
The Taenia saginata remains asymptomatic due to the fact the organism does not present cysticerci in humans. Therefore, there is no presence of cysticercosis in humans either. Typically, cysticercosis is a parasitical tissue infection which infect the brain and muscle tissues. However the Taenia saginata can cause taeniasis, which is an infection. Taeniasis causes weight loss, pain and blockages in the intestines which can potentially become life-threatening.[14]
Diagnosis
The basic diagnosis is done from a stool sample. Feces are examined to find parasite eggs. The eggs look like other eggs from the family Taeniidae, so it is only possible to identify the eggs to the family, not to the species level. Since it is difficult to diagnose using eggs alone, looking at the scolex or the gravid proglottids can help identify it as Taenia saginata.[6] Proglottids sometimes trickle down the thighs of infected humans and are visible with unaided eye, so can aid with identification. Observation of scolex help distinguish between T. saginata, T. solium and T. asiatica. When the a tapeworm's uterus is injected with India ink, its branches become visible. Counting the uterine branches enables some identification (T. saginata uteri have 12 or more branches on each side, while other species such as T. solium only have five to 10).[2]
Differentiation of the species of
Eosinophilia and elevated IgE levels are chief hematological findings. Also Ziehl–Neelsen stain can be used to differentiate between mature T. saginata and T. solium, in most cases T. saginata will stain while T. solium will not, but the method is not strictly reliable.[17]
Prevention
Adequate cooking at 56 °C (133 °F) for 5 minutes of beef viscera destroys cysticerci. Refrigeration, freezing at −10 °C (14 °F) for 9 days or long periods of salting is lethal to cysticerci. Inspection of beef and proper disposal of human excreta are also important measures.[10]
Treatment
Taeniasis is easily treated with
See also
- List of parasites (human)
References
- ^ ISBN 9781588902450.
- ^ ISBN 9780071628792.
- ^ ISBN 9780124159150.
- ^ ISBN 9780781730143.
- PMID 17907306.
- ^ ISBN 978-0-07-128458-5.
- ^ ISBN 9780387311975.
- PMID 32381027.
- ^ ISBN 978-0-07-352419-1.
- ^ a b c "Taeniasis/Cysticercosis". WHO Fact sheet no. 376. World Health Organization. 2013. Retrieved 7 February 2014.
- PMID 23340150.
- ^ Hendrickx, Emilie, et al. "Epidemiology of Taenia Saginata Taeniosis/Cysticercosis: A Systematic Review of the Distribution in West and Central Africa." Parasites & Vectors, vol. 12, no. 1, 2019, doi:10.1186/s13071-019-3584-7.
- ^ "Taeniasis/Cysticercosis." World Health Organization, World Health Organization, www.who.int/news-room/fact-sheets/detail/taeniasis-cysticercosis.
- ISBN 978-3662439777.
- PMID 10655377.
- PMID 1822899.
- PMID 20579318.
- PMID 24309372.
- ^ "Clinical Aspects and Treatment of the More Common Intestinal Parasites of Man (TB-33)". Veterans Administration Technical Bulletin 1946 & 1947. 10: 1–14. 1948.
