Thyroid
| Thyroid | |
|---|---|
Inferior thyroid veins | |
| Identifiers | |
| Latin | glandula thyreoidea |
| MeSH | D013961 |
| TA98 | A11.3.00.001 |
| TA2 | 3863 |
| FMA | 9603 |
| Anatomical terminology] | |
The thyroid, or thyroid gland, is an
Thyroid disorders include
Structure
Features
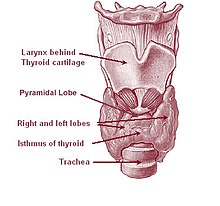
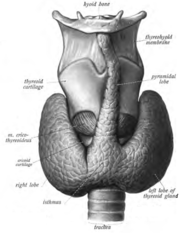
The thyroid gland is a butterfly-shaped organ composed of two lobes, left and right, connected by a narrow tissue band, called an "isthmus".[4] It weighs 25 grams in adults, with each lobe being about 5 cm long, 3 cm wide, and 2 cm thick and the isthmus about 1.25 cm in height and width.[4] The gland is usually larger in women than in men, and increases in size during pregnancy.[4][5]
The thyroid is near the front of the neck, lying against and around the front of the
The thyroid gland is covered by a thin fibrous capsule,[4] which has an inner and an outer layer. The inner layer extrudes into the gland and forms the septa that divide the thyroid tissue into microscopic lobules.[4] The outer layer is continuous with the pretracheal fascia, attaching the gland to the cricoid and thyroid cartilages[5] via a thickening of the fascia to form the posterior suspensory ligament of thyroid gland, also known as Berry's ligament.[5] This causes the thyroid to move up and down with the movement of these cartilages when swallowing occurs.[5]
Blood, lymph and nerve supply
The thyroid is supplied with arterial blood from the superior thyroid artery, a branch of the external carotid artery, and the inferior thyroid artery, a branch of the thyrocervical trunk, and sometimes by an anatomical variant the thyroid ima artery,[4] which has a variable origin.[10] The superior thyroid artery splits into anterior and posterior branches supplying the thyroid, and the inferior thyroid artery splits into superior and inferior branches.[4] The superior and inferior thyroid arteries join behind the outer part of the thyroid lobes.[10] The venous blood is drained via superior and middle thyroid veins, which drain to the internal jugular vein, and via the inferior thyroid veins. The inferior thyroid veins originate in a network of veins and drain into the left and right brachiocephalic veins.[4] Both arteries and veins form a plexus between the two layers of the capsule of the thyroid gland.[10]
Variation
There are many variants in the size and shape of the thyroid gland, and in the position of the embedded parathyroid glands.[5]
Sometimes there is a third lobe present called the pyramidal lobe.
Other variants include a levator muscle of thyroid gland, connecting the isthmus to the body of the hyoid bone,[5] and the presence of the small thyroid ima artery.[5]
Microanatomy

At the
- Follicles
Thyroid follicles are small spherical groupings of cells 0.02–0.9mm in diameter that play the main role in thyroid function.[4] They consist of a rim that has a rich blood supply, nerve and lymphatic presence, that surrounds a core of colloid that consists mostly of thyroid hormone precursor proteins called thyroglobulin, an iodinated glycoprotein.[4][15]
- Follicular cells
The core of a follicle is surrounded by a single layer of follicular cells. When stimulated by thyroid stimulating hormone (TSH), these secrete the thyroid hormones T3 and T4. They do this by transporting and metabolising the thyroglobulin contained in the colloid.[4] Follicular cells vary in shape from flat to cuboid to columnar, depending on how active they are.[4][15]
- Follicular lumen
The follicular lumen is the fluid-filled space within a follicle of the thyroid gland. There are hundreds of follicles within the thyroid gland. A follicle is formed by a spherical arrangement of
- Parafollicular cells
Scattered among follicular cells and in spaces between the spherical follicles are another type of thyroid cell, parafollicular cells.[4] These cells secrete calcitonin and so are also called C cells.[17]
Development

In the
The
The neuroendocrine parafollicular cells, also known as C cells, responsible for the production of calcitonin, are derived from foregut endoderm. This part of the thyroid then first forms as the ultimopharyngeal body, which begins in the ventral fourth pharyngeal pouch and joins the primordial thyroid gland during its descent to its final location.[23]
Aberrations in
Function
Thyroid hormones
The primary function of the thyroid is the production of the iodine-containing
- Metabolic. The thyroid hormones increase the free fatty acids.[28] Despite increasing free fatty acids, thyroid hormones decrease cholesterol levels, perhaps by increasing the rate of secretion of cholesterol in bile.[28]
- Cardiovascular. The hormones increase the rate and strength of the heartbeat. They increase the rate of breathing, intake and consumption of oxygen, and increase the activity of
- Developmental. Thyroid hormones are important for normal development.[28] They increase the growth rate of young people,[29] and cells of the developing brain are a major target for the thyroid hormones T3 and T4. Thyroid hormones play a particularly crucial role in brain maturation during fetal development and first few years of postnatal life[28]
- The thyroid hormones also play a role in maintaining normal sexual function, sleep, and thought patterns. Increased levels are associated with increased speed of thought generation but decreased focus.[27] Sexual function, including libido and the maintenance of a normal menstrual cycle, are influenced by thyroid hormones.[27]
After secretion, only a very small proportion of the thyroid hormones travel freely in the blood. Most are bound to thyroxine-binding globulin (about 70%), transthyretin (10%), and albumin (15%).[30] Only the 0.03% of T4 and 0.3% of T3 traveling freely have hormonal activity.[31] In addition, up to 85% of the T3 in blood is produced following conversion from T4 by iodothyronine deiodinases in organs around the body.[24]
Thyroid hormones act by crossing the
Hormone production
The thyroid hormones are created from
When the follicular cells are stimulated by thyroid-stimulating hormone, the follicular cells reabsorb thyroglobulin from the follicular lumen. The iodinated tyrosines are cleaved, forming the thyroid hormones T4, T3, DIT, MIT, and traces of reverse triiodothyronine. T3 and T4 are released into the blood. The hormones secreted from the gland are about 80–90% T4 and about 10–20% T3.[36][37] Deiodinase enzymes in peripheral tissues remove the iodine from MIT and DIT and convert T4 to T3 and RT3. [34] This is a major source of both RT3 (95%) and T3 (87%) in peripheral tissues.[38]
Regulation
The production of thyroxine and triiodothyronine is primarily regulated by thyroid-stimulating hormone (TSH), released by the
TRH is secreted at an increased rate in situations such as cold exposure in order to stimulate thermogenesis.[41] In addition to being suppressed by the presence of thyroid hormones, TSH production is blunted by dopamine, somatostatin, and glucocorticoids.[42]
Calcitonin
The thyroid gland also produces the hormone
Gene and protein expression
About 20,000
Clinical significance
Functional disorders
Hyperthyroidism
Excessive production of the thyroid hormones is called hyperthyroidism. Causes include Graves' disease, toxic multinodular goitre, solitary thyroid adenoma, inflammation, and a pituitary adenoma which secretes excess TSH. Another cause is excess iodine availability, either from excess ingestion, induced by the drug amiodarone, or following iodinated contrast imaging.[46][47]
Hyperthyroidism often causes a variety of
Long-term management of hyperthyroidism may include drugs that suppress thyroid function such as
Hypothyroidism
An underactive thyroid gland results in hypothyroidism. Typical symptoms are abnormal weight gain, tiredness, constipation, heavy menstrual bleeding, hair loss, cold intolerance, and a slow heart rate.[48] Iodine deficiency is the most common cause of hypothyroidism worldwide,[53] and the autoimmune disease Hashimoto's thyroiditis is the most common cause in the developed world.[54] Other causes include congenital abnormalities, diseases causing transient inflammation, surgical removal or radioablation of the thyroid, the drugs amiodarone and lithium, amyloidosis, and sarcoidosis.[55] Some forms of hypothyroidism can result in myxedema and severe cases can result in myxedema coma.[56]
Hypothyroidism is managed with replacement of the thyroid hormones. This is usually given daily as an oral supplement, and may take a few weeks to become effective.[56] Some causes of hypothyroidism, such as Postpartum thyroiditis and Subacute thyroiditis may be transient and pass over time, and other causes such as iodine deficiency may be able to be rectified with dietary supplementation.[57]
Diseases
Graves' disease
Graves' disease is an autoimmune disorder that is the most common cause of hyperthyroidism.[58] In Graves' disease, for an unknown reason autoantibodies develop against the thyroid stimulating hormone receptor. These antibodies activate the receptor, leading to development of a goitre and symptoms of hyperthyroidism, such as heat intolerance, weight loss, diarrhoea and palpitations. Occasionally such antibodies block but do not activate the receptor, leading to symptoms associated with hypothyroidism.[58] In addition, gradual protrusion of the eyes may occur, called Graves' ophthalmopathy, as may swelling of the front of the shins.[58] Graves' disease can be diagnosed by the presence of pathomnomonic features such as involvement of the eyes and shins, or isolation of autoantibodies, or by results of a radiolabelled uptake scan. Graves' disease is treated with anti-thyroid drugs such as propylthiouracil, which decrease the production of thyroid hormones, but hold a high rate of relapse. If there is no involvement of the eyes, then use of radioactive isotopes to ablate the gland may be considered. Surgical removal of the gland with subsequent thyroid hormone replacement may be considered, however this will not control symptoms associated with the eye or skin.[58]
Nodules
Thyroid nodules are often found on the gland, with a prevalence of 4–7%.[59] The majority of nodules do not cause any symptoms, thyroid hormone secretion is normal, and they are non-cancerous.[60] Non-cancerous cases include simple cysts, colloid nodules, and thyroid adenomas. Malignant nodules, which only occur in about 5% of nodules, include follicular, papillary, medullary carcinomas and metastasis from other sites [61] Nodules are more likely in females, those who are exposed to radiation, and in those who are iodine deficient.[59]
When a nodule is present,
The presence of multiple nodules is called a
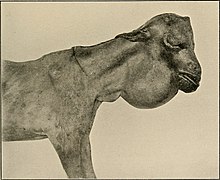
Goitre
An enlarged thyroid gland is called a goitre.[62] Goitres are present in some form in about 5% of people,[61] and are the result of a large number of causes, including iodine deficiency, autoimmune disease (both Graves' disease and Hashimoto's thyroiditis), infection, inflammation, and infiltrative disease such as sarcoidosis and amyloidosis. Sometimes no cause can be found, a state called "simple goitre".[63]
Some forms of goitre are associated with pain, whereas many do not cause any symptoms. Enlarged goitres may extend beyond the normal position of the thyroid gland to below the sternum, around the airway or esophagus.[61] Goitres may be associated with hyperthyroidism or hypothyroidism, relating to the underlying cause of the goitre.[61] Thyroid function tests may be done to investigate the cause and effects of the goitre. The underlying cause of the goitre may be treated, however many goitres with no associated symptoms are simply monitored.[61]
Inflammation
Inflammation of the thyroid is called
Postpartum thyroiditis occurs sometimes following childbirth. After delivery, the thyroid becomes inflamed and the condition initially presents with a period of hyperthyroidism followed by hypothyroidism and, usually, a return to normal function. [66] The course of the illness takes place over several months, and is characterised by a painless goitre. Antibodies against thyroid peroxidase can be found on testing. The inflammation usually resolves without treatment, although thyroid hormone replacement may be needed during the period of hypothyroidism.[66]
Cancer
The most common
In most cases, thyroid cancer presents as a painless mass in the neck. It is very unusual for thyroid cancers to present with other symptoms, although in some cases cancer may cause hyperthyroidism.[68] Most thyroid cancers are papillary, followed by follicular, medullary, and thyroid lymphoma.[67][68] Because of the prominence of the thyroid gland, cancer is often detected earlier in the course of disease as the cause of a nodule, which may undergo fine-needle aspiration. Thyroid function tests will help reveal whether the nodule produces excess thyroid hormones. A radioactive iodine uptake test can help reveal the activity and location of the cancer and metastases.[67][69]
Thyroid cancers are treated by
Congenital
A persistent thyroglossal duct is the most common clinically significant birth defect of the thyroid gland. A persistent sinus tract may remain as a vestigial remnant of the tubular development of the thyroid gland. Parts of this tube may be obliterated, leaving small segments to form thyroglossal cysts.[23] Preterm neonates are at risk of hypothyroidism as their thyroid glands are insufficiently developed to meet their postnatal needs.[71] In order to detect hypothyroidism in newborn babies, to prevent growth and development abnormalities in later life, many countries have newborn screening programs at birth.[72]
Infants with thyroid hormone deficiency (
Mucinous, clear secretions may collect within these cysts to form either spherical masses or fusiform swellings, rarely larger than 2 to 3 cm in diameter. These are present in the midline of the neck anterior to the trachea. Segments of the duct and cysts that occur high in the neck are lined by stratified squamous epithelium, which is essentially identical to that covering the posterior portion of the tongue in the region of the foramen cecum. The disorders that occur in the lower neck more proximal to the thyroid gland are lined by epithelium resembling the thyroidal acinar epithelium. Characteristically, next to the lining epithelium, there is an intense lymphocytic infiltrate. Superimposed infection may convert these lesions into abscess cavities, and rarely, give rise to cancers.[citation needed]
Another disorder is that of thyroid dysgenesis which can result in various presentations of one or more misplaced accessory thyroid glands.[4] These can be asymptomatic.
Iodine

Because the thyroid concentrates iodine, it also concentrates the various radioactive
Excessive iodine intake is uncommon and usually has no effect on the thyroid function. Sometimes though it may cause hyperthyroidism, and sometimes hypothyroidism with a resulting goitre.[80]
Evaluation
The thyroid is
An examination of the thyroid will also include observation of the person as a whole, to look for systemic signs such as weight gain or loss, hair loss, and signs in other locations – such as protrusion of the eyes or swelling of the calves in Graves' disease.[83][81]
Tests
TSH levels are considered the most sensitive marker of thyroid dysfunction.
T3 and T4 can be measured directly. However, as the two thyroid hormones travel bound to other molecules, and it is the "free" component that is biologically active, free T3 and free T4 levels can be measured.[84] T3 is preferred, because in hypothyroidism T3 levels may be normal.[84] The ratio of bound to unbound thyroid hormones is known as the thyroid hormone binding ratio (THBR).[85] It is also possible to measure directly the main carriers of the thyroid hormones, thyroglobulin and throxine-binding globulin.[86] Thyroglobulin will also be measurable in a healthy thyroid, and will increase with inflammation, and may also be used to measure the success of thyroid removal or ablation. If successful, thyroglobulin should be undetectable.[85] Lastly, antibodies against components of the thyroid, particularly anti-TPO and anti-thyroglobulin, can be measured. These may be present in normal individuals but are highly sensitive for autoimmune-related disease.[85]
Imaging
Ultrasound of the thyroid may be used to reveal whether structures are solid or filled with fluid, helping to differentiate between nodules and goitres and cysts. It may also help differentiate between malignant and benign lesions.[87]
When further imaging is required, a radiolabelled
A
Computed tomography of the thyroid plays an important role in the evaluation of thyroid cancer.[90] CT scans often incidentally find thyroid abnormalities, and thereby practically becomes the first investigation modality.[90]
History

The thyroid gland received its modern name in the 1600s, when the anatomist Thomas Wharton likened its shape to that of an Ancient Greek shield or thyos. However, the existence of the gland, and of the diseases associated with it, was known long before then.
Antiquity
The presence and diseases of the thyroid have been noted and treated for thousands of years.
Scientific era
In 1500 polymath Leonardo da Vinci provided the first illustration of the thyroid.[91] In 1543 anatomist Andreas Vesalius gave the first anatomic description and illustration of the gland.[91] In 1656 the thyroid received its modern name, by the anatomist Thomas Wharton.[91] The gland was named thyroid, meaning shield, as its shape resembled the shields commonly used in Ancient Greece.[91] The English name thyroid gland[93] is derived from the medical Latin used by Wharton – glandula thyreoidea.[94] Glandula means 'gland' in Latin,[95] and thyreoidea can be traced back to the Ancient Greek word θυρεοειδής, meaning 'shield-like/shield-shaped'.[96]
French chemist Bernard Courtois discovered iodine in 1811,[92] and in 1896 Eugen Baumann documented it as the central ingredient in the thyroid gland. He did this by boiling the thyroid glands of a thousand sheep, and named the precipitate, a combination of the thyroid hormones, 'iodothyrin'.[92] David Marine in 1907 proved that iodine is necessary for thyroid function.[92][91]
Graves' disease was described by Robert James Graves in 1834. The role of the thyroid gland in metabolism was demonstrated in 1895 by Adolf Magnus-Levy.[97] Thyroxine was first isolated in 1914 and synthesized in 1927, and triiodothyroxine in 1952.[92][98] The conversion of T4 to T3 was discovered in 1970.[91] The process of discovering TSH took place over the early to mid twentieth century.[99] TRH was discovered by Polish endocrinologist Andrew Schally in 1970, contributing in part to his Nobel Prize in Medicine in 1977.[91][100]
In the nineteenth century numerous authors described both
Surgery
Either
Other animals
The thyroid gland is found in all vertebrates. In fish, it is usually located below the gills and is not always divided into distinct lobes. However, in some teleosts, patches of thyroid tissue are found elsewhere in the body, associated with the kidneys, spleen, heart, or eyes.[104]
In tetrapods, the thyroid is always found somewhere in the neck region. In most tetrapod species, there are two paired thyroid glands – that is, the right and left lobes are not joined. However, there is only ever a single thyroid gland in most mammals, and the shape found in humans is common to many other species.[104]
In larval
Thyroxine is critical to
See also
- Desiccated thyroid
- Thyroid disease in pregnancy
References
- ^ Guyton & Hall 2011, p. 907.
- ^ ISBN 978-1-4377-1753-2.
- ^ Harrison's 2011, pp. 2913, 2918.
- ^ a b c d e f g h i j k l m n o p q r s t u Gray's Anatomy 2008, pp. 462–4.
- ^ a b c d e f g h i j k Elsevier's 2007, p. 342.
- ^ Elsevier's 2007, pp. 342–3.
- ISBN 978-0-443-07168-3.
- ISBN 978-1-4557-0418-7.
- ^ S2CID 22063700.
- ^ a b c Elsevier's 2007, p. 343.
- ^ PMID 17457471.
- PMID 23031220.
- ISBN 978-1-4160-6257-8.
- ISBN 978-0-340-80677-7.
- ^ ISBN 978-0-443-06850-8.
- ^ The Thyroid Follicle Archived 2013-01-23 at archive.today, Endocrinology by J. Larry Jameson, MD, PhD and Leslie J. De Groot, MD, chapter 72
- PMID 18012.
- ^ ISBN 978-0-443-06583-5.
- ^ a b c d Greenspan's 2011, p. 179.
- ^ ISBN 978-0-7817-4059-3.
- PMID 12671044.
- ^ a b c d "Iodine supplementation in pregnant and lactating women". World Health Organization. Archived from the original on January 4, 2014. Retrieved 2016-11-13.
- ^ ISBN 978-1-4511-9164-6.
- ^ a b Davidson's 2010, p. 736.
- ^ Guyton & Hall 2011, p. 909.
- ^ Guyton & Hall 2011, p. 934.
- ^ a b c d e Guyton & Hall 2011, p. 937.
- ^ a b c d e Guyton & Hall 2011, p. 936.
- ^ Guyton & Hall 2011, p. 935-6.
- ^ Greenspan's 2011, p. 169.
- ^ a b Bowen R (2000). "Thyroid Hormone Receptors". Colorado State University. Archived from the original on 27 September 2011. Retrieved 22 February 2015.
- ^ Greenspan's 2011, p. 178.
- ^ ISBN 978-1-4160-2328-9.
- ^ PMID 11844744.
- ISBN 978-1-4377-0324-5.
- ^ How Your Thyroid Works: A Delicate Feedback Mechanism. Updated 2009-05-21.
- ISBN 1-85996-252-1
- ^ Ganong's review of medical physiology Edition 25.
- ^ Greenspan's 2011, p. 174.
- ^ Greenspan's 2011, p. 177.
- ^ Guyton & Hall 2011, p. 896.
- ^ Harrison's 2011, pp. 2215.
- ^ Guyton & Hall 2011, pp. 988–9.
- ^ "The human proteome in thyroid gland – The Human Protein Atlas". www.proteinatlas.org. Retrieved 2017-09-25.
- S2CID 802377.
- ^ Davidson's 2010, p. 738.
- PMID 32232955.
- ^ a b Davidson's 2010, p. 740.
- ^ a b Davidson's 2010, p. 739.
- ^ Davidson's 2010, p. 745.
- PMID 23781316.
- ^ Thyroid Problems eMedicine Health. Retrieved on 2010-02-07
- ^ "Iodine Deficiency & Nutrition". www.thyroidfoundation.org.au. Australian Thyroid Foundation. Archived from the original on 13 January 2017. Retrieved 11 January 2017.
- ^ So M, MacIsaac R, Grossmann M. "Hypothyroidism – Investigation and management". www.racgp.org.au. The Royal Australian College of General Practitioners. Retrieved 11 January 2017.
- ^ Davidson's 2010, p. 741.
- ^ a b Davidson's 2010, p. 743.
- ^ Davidson's 2010, p. 741-3.
- ^ PMID 27797318. Archived from the original(PDF) on 2020-08-01. Retrieved 2020-07-22.
- ^ PMID 19041821.
- ^ PMID 12588078. Retrieved 6 September 2016.
- ^ a b c d e f g Davidson's 2010, p. 744.
- ^ "goitre – definition of goitre in English". Oxford Dictionaries | English. Archived from the original on September 18, 2016. Retrieved 18 September 2016.
- ^ Davidson's 2010, p. 750.
- ^ Harrison's 2011, pp. 2237.
- ^ a b c d Harrison's 2011, pp. 2230.
- ^ a b Harrison's 2011, pp. 2238.
- ^ a b c d e Harrison's 2011, p. 2242.
- ^ a b Davidson's 2010, p. 751.
- ^ a b Davidson's 2010, p. 752.
- ^ Harrison's 2011, p. 2242,2246.
- PMID 19812240.
- PMID 23154158.
- ^ a b c Greenspan's 2011, p. 164.
- PMID 16740880.
- ^ The thyroid gland in health and disease Year: 1917 Robert McCarrison
- ISBN 978-1-284-03445-5.
- PMID 23201844.
- ^ "Map: Count of Nutrients In Fortification Standards". Global Fortification Data Exchange. Retrieved 23 December 2019.
- ^ "Chernobyl children show DNA changes". BBC News. 2001-05-08. Retrieved 2010-05-25.
- ^ "Iodine - Disorders of Nutrition". MSD Manual Consumer Version. Archived from the original on 18 December 2019. Retrieved 18 December 2019.
- ^ ISBN 978-0-7295-4198-5.
- ISBN 978-1-4377-2419-6.
- ^ Harrison's 2011, p. 2228.
- ^ a b c d e f Greenspan's 2011, p. 184.
- ^ a b c Harrison's 2011, p. 2229.
- ^ Greenspan's 2011, p. 186.
- ^ Greenspan's 2011, p. 189.
- ^ Greenspan's 2011, p. 188-9.
- ^ Greenspan's 2011, p. 190.
- ^
- ^ a b c d e f g h i j k l m n o "Thyroid History Timeline – American Thyroid Association". www.thyroid.org. Archived from the original on 3 August 2021. Retrieved 13 November 2016.
- ^ PMID 21966648.
- ^ Anderson DM (2000). Dorland's Illustrated Medical Dictionary (29th ed.). Philadelphia/London/Toronto/Montreal/Sydney/Tokyo: W.B. Saunders Company.
- ^ His W (1895). Die anatomische Nomenclatur. Nomina Anatomica. Der von der Anatomischen Gesellschaft auf ihrer IX. Versammlung in Basel angenommenen Namen [The anatomical nomenclature. Nominal Anatomica. Anatomical Society on its IX. Assembly adopted in Basel] (in German). Leipzig: Verlag Veit & Comp.
- ^ Lewis CT, Short C (1879). A Latin dictionary. founded on Andrews' edition of Freund's Latin dictionary. Oxford: Clarendon Press.
- ^ Liddell HG, Scott R (1940). A Greek-English Lexicon. revised and augmented throughout by Sir Henry Stuart Jones. with the assistance of. Roderick McKenzie. Oxford: Clarendon Press.
- PMID 8527221.
- ^ Hamdy, Roland. "The thyroid glands: a brief historical perspective". www.medscape.com. Retrieved 2016-11-13.
- PMID 25114872.
- ^ "The Nobel Prize in Physiology or Medicine 1977". www.nobelprize.org. Retrieved 14 January 2017.
- ^ Slidescenter.com. "Hormones.gr". www.hormones.gr. Retrieved 2016-11-13.
- ISBN 978-0-7817-5047-9.
- ^ "The Nobel Prize in Physiology or Medicine 1909". Nobel Foundation. Retrieved 2007-07-28.
- ^ ISBN 978-0-03-910284-5.
- ISSN 1872-3136.
- ISSN 0393-9375.
Books
- Greer MA, ed. (1990). The Thyroid Gland. Comprehensive Endocrinology Revised Series. N.Y.: Raven Press. ISBN 0-88167-668-3.
- Shoback D (2011). Gardner DG (ed.). Greenspan's basic & clinical endocrinology (9th ed.). New York: McGraw-Hill Medical. ISBN 978-0-07-162243-1.
- Hall JE, Guyton AC (2011). Guyton and Hall textbook of medical physiology (12th ed.). Philadelphia, Pa.: Saunders/Elsevier. ISBN 978-1-4160-4574-8.
- Longo D, Fauci A, Kasper D, Hauser S, Jameson J, Loscalzo J (August 11, 2011). Harrison's Principles of Internal Medicine (18 ed.). McGraw-Hill Professional. ISBN 978-0-07-174889-6.
- Colledge NR, Walker BR, Ralston SH, eds. (2010). Davidson's principles and practice of medicine. Illustrated by Robert Britton (21st ed.). Edinburgh: Churchill Livingstone/Elsevier. ISBN 978-0-7020-3085-7.
- Ort V, Bogart BI (2007). Elsevier's integrated anatomy and embryology. Philadelphia, Pa.: Elsevier Saunders. ISBN 978-1-4160-3165-9.
- Standring S, Borley NR, et al., eds. (2008). Gray's anatomy : the anatomical basis of clinical practice (40th ed.). London: Churchill Livingstone. ISBN 978-0-8089-2371-8.
