Taeniasis
| Taeniasis | |
|---|---|
stool samples[4] | |
| Prevention | Properly cooking meat[1] |
| Treatment | Praziquantel, niclosamide[1] |
| Frequency | 50 million (with cysticercosis)[5] |
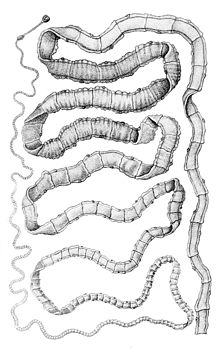
Taeniasis is an
Types of Taenia that cause infections in humans include
Prevention is by properly cooking meat.[1] Treatment is generally with praziquantel, though niclosamide may also be used.[1] Together with cysticercosis, infections affect about 50 million people globally.[5] The disease is most common in the developing world.[1] In the United States less than 1,000 cases occur a year.[1]
Signs and symptoms
Taeniasis generally has few or no symptoms.[6] It takes about 8 weeks from infection for adult worms to form and can last for years without treatment.[6]
Infection may be suspected when a portion of the worm is passed in the stool.[4] It is not generally fatal.[7][8][9]
Pork tapeworm
Infection in the intestines by the adult T. solium worms is normally asymptomatic. Heavy infection can result in
A complication, known as
Beef tapeworm
Taenia saginata infection is usually asymptomatic, but heavy infection causes weight loss,
Asian tapeworm
Transmission
Taeniasis is contracted after eating undercooked pork or beef that contain the
If consumed by an
Cysticercosis occurs when contaminated food, water, or soil that contain T. solium eggs is eaten.[14][15]
Diagnosis

To date the most relevant test for T. asiatica is by
Prevention
Prevention efforts include properly cooking meat, treating active cases in humans, vaccinating and treating pigs against the disease, stricter meat-inspection standards, health education, improved sanitation, and improved pig raising practices.[1][6]
Preventing human faeces from contaminating pig feeds also plays a role. Infection can be prevented with proper disposal of human faeces around pigs, cooking meat thoroughly and/or freezing the meat at −10 °C for 5 days. For human cysticercosis, contaminated hands are the primary cause, and especially concerning among food handlers.[7]
Proper cooking of meat is an effective prevention. For example, cooking (56 °C for 5 minutes) of beef
Treatment
Praziquantel is the treatment of choice.[22] Usual treatments are with praziquantel (5–10 mg/kg, single-administration) or niclosamide (adults and children over 6 years: 2 g, single-administration after a light breakfast, followed after 2 hours by a laxative; children aged 2–6 years: 1 g; children under 2 years: 500 mg).[11] One study showed albendazole is effective against animal beef tapeworm cysticercosis.[23] Mepacrine is quite effective but has adverse effects in humans.[24]
Epidemiology
The total global infection is estimated to be between 40 and 60 million people.[25] In the US, the incidence of infection is low, but 25% of cattle sold are still infected.[16]
Regions
Taeniasis is predominantly found in Asia, Africa, Latin America, particularly on farms in which pigs are exposed to human excrement. At a low level though, it occurs everywhere where beef and pork are eaten, even in countries with strict sanitation policies such as the United States. Taenia saginata is relatively common in Africa, some parts of Eastern Europe,[26] the Philippines, and Latin America.[27] It is most prevalent in Sub-Saharan Africa and the Middle East.[28] Taenia asiatica is restricted to East Asia, including Taiwan, Korea, Indonesia, Nepal, Thailand and China.[29][30]
See also
- Tapeworm infection
References
- ^ a b c d e f g h i j k l m n "CDC - Taeniasis - General Information - Frequently Asked Questions (FAQs)". www.cdc.gov. 24 April 2019. Retrieved 16 December 2019.
- ^ a b c d e f "CDC - Taeniasis". www.cdc.gov. 24 April 2019. Retrieved 16 December 2019.
- ^ a b "CDC - Taeniasis - Biology". www.cdc.gov. 24 April 2019. Retrieved 16 December 2019.
- ^ a b c "CDC - Taeniasis - Diagnosis". www.cdc.gov. 24 April 2019. Retrieved 17 December 2019.
- ^ ISBN 978-0-12-381507-1.
- ^ a b c "Taeniasis/Cysticercosis". www.who.int. Retrieved 17 December 2019.
- ^ ISBN 978-3-642-39021-0.)
{{cite book}}: CS1 maint: multiple names: authors list (link - ^ "About Taeniasis/cysticercosis". Archived from the original on March 14, 2014. Retrieved 13 March 2014.
- ^ "Signs, symptoms and treatment of taeniasis/cysticercosis". Archived from the original on March 14, 2014. Retrieved 13 March 2014.
- S2CID 25698465.
- ^ a b c "Taeniasis/Cysticercosis". WHO Fact sheet N°376. World Health Organization. 2013. Retrieved 7 February 2014.
- PMID 23340150.
- PMID 18752896.
- ISBN 978-0-07-302827-9.
- ^ "Transmission of taeniasis/cysticercosis". Archived from the original on March 14, 2014. Retrieved 13 March 2014.
- ^ ISBN 978-0-07-128458-5.
- PMID 10655377.
- PMID 1822899.
- PMID 20579318.
- PMID 20631114.
- PMID 19290097.
- ^ "CDC - DPDX Homepage". 2019-05-14. Archived from the original on 2013-07-10. Retrieved 2014-11-28.
- PMID 24309372.
- PMID 23467308.
- ISBN 9781588902450.
- PMID 30376899.
- ISBN 9780071628792.
- ISBN 9780387311975.
- PMID 19885327.
- PMID 24450957.
