Thyroid nodule
| Thyroid nodule | |
|---|---|
ENT surgery, oncology |
Thyroid nodules are
Signs and symptoms
Often these abnormal growths of thyroid tissue are located at the edge of the thyroid gland and can be felt as a lump in the throat. When they are large, they can sometimes be seen as a lump in the front of the neck.[citation needed]
Sometimes a thyroid nodule presents as a fluid-filled cavity called a thyroid cyst. Often, solid components are mixed with the fluid. Thyroid cysts most commonly result from degenerating thyroid adenomas, which are benign, but they occasionally contain malignant solid components.[3]
Diagnosis
After a
Thyroid nodules are extremely common in young adults and children. Almost 50% of people have had one, but they are usually only detected by a physician during the course of a health examination or fortuitously discovered during the investigation of an unrelated condition.[8]
Workup of incidental nodules
| Features | Workup |
|---|---|
|
Very likely ultrasonography |
| Multiple nodules | Likely ultrasonography |
| Solitary nodule in person younger than 35 years old |
|
| Solitary nodule in person at least 35 years old |
|
Ultrasound
Fine needle biopsy
| Category | Description | Risk of malignancy[18] | Recommendation[18] |
|---|---|---|---|
| I | Non diagnostic/unsatisfactory | – | Repeating FNAC with ultrasound-guidance in more than 3 months |
| II | Benign (colloid and follicular cells) | 0–3% | Clinical follow-up |
| III | Atypia of undetermined significance (AUS) or follicular lesion of undetermined significance (FLUS) (follicular or lymphoid cells with atypical features) | 5–15% | Repeating FNAC |
| IV | Follicular nodule/suspicious follicular nodule (cell crowding, micro follicles, dispersed isolated cells, scant colloid) | 15–30% | Surgical lobectomy |
| V | Suspicious for malignancy | 60–75% | Surgical lobectomy or near-total thyroidectomy |
| VI | Malignant | 97–99% | Near-total thyroidectomy |
Blood tests
Other imaging
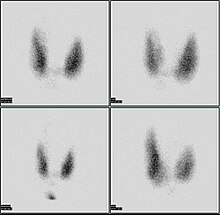
A thyroid scan using a radioactive iodine uptake test can be used in viewing the thyroid.[19] A scan using iodine-123 showing a hot nodule, accompanied by a lower than normal TSH, is strong evidence that the nodule is not cancerous, as most hot nodules are benign.[citation needed]
Computed tomography of the thyroid plays an important role in the evaluation of thyroid cancer.[20] CT scans often incidentally find thyroid abnormalities, and thereby practically becomes the first investigation modality.[20]
Malignancy
Only a small percentage of lumps in the neck are malignant (around 4 – 6.5%[21]), and most thyroid nodules are benign colloid nodules.
There are many factors to consider when diagnosing a malignant lump. Trouble swallowing or speaking, swollen cervical lymph nodes or a firm, immobile nodule are more indicative of malignancy, whereas a family history of autoimmune disease or goiter, thyroid hormonal dysfunction or a soft, painful nodule are more indicative of benignancy.[citation needed]
The prevalence of cancer is higher in males, patients under 20 years old or over 70 years old, and patients with a history of head and neck irradiation or a family history of thyroid cancer.[22]
Solitary thyroid nodule

Risks for cancer
Solitary
Radiation exposure to the head and neck may be for historic indications such as tonsillar and adenoid hypertrophy, "enlarged thymus", acne vulgaris, or current indications such as Hodgkin's lymphoma. Children living near the Chernobyl nuclear power plant during the catastrophe of 1986 have experienced a 60-fold increase in the incidence of thyroid cancer. Thyroid cancer arising in the background of radiation is often multifocal with a high incidence of lymph node metastasis and has a poor prognosis.[citation needed]
Signs and symptoms
Worrisome sign and symptoms include voice hoarseness, rapid increase in size, compressive symptoms (such as dyspnoea or dysphagia) and appearance of lymphadenopathy.[citation needed]
Investigations
- TSH – A thyroid-stimulating hormone level should be obtained first. If it is suppressed, then the nodule is likely a hyperfunctioning (or "hot") nodule. These are rarely malignant.
- FNAC – fine
- Imaging – radioiodinescanning.
Thyroid scan
85% of nodules are cold nodules, and 5–8% of cold and warm nodules are malignant.[27]
5% of nodules are hot. Malignancy is virtually non-existent in hot nodules.[28]
Surgery
Surgery (thyroidectomy) may be indicated in the following instances:
- Reaccumulation of the nodule despite 3–4 repeated FNACs
- Size in excess of 4 cm in some cases
- Compressive symptoms
- Signs of malignancy (vocal cord dysfunction, lymphadenopathy)
- Cytopathology that does not exclude thyroid cancer
Minimally-invasive procedures
Non-surgical, minimally invasive ultrasound-guided techniques are now being used for the treatment of large, symptomatic nodules. They include percutaneous ethanol injection, laser thermal ablation, radiofrequency ablation, high intensity focused ultrasound (HIFU), and percutaneous microwave ablation.[29]
HIFU has recently proved its effectiveness in treating benign thyroid nodules. This method is noninvasive, without general anesthesia and is performed in an ambulatory setting. Ultrasound waves are focused and produce heat enabling to destroy thyroid nodules.[30] Focused ultrasounds have been used to treat other benign tumors, such as breast fibroadenomas and fibroid disease in the uterus.[citation needed]
Treatment
Levothyroxine (T4) is a prohormone that peripheral tissues convert to the primary active thyroid hormone, triiodothyronine (T3). Hypothyroid patients normally take it once per day.
Autonomous thyroid nodule
An autonomous thyroid nodule or "hot nodule" is one that has thyroid function independent of the
See also
References
- ^ "New York Thyroid Center: Thyroid Nodules". Archived from the original on 2010-09-17.
- PMID 21893493.
- ^ "Symptoms and causes - Mayo Clinic". Mayo Clinic.
- S2CID 21514672.
- PMID 11156519.
- ^ "Thyroid Nodule". www.meddean.luc.edu.
- PMID 32491169.
- PMID 25538897.
- ^ Jenny Hoang (2013-11-05). "Reporting of incidental thyroid nodules on CT and MRI". Radiopaedia., citing:
- Hoang JK, Langer JE, Middleton WD, Wu CC, Hammers LW, Cronan JJ, et al. (February 2015). "Managing incidental thyroid nodules detected on imaging: white paper of the ACR Incidental Thyroid Findings Committee". Journal of the American College of Radiology. 12 (2): 143–150. PMID 25456025.
- Hoang JK, Langer JE, Middleton WD, Wu CC, Hammers LW, Cronan JJ, et al. (February 2015). "Managing incidental thyroid nodules detected on imaging: white paper of the ACR Incidental Thyroid Findings Committee". Journal of the American College of Radiology. 12 (2): 143–150.
- S2CID 5042725.
- ^ PMID 16361145.
- .
- PMID 19276237.
- PMID 30299457.
- S2CID 15979225.
- ^ Diana SD, Hossein G. "Fine-Needle Aspiration Biopsy of the Thyroid Gland". Thyroid Disease Manager. Archived from the original on 12 July 2017. Retrieved 16 October 2017.
- PMID 27294815.
- ^ PMID 24294568.
- ^ MedlinePlus Encyclopedia: Thyroid scan
- ^
- ^ "UpToDate".
- ^ Thyroid Nodule at eMedicine
- PMID 26458591.
- ^ Schwartz 7th/e page 1679,1678
- S2CID 32693137.
- S2CID 205287747.
- PMID 19482296.
- ^ Robbins pathology 8ed page 767
- PMID 32038482.
- ^ "Echotherapy for thyroid nodules". Echotherapy.
- PMID 8190053.
