Ticagrelor
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Brilinta, Brilique, others |
| Other names | AZD-6140 |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a611050 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | By mouth |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 36% |
| Protein binding | >99.7% |
| Metabolism | Liver (CYP3A4) |
| Elimination half-life | 7 hrs (ticagrelor), 8.5 hrs (active metabolite AR-C124910XX) |
| Excretion | Bile duct |
| Identifiers | |
| |
JSmol) | |
| |
| |
| | |
Ticagrelor, sold under the brand name Brilinta among others, is a

The most common side effects include
It was approved for medical use in the European Union in December 2010,[6][8][9] and in the United States in July 2011.[5][10][11] In 2020, it was the 247th most commonly prescribed medication in the United States, with more than 1 million prescriptions.[12][13]
Medical uses
In the US, ticagrelor is
In the EU, ticagrelor, co-administered with acetylsalicylic acid (aspirin), is indicated for the prevention of atherothrombotic events in adults with acute coronary syndromes or a history of myocardial infarction and a high risk of developing an atherothrombotic event; and for the prevention of atherothrombotic events in adults with a history of myocardial infarction and a high risk of developing an atherothrombotic event.[6]
Contraindications
Contraindications to ticagrelor are active bleeding, increased risk of bradycardia, concomitant therapy of ticagrelor and strong cytochrome P-450 3A (CYP3A4) inhibitors and moderate or severe hepatic impairment due to the risk of increased exposure to ticagrelor.[14][15]
Adverse effects
The common adverse effects are increased risk of bleeding (which may be severe)[16] and shortness of breath (dyspnoea).[17] Dyspnoea is usually transient and mild-to-moderate in severity, with a higher risk at < 1 month, 1–6 months and >6 months of follow up compared to clopidogrel.[17][18][19][20] Discontinuation of therapy is rare, although some people do not persist or switch therapies.[17][18][19] People who develop tolerable dyspnoea as a side effect of ticagrelor should be reassured to continue therapy, as it does not impact on the drug's cardiovascular benefit and bleeding risk in acute coronary syndrome (ACS).[17] Furthermore, two small subgroup analyses found no associations between ticagrelor and adverse changes in heart and lung function that may induce dyspnoea in stable coronary artery disease (CAD) and people with ACS without heart failure or significant lung disease.[18][21]
Ventricular pauses ≥3 seconds may occur in people with ACS the first week of treatment, but are likely to be mostly asymptomatic and transient, without causing increased clinical bradycardic adverse events.
Interactions
Inhibitors of the liver enzyme CYP3A4, such as
The drug also inhibits P-glycoprotein (P-gp), leading to increased plasma levels of digoxin, ciclosporin and other P-gp substrates. Levels of ticagrelor and AR-C124910XX (the active metabolite of ticagrelor formed by O-deethylation[27]) are not significantly influenced by P-gp inhibitors.[24]
It is recommended to use low-dose aspirin (75–100 mg per day) with ticagrelor as dual antiplatelet therapy (DAPT).[14][28][29][30][31][32] The combination of ticagrelor with aspirin doses greater than 100 mg per day may be less effective.[33]
Pharmacology
Mechanism of action
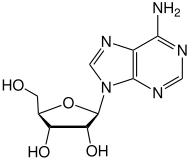
Like the
Pharmacokinetics
Ticagrelor is absorbed quickly from the gut, the bioavailability being 36%, and reaches its peak concentration after about 1.5 hours. The main metabolite, AR-C124910XX, is formed quickly via CYP3A4 by de-hydroxyethylation at position 5 of the cyclopentane ring.[27]
Plasma concentrations of ticagrelor are slightly increased (12–23%) in elderly people, women, people of
Consistently with its reversible mode of action, ticagrelor is known to act faster and shorter than clopidogrel.
Chemistry
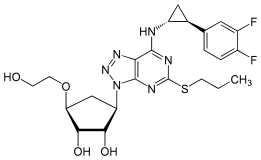
Ticagrelor is a
 |
 |
Research
With clopidogrel
The PLATO trial concluded superiority of ticagrelor compared to clopidogrel in reducing the rate of death from vascular causes, MI, and stroke in people presenting with acute coronary syndromes.[14] A post-hoc subgroup analysis of the PLATO trial suggested a reduction in total mortality with ticagrelor compared to clopidogrel in people with non-ST elevation acute coronary syndrome.[42] However, this finding should only be considered exploratory as it was not a primary endpoint of the PLATO trial.[14] Subsequent studies have also been underpowered in evaluating total mortality benefits with ticagrelor.[43]
The PLATO trial[44] found that ticagrelor use, in conjunction with low-dose aspirin (where tolerated), had better all-cause mortality rates than the same treatment plan with clopidogrel (4.5% vs. 5.9%, p<0.001) in treating people with acute coronary syndrome. People given ticagrelor were less likely to die from vascular causes, heart attack, or stroke, regardless of whether the treatment plan was invasive. While the patient group on ticagrelor had more instances of fatal bleeding and intracranial bleeding, the difference in cases was not considered significant (p=0.70). Rates of major bleeding were not significantly different between the two groups (7.9% vs. 7.7%, p=0.57). However, dyspnoea was significantly more likely in the ticagrelor group (13.8% vs. 7.8%, p<0.001). Premature discontinuation of the study drug was far more common in the ticagrelor group (23.4% vs. 21.5%, p=0.002), which could be due to adverse events (7.4% vs. 6.0%, p<0.001) or the patient’s unwillingness to continue (10.1% vs. 9.2%, p = 0.04).[14]
The PLATO trial showed a statistically insignificant trend toward worse outcomes with ticagrelor versus clopidogrel among US participants in the study – who comprised 1627 of the total 13,326 participants. The hazard ratio actually reversed for the composite end point cardiovascular (death, MI, or stroke): 11.1% for participants given ticagrelor and 9.1% for participants given clopidogrel (HR = 1.27).[44] It is important to note that even though there was a trend to worse outcomes in the US patient population, this trend was still classed as insignificant, and therefore should not affect patient use in the US population.[44]
There is some conjecture in the safety and efficacy of ticagrelor within the Asian population, despite significant thrombotic benefits.[42] A meta-analysis of observational studies in several Asian countries proposed that ticagrelor did not increase the risk of considerable bleeding events in Asian individuals.[45] It is important to note that despite this being “real world” data, the study did not provide ethnic population demographics, leading to potential generalisation of data for Asian individuals.[45] There is evidence to suggest that East Asian individuals are at a higher risk of bleeding events when using ticagrelor.[46][47][48] Several recent meta-analyses of RCTs have been carried out in this population and although underpowered (more research is needed), the Asian Pacific Society of Cardiology Guidelines have taken these trials into account.[46][47][48][49] The guidelines recommend that people of East Asian origin exercise caution and that treatment continuation after six months be based on net-clinical benefit.[49]
With prasugrel
In 2019, the results of the ISAR-REACT 5 trial was published, comparing ticagrelor and prasugrel in participants with acute coronary syndrome.[50]
An
References
- ^ "Updates to the Prescribing Medicines in Pregnancy database". Therapeutic Goods Administration (TGA). 12 May 2022. Retrieved 13 May 2022.
- FDA. Retrieved 22 October 2023.
- ^ "Ticalor; Blooms The Chemist Ticagrelor; Apo-Ticagrelor; Ticagrelor Arx (Accelagen Pty Ltd)". Therapeutic Goods Administration (TGA). 11 November 2022. Retrieved 9 April 2023.
- ^ "Product monograph brand safety updates". Health Canada. February 2024. Retrieved 24 March 2024.
- ^ a b c "Brilinta- ticagrelor tablet". DailyMed. 10 August 2021. Retrieved 19 May 2022.
- ^ a b c d "Brilique EPAR". European Medicines Agency. 17 September 2018. Retrieved 18 May 2022. Text was copied from this source which is copyright European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- PMID 20594935.
- ^ a b "Assessment Report for Brilique" (PDF). European Medicines Agency. January 2011.
- ^ European Public Assessment Report Possia
- ^ "FDA approves blood-thinning drug Brilinta to treat acute coronary syndromes" (Press release). U.S. Food and Drug Administration (FDA). 20 July 2011. Archived from the original on 12 January 2017.
- ^ "Drug Approval Package: Brilinta (ticagrelor) NDA #022433". U.S. Food and Drug Administration (FDA). 22 August 2011. Retrieved 22 May 2021.
- ^ "The Top 300 of 2020". ClinCalc. Retrieved 7 October 2022.
- ^ "Ticagrelor - Drug Usage Statistics". ClinCalc. Retrieved 7 October 2022.
- ^ PMID 19717846.
- PMID 23650452.
- PMID 22090660.
- ^ PMID 21804104.
- ^ PMID 20620737.
- ^ S2CID 35647876.
- PMID 32183711.
- PMID 21890085.
- PMID 21545948.
- ^ 6 [dead link]
- ^ a b c d Haberfeld, H, ed. (2010). Austria-Codex (in German) (2010/2011 ed.). Vienna: Österreichischer Apothekerverlag.
- ^ PMID 30003466.
- S2CID 17914035.
- ^ S2CID 22084793.
- PMID 27476580.
- PMID 26320110.
- PMID 25260718.
- ^ "Brilinta (ticagrelor) Prescribing Information" (PDF). AstraZeneca. 2019.
- ^ "Australia Product Information Brilinta (ticagrelor)". AstraZeneca. 2019.
- PMID 21709065.
- PMID 22282698.
- ^ Spreitzer H (4 February 2008). "Neue Wirkstoffe - AZD6140". Österreichische Apothekerzeitung (in German) (3/2008): 135.
- .
- PMID 21079055.
- S2CID 240072625.
- ^ "Brilique: EPAR – Product Information" (PDF). European Medicines Agency. 16 October 2019.
- ^ Miller R (24 February 2010). "Is there too much excitement for ticagrelor?". TheHeart.org.
- ^ Spreitzer H (17 January 2011). "Neue Wirkstoffe - Elinogrel". Österreichische Apothekerzeitung (in German) (2/2011): 10.
- ^ PMID 24727884.
- PMID 33035298.
- ^ S2CID 22469812.
- ^ PMID 31000178.
- ^ S2CID 3377054.
- ^ S2CID 246388246.
- ^ PMID 29094604.
- ^ PMID 33708263.
- S2CID 201712809.
- ^ PMID 31066863.
- S2CID 220631373.
- PMID 32750138.
