Toxoplasmosis
This article may be too technical for most readers to understand. (May 2023) |
This article needs attention from an expert in medicine. The specific problem is: convoluted logic in first para of diagnosis. (May 2023) |
| Toxoplasmosis | |
|---|---|
Infectious disease | |
| Symptoms | Often none, during pregnancy (birth defects)[1][2] |
| Causes | Toxoplasma gondii[3] |
| Risk factors | Eating poorly cooked food, exposure to infected cat feces[3] |
| Diagnostic method | Blood test, amniotic fluid test[4] |
| Treatment | During pregnancy spiramycin or pyrimethamine/sulfadiazine and folinic acid[5] |
| Frequency | Up to 50% of people, 200,000 cases of congenital toxoplasmosis a year[6][7] |
Toxoplasmosis is a
Toxoplasmosis is usually spread by eating poorly cooked food that contains
Prevention is by properly preparing and cooking food.[10] Pregnant women are also recommended not to clean cat litter boxes or, if they must, to wear gloves and wash their hands afterwards.[10] Treatment of otherwise healthy people is usually not needed.[5] During pregnancy, spiramycin or pyrimethamine/sulfadiazine and folinic acid may be used for treatment.[5]
Up to half of the world's population is infected by T. gondii, but have no symptoms.[7] In the United States, approximately 11% of people have been infected, while in some areas of the world this is more than 60%.[3] Approximately 200,000 cases of congenital toxoplasmosis occur a year.[6] Charles Nicolle and Louis Manceaux first described the organism in 1908.[11] In 1941, transmission during pregnancy from a pregnant woman to her baby was confirmed.[11] There is tentative evidence that infection may affect people's behavior.[12]
Signs and symptoms
Infection has three stages:
Acute
Acute toxoplasmosis is often asymptomatic in healthy adults.
Latent
Due to the absence of obvious symptoms,
Reviews of serological studies have estimated that 30–50% of the global population has been exposed to and may be chronically infected with latent toxoplasmosis, although infection rates differ significantly from country to country.[7][25][26] This latent state of infection has recently been associated with numerous disease burdens,[7] neural alterations,[23][25] and subtle gender-dependent behavioral changes in immunocompetent humans,[27][28] as well as an increased risk of motor vehicle collisions.[29]
Skin
While rare, skin lesions may occur in the acquired form of the disease, including
Cause
Parasitology
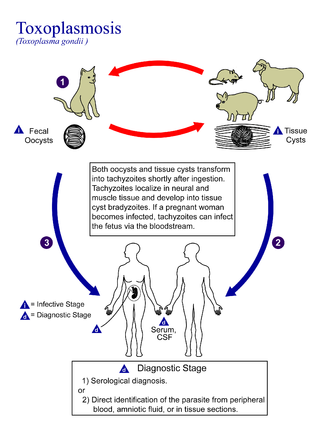
In its lifecycle, T. gondii adopts several forms.
The parasite's survival is dependent on a balance between host survival and parasite proliferation.[34] T. gondii achieves this balance by manipulating the host's immune response, reducing the host's immune response, and enhancing the parasite's reproductive advantage.[34] Once it infects a normal host cell, it resists damage caused by the host's immune system, and changes the host's immune processes.[35] As it forces its way into the host cell, the parasite forms a
When first invading the cell, the parasite releases ROP proteins from the bulb of the rhoptry organelle.[2] These proteins translocate to the nucleus and the surface of the PV membrane where they can activate STAT pathways to modulate the expression of cytokines at the transcriptional level, bind and inactivate PV membrane destroying IRG proteins, among other possible effects.[2][36][37] Additionally, certain strains of T. gondii can secrete a protein known as GRA15, activating the NF-κB pathway, which upregulates the pro-inflammatory cytokine IL-12 in the early immune response, possibly leading to the parasite's latent phase.[2] The parasite's ability to secrete these proteins depends on its genotype and affects its virulence.[2][37]
The parasite also influences an anti-apoptotic mechanism, allowing the infected host cells to persist and replicate. One method of
T. gondii also has the ability to initiate autophagy of the host's cells.[39] This leads to a decrease in healthy, uninfected cells, and consequently fewer host cells to attack the infected cells. Research by Wang et al finds that infected cells lead to higher levels of autophagosomes in normal and infected cells.[39] Their research reveals that T. gondii causes host cell autophagy using a calcium-dependent pathway.[39] Another study suggests that the parasite can directly affect calcium being released from calcium stores, which are important for the signalling processes of cells.[38]
The mechanisms above allow T. gondii to persist in a host. Some limiting factors for the toxoplasma is that its influence on the host cells is stronger in a weak immune system and is quantity-dependent, so a large number of T. gondii per host cell cause a more severe effect.[40] The effect on the host also depends on the strength of the host immune system. Immunocompetent individuals do not normally show severe symptoms or any at all, while fatality or severe complications can result in immunocompromised individuals.[40]
T. gondii has been shown to produce a protein called GRA28, released by the MYR1 secretory pathway, which interferes with gene expression in infected cells and results in cells that behave like dendritic cells, becoming highly mobile in the body.[41]
Since the parasite can change the host's immune response, it may also have an effect, positive or negative, on the immune response to other pathogenic threats.[34] This includes, but is not limited to, the responses to infections by Helicobacter felis, Leishmania major, or other parasites, such as Nippostrongylus brasiliensis.[34]
Transmission
Toxoplasmosis is generally transmitted through the mouth when Toxoplasma gondii
Oral transmission may occur through:
- Ingestion of raw or partly cooked meat, especially pork, lamb, or venison containing Toxoplasma cysts: Infection prevalence in countries where undercooked meat is traditionally eaten has been related to this transmission method. Tissue cysts may also be ingested during hand-to-mouth contact after handling undercooked meat, or from using knives, utensils, or cutting boards contaminated by raw meat.[46]
- Ingestion of unwashed fruit or vegetables that have been in contact with contaminated soil containing infected cat feces.[47]
- Ingestion of cat feces containing oocysts: This can occur through hand-to-mouth contact following gardening, cleaning a cat's litter box, contact with children's sandpits; the parasite can survive in the environment for months.[48]
- Ingestion of untreated, unfiltered water through direct consumption or utilization of water for food preparation.[49]
- Ingestion of unpasteurized milk and milk products, particularly goat's milk.[50]
- Ingestion of raw seafood.[51]
Cats excrete the pathogen in their feces for a number of weeks after contracting the disease, generally by eating an infected intermediate host that could include mammals (like rodents) or birds. Oocyst shedding usually starts from the third day after ingestion of infected intermediate hosts, and may continue for weeks. The oocysts are not infective when excreted. After about a day, the oocyst undergoes a process called sporulation and becomes potentially pathogenic.[52] In addition to cats, birds and mammals including human beings are also intermediate hosts of the parasite and are involved in the transmission process. However the pathogenicity varies with the age and species involved in infection and the mode of transmission of T. gondii.[53]
Toxoplasmosis may also be transmitted through solid organ transplants. Toxoplasma-seronegative recipients who receive organs from recently infected Toxoplasma-seropositive donors are at risk. Organ recipients who have latent toxoplasmosis are at risk of the disease reactivating in their system due to the immunosuppression occurring during solid organ transplant.[44] Recipients of hematogenous stem cell transplants may experience higher risk of infection due to longer periods of immunosuppression.[45]
Heart and lung transplants provide the highest risk for toxoplasmosis infection due to the striated muscle making up the heart,[44] which can contain cysts, and risks for other organs and tissues vary widely.[54] Risk of transmission can be reduced by screening donors and recipients prior to the transplant procedure and providing treatment.[54]
Pregnancy precautions
Not much evidence exists around the effect of education before pregnancy to prevent congenital toxoplasmosis.[56] However educating parents before the baby is born has been suggested to be effective because it may improve food, personal and pet hygiene.[56] More research is needed to find whether antenatal education can reduce congenital toxoplasmosis.[56]
For pregnant women with negative antibody titers, indicating no previous exposure to T. gondii, serology testing as frequent as monthly is advisable as treatment during pregnancy for those women exposed to T. gondii for the first time dramatically decreases the risk of passing the parasite to the fetus. Since a baby's immune system does not develop fully for the first year of life, and the resilient cysts that form throughout the body are very difficult to eradicate with antiprotozoans, an infection can be very serious in the young.[citation needed]
Despite these risks, pregnant women are not routinely screened for toxoplasmosis in most countries, for reasons of cost-effectiveness and the high number of
Pregnant women should avoid handling
In 2006, a Czech research team[66] discovered women with high levels of toxoplasmosis antibodies were significantly more likely to give birth to baby boys than baby girls. In most populations, the birth rate is around 51% boys, but people infected with T. gondii had up to a 72% chance of a boy.[67]
Diagnosis
Diagnosis of toxoplasmosis in humans is made by biological, serological, histological, or molecular methods, or by some combination of the above.[62] Toxoplasmosis can be difficult to distinguish from primary central nervous system lymphoma. It mimics several other infectious diseases so clinical signs are non-specific and are not sufficiently characteristic for a definite diagnosis. As a result, the possibility of an alternative diagnosis is supported by a failed trial of antimicrobial therapy (pyrimethamine, sulfadiazine, and folinic acid (USAN: leucovorin)), i.e., if the drugs produce no effect clinically and no improvement on repeat imaging.[citation needed]
T. gondii may also be detected in blood, amniotic fluid, or cerebrospinal fluid by using polymerase chain reaction.[68] T. gondii may exist in a host as an inactive cyst that would likely evade detection.[citation needed]
The most commonly used tests to measure
To some extent, acute toxoplasmosis infections can be differentiated from chronic infections using an IgG avidity test, which is a variation on the ELISA. In the first response to infection, toxoplasma-specific IgG has a low affinity for the toxoplasma antigen; in the following weeks and month, IgG affinity for the antigen increases. Based on the IgG avidity test, if the IgG in the infected individual has a high affinity, it means that the infection began three to five months before testing. This is particularly useful in congenital infection, where pregnancy status and gestational age at time of infection determines treatment.[71]
In contrast to IgG, IgM antibodies can be used to detect acute infection but generally not chronic infection.
In 2021, twenty commercial anti-Toxoplasma IgG assays were evaluated in a
Congenital

Recommendations for the diagnosis of congenital toxoplasmosis include: prenatal diagnosis based on
Even though diagnosis of toxoplasmosis heavily relies on serological detection of specific anti-Toxoplasma immunoglobulin, serological testing has limitations. For example, it may fail to detect the active phase of T. gondii infection because the specific anti-Toxoplasma IgG or IgM may not be produced until after several weeks of infection. As a result, a pregnant woman might test negative during the active phase of T. gondii infection leading to undetected and therefore untreated congenital toxoplasmosis.[74] Also, the test may not detect T. gondii infections in immunocompromised patients because the titers of specific anti-Toxoplasma IgG or IgM may not rise in this type of patient.[citation needed]
Many PCR-based techniques have been developed to diagnose toxoplasmosis using clinical specimens that include amniotic fluid,
Real-time PCR is useful in pathogen detection, gene expression and regulation, and allelic discrimination. This PCR technique utilizes the 5' nuclease activity of Taq DNA polymerase to cleave a nonextendible, fluorescence-labeled hybridization probe during the extension phase of PCR.[74] A second fluorescent dye, e.g., 6-carboxy-tetramethyl-rhodamine, quenches the fluorescence of the intact probe.[74] The nuclease cleavage of the hybridization probe during the PCR releases the effect of quenching resulting in an increase of fluorescence proportional to the amount of PCR product, which can be monitored by a sequence detector.[74]
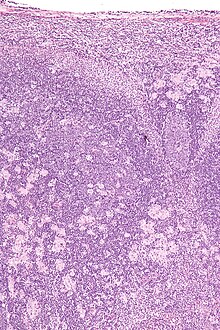
Lymph nodes affected by Toxoplasma have characteristic changes, including poorly demarcated reactive
The classic triad of congenital toxoplasmosis includes:
Congenital toxoplasmosis may also impact a child's hearing. Up to 30% of newborns have some degree of sensorineural hearing loss.[77] The child's communication skills may also be affected. A study published in 2010 looked at 106 patients, all of whom received toxoplasmosis treatment prior to 2.5 months. Of this group, 26.4% presented with language disorders.[78]
Treatment
Treatment is recommended for people with serious health problems, such as people with HIV whose CD4 counts are under 200 cells/mm3. Trimethoprim/sulfamethoxazole is the drug of choice to prevent toxoplasmosis, but not for treating active disease. A 2012 study shows a promising new way to treat the active and latent form of this disease using two endochin-like quinolones.[79]
Acute
The medications prescribed for acute toxoplasmosis are the following:[citation needed]
- Pyrimethamine – an antimalarial medication
- Sulfadiazine – an antibiotic used in combination with pyrimethamine to treat toxoplasmosis
- Combination therapy is usually given with folic acid supplements to reduce incidence of thrombocytopaenia.
- Combination therapy is most useful in the setting of HIV.
- Combination therapy is usually given with folic acid supplements to reduce incidence of
- Clindamycin[80]
- Spiramycin – an antibiotic used most often for pregnant women to prevent the infection of their children.
(other antibiotics, such as minocycline, have seen some use as a salvage therapy).
If infected during pregnancy, spiramycin is recommended in the first and early second trimesters while pyrimethamine/sulfadiazine and
Latent
In people with latent toxoplasmosis, the cysts are immune to these treatments, as the antibiotics do not reach the
The medications prescribed for latent toxoplasmosis are:
- AIDS patients[82]
- Clindamycin – an antibiotic that, in combination with atovaquone, seemed to optimally kill cysts in mice[83]
Congenital
When a pregnant woman is diagnosed with acute toxoplasmosis, amniocentesis can be used to determine whether the fetus has been infected or not. When a pregnant woman develops acute toxoplasmosis, the
If the parasite has not yet reached the fetus,
Newborns who undergo 12 months of postnatal anti-toxoplasmosis treatment have a low chance of sensorineural hearing loss.[86] Information regarding treatment milestones for children with congenital toxoplasmosis have been created for this group.[87]
Epidemiology
T. gondii infections occur throughout the world, although infection rates differ significantly by country.[26] For women of childbearing age, a survey of 99 studies within 44 countries found the areas of highest prevalence are within Latin America (about 50–80%), parts of Eastern and Central Europe (about 20–60%), the Middle East (about 30–50%), parts of Southeast Asia (about 20–60%), and parts of Africa (about 20–55%).[26]
In the United States, data from the
The protist responsible for toxoplasmosis is T. gondii. There are three major types of T. gondii responsible for the patterns of toxoplasmosis throughout the world. There are types I, II, and III. These three types of T. gondii have differing effects on certain hosts, mainly mice and humans due to their variation in genotypes.[90]
- Type I: virulent in mice and humans, seen in people with AIDS.
- Type II: non-virulent in mice, virulent in humans (mostly Europe and North America), seen in people with AIDS.
- Type III: non-virulent in mice, virulent mainly in animals but seen to a lesser degree in humans as well.
Current
Because the parasite poses a particular threat to fetuses when it is contracted during pregnancy,
History
The first recorded case of congenital toxoplasmosis was in 1923, but it was not identified as caused by T. gondii.[42] Janků (1923) described in detail the autopsy results of an 11-month-old boy who had presented to hospital with hydrocephalus. The boy had classic marks of toxoplasmosis including chorioretinitis (inflammation of the choroid and retina of the eye).[42] Histology revealed a number of "sporocytes", though Janků did not identify these as T. gondii.[42]
It was not until 1937 that the first detailed scientific analysis of T. gondii took place using techniques previously developed for analyzing viruses.[11] In 1937 Sabin and Olitsky analyzed T. gondii in laboratory monkeys and mice. Sabin and Olitsky showed that T. gondii was an obligate intracellular parasite and that mice fed T. gondii-contaminated tissue also contracted the infection.[11] Thus Sabin and Olitsky demonstrated T. gondii as a pathogen transmissible between animals.[citation needed]
T. gondii was first described as a human pathogen in 1939 at
The first adult case of toxoplasmosis was reported in 1940 with no neurological signs. Pinkerton and Weinman reported the presence of Toxoplasma in a 22-year-old man from Peru who died from a subsequent bacterial infection and fever.[42]
In 1948, a serological dye test was created by Sabin and Feldman based on the ability of the patient's antibodies to alter staining of Toxoplasma.[11][95] The Sabin Feldman Dye Test is now the gold standard for identifying Toxoplasma infection.[11]
Transmission of Toxoplasma by eating raw or undercooked meat was demonstrated by Desmonts et al. in 1965 Paris.[11] Desmonts observed that the therapeutic consumption of raw beef or horse meat in a tuberculosis hospital was associated with a 50% per year increase in Toxoplasma antibodies.[11] This means that more T. gondii was being transmitted through the raw meat.
In 1974, Desmonts and Couvreur showed that infection during the first two trimesters produces most harm to the fetus, that transmission depended on when mothers were infected during pregnancy, that mothers with antibodies before pregnancy did not transmit the infection to the fetus, and that spiramycin lowered the transmission to the fetus.[42]
Toxoplasma gained more attention in the 1970s with the rise of immune-suppressant treatment given after organ or bone marrow transplants and the
Society and culture
"Crazy cat-lady"
"Crazy cat-lady syndrome" is a term coined by news organizations to describe scientific findings that link the parasite
The term crazy cat-lady syndrome draws on both stereotype and popular cultural reference. It was originated as instances of the aforementioned afflictions were noted amongst the populace. A cat lady is a cultural stereotype of a woman who compulsively hoards and dotes upon cats. The biologist Jaroslav Flegr is a proponent of the theory that toxoplasmosis affects human behaviour.[101][102]
Notable cases
- Tennis player Arthur Ashe developed neurological problems from toxoplasmosis (and was later found to be HIV-positive).[103]
- Actor Merritt Butrick was HIV-positive and died from toxoplasmosis as a result of his already-weakened immune system.[104]
- Pedro Zamora, reality television personality and HIV/AIDS activist, was diagnosed with toxoplasmosis as a result of his immune system being weakened by HIV.[105]
- throne of Francehad congenital toxoplasmosis; his disability caused him to be overlooked in the line of succession.
- Actress Leslie Ash contracted toxoplasmosis in the second month of pregnancy.[106]
- British middle-distance runner Sebastian Coe contracted toxoplasmosis in 1983, which was probably transmitted by a cat while he trained in Italy.[107][108]
- Tennis player 1982 US Open.[109]
Other animals
Although T. gondii has the capability of infecting virtually all warm-blooded animals, susceptibility and rates of infection vary widely between different
Although infection with T. gondii has been noted in several species of Asian primates, seroprevalence of T. gondii antibodies were found for the first time in toque macaques (
Australian
It is estimated that 23% of wild swine worldwide are seropositive for T. gondii.[117] Seroprevalence varies across the globe with the highest seroprevalence in North America (32%) and Europe (26%) and the lowest in Asia (13%) and South America (5%).[117] Geographical regions located at higher latitudes and regions that experience warmer, humid climates are associated with increased seroprevalence of T. gondii among wild boar.[117] Wild boar infected with T. gondii pose a potential health risk for humans who consume their meat.[117]
Livestock
Among
Pigs
Worldwide, the percentage of pigs harboring viable parasites has been measured to be 3–71.43%
Sheep
Along with pigs, sheep and goats are among the most commonly infected livestock of epidemiological significance for human infection.[122] Prevalence of viable T. gondii in sheep tissue has been measured (via bioassay) to be as high as 78% in the United States,[126] and a 2011 survey of goats intended for consumption in the United States found a seroprevalence of 53.4%.[127] A single live attenuated vaccine, Toxovax, is currently available to mitigate the negative impacts of congenital toxoplasmosis on the sheep industry.[128][129]
Chickens
Due to a lack of exposure to the outdoors, chickens raised in large-scale indoor confinement operations are not commonly infected with T. gondii.[14] Free-ranging or backyard-raised chickens are much more commonly infected.[14] A survey of free-ranging chickens in the United States found its prevalence to be 17–100%, depending on the farm.[130] Because chicken meat is generally cooked thoroughly before consumption, poultry is not generally considered to be a significant risk factor for human T. gondii infection.[131]
Cattle
Although cattle and buffalo can be infected with T. gondii, the parasite is generally eliminated or reduced to undetectable levels within a few weeks following exposure.[14] Tissue cysts are rarely present in buffalo meat or beef, and meat from these animals is considered to be low-risk for harboring viable parasites.[47][122][132]
Horses
Horses are considered resistant to chronic T. gondii infection.[14] However, viable cells have been isolated from US horses slaughtered for export, and severe human toxoplasmosis in France has been epidemiologically linked to the consumption of horse meat.[47][133]
Domestic cats
In 1942, the first case of feline toxoplasmosis was diagnosed and reported in a domestic cat in Middletown, New York.[134] The investigators isolated oocysts from feline feces and found that the oocysts could be infectious for up to 12 months in the environment.[135]
The seroprevalence of T. gondii in
T. gondii infection rates in domestic cats vary widely depending on the cats' diets and lifestyles.
Most infected cats will shed oocysts only once in their lifetimes, for a period of about one to two weeks.[136] This shedding can release millions of oocysts, each capable of spreading and surviving for months.[136] An estimated 1% of cats at any given time are actively shedding oocysts.[14]
It is difficult to control the cat population with the infected oocysts due to lack of an effective vaccine. This remains a challenge in most cases and the programs that are readily available are questionable in efficacy.[143]
Rodents
Infection with T. gondii has been shown to
In rodents, T. gondii–induced behavioral changes occur through
T. gondii-infected rodents show a number of behavioral changes beyond altered responses to cat odors. Rats infected with the parasite show increased levels of activity and decreased
Marine mammals
A
Giant panda
Toxoplasma gondii has been reported as the cause of death of a
Research
Chronic infection with T. gondii has traditionally been considered asymptomatic in people with normal immune function.[169] Some evidence suggests latent infection may subtly influence a range of human behaviors and tendencies, and infection may alter the susceptibility to or intensity of a number of psychiatric or neurological disorders.[170][169]
In most of the current studies where positive correlations have been found between T. gondii antibody titers and certain behavioral traits or neurological disorders, T. gondii seropositivity tests are conducted after the onset of the examined disease or behavioral trait; that is, it is often unclear whether infection with the parasite increases the chances of having a certain trait or disorder, or if having a certain trait or disorder increases the chances of becoming infected with the parasite.[171] Groups of individuals with certain behavioral traits or neurological disorders may share certain behavioral tendencies that increase the likelihood of exposure to and infection with T. gondii; as a result, it is difficult to confirm causal relationships between T. gondii infections and associated neurological disorders or behavioral traits.[171]
Mental health
Some evidence links T. gondii to
Correlations have also been found between antibody
Neurological disorders
Latent infection has been linked to Parkinson's disease and Alzheimer's disease.[170]
Individuals with multiple sclerosis show infection rates around 15% lower than the general public.[179]
Traffic accidents
Latent T. gondii infection in humans has been associated with a higher risk of
Climate change
Climate change has been reported to affect the occurrence, survival, distribution and transmission of T. gondii.[181] T. gondii has been identified in the Canadian arctic, a location that was once too cold for its survival.[182] Higher temperatures increase the survival time of T. gondii.[181] More snowmelt and precipitation can increase the amount of T. gondii oocysts that are transported via river flow.[181] Shifts in bird, rodent, and insect populations and migration patterns can impact the distribution of T. gondii due to their role as reservoir and vector.[181] Urbanization and natural environmental degradation are also suggested to affect T. gondii transmission and increase risk of infection.[181]
See also
- Toxoplasmic chorioretinitis
- TORCH infection
- Pyrimethamine
References
- ^ a b c d e "Parasites – Toxoplasmosis (Toxoplasma infection) Disease". July 10, 2014. Archived from the original on 22 August 2015. Retrieved 22 August 2015.
- ^ PMID 23070557.
- ^ a b c d e f g "Parasites – Toxoplasmosis (Toxoplasma infection) Epidemiology & Risk Factors". March 26, 2015. Archived from the original on 23 August 2015. Retrieved 22 August 2015.
- ^ a b "Parasites – Toxoplasmosis (Toxoplasma infection) Diagnosis". January 10, 2013. Archived from the original on 22 August 2015. Retrieved 22 August 2015.
- ^ a b c "Parasites – Toxoplasmosis (Toxoplasma infection) Resources for Health Professionals". April 14, 2014. Archived from the original on 13 September 2015. Retrieved 22 August 2015.
- ^ PMID 23825877.
- ^ PMID 24662942.
Toxoplasmosis is becoming a global health hazard as it infects 30–50% of the world human population.
- PMID 33012669.
Accumulating evidence suggests that latent infection of Toxoplasma gondii is associated with a variety of neuropsychiatric and behavioral conditions.
- ^ a b "Parasites – Toxoplasmosis (Toxoplasma infection) Biology". March 17, 2015. Archived from the original on 28 August 2015. Retrieved 22 August 2015.
- ^ a b "Parasites – Toxoplasmosis (Toxoplasma infection) Prevention & Control". January 10, 2013. Archived from the original on 22 August 2015. Retrieved 22 August 2015.
- ^ PMID 19430635.
- S2CID 53726244.
- ^ PMID 22955326.
- ^ PMID 18508057.
- ^ a b "toxoplasmosis". Mayo Clinic. Archived from the original on 2015-09-08.
- PMID 11495859.
- ^ "Tachyzoite – an overview | ScienceDirect Topics". www.sciencedirect.com. Retrieved 2021-01-16.
- PMID 10391853.
- ^ "Lymphadenopathy" (PDF). UK Neqas Micro. Archived (PDF) from the original on 2016-04-24. Retrieved 2016-04-12.
- ^ "CDC Parasites – Toxoplasmosis (Toxoplasma infection) – Disease". Archived from the original on 7 March 2013. Retrieved 12 March 2013.
- S2CID 20384171.
- ^ Nawaz Khan, A (2015). "Imaging in CNS Toxoplasmosis". Medscape Web Site.
- ^ S2CID 1711188.
The seroprevalence of T. gondii in humans varies between 10 and 70% worldwide, depending on the region and increases significantly with age. Upon infection, the parasites persist as intraneuronal cysts in the central nervous system (CNS) for the lifetime of the host (1, Figure 1). Until recently, parasite persistence in healthy individuals was regarded as clinically asymptomatic. However, in the last decade, several reports have indicated that chronic cerebral toxoplasmosis may impact on the behaviour of its host (2).
- ^ Randall Parker: Humans Get Personality Altering Infections From Cats Archived 2005-12-17 at the Wayback Machine. September 30, 2003
- ^ S2CID 17132378.
The zoonotic pathogen Toxoplasma gondii infects over 30% of the human population. The intracellular parasite can persist lifelong in the CNS within neurons modifying their function and structure, thus leading to specific behavioural changes of the host. ... Furthermore, investigations of the human population have correlated Toxoplasma seropositivity with changes in neurological functions; however, the complex underlying mechanisms of the subtle behavioural alteration are still not fully understood. The parasites are able to induce direct modifications in the infected cells, for example by altering dopamine metabolism, by functionally silencing neurons as well as by hindering apoptosis.
- ^ PMID 19433092.
- PMID 25306262.
- PMID 23224444.
Nine of eleven studies using the Cattell's 16-Personality Factor self-report questionnaire found significant and consistent results for both genders. Seropositive men overall had lower regard for rules and higher vigilance (suspicious, jealous, rigid/inflexible) than seronegative men. In contrast, seropositive women had greater regard for rules and higher warmth than seronegative women. Both seropositive genders were more anxious than matched healthy-comparison subjects. ... Behavioral observations and interviews were completed to ascertain whether the gender differences found in self-report measures were replicated by objective measures. Seropositive men scored significantly lower than seronegative men on Self-Control, Clothes Tidiness, and Relationships. The differences were less impressive for the seropositive women, with only trends toward higher scores on Self-Control and Clothes Tidiness as compared with seronegative women. The authors view the study results as objective confirmation that T. gondii presence can change a human host's behaviors.
- S2CID 49234104.
- PMID 23390283.
- ISBN 0-07-138067-1.
- ^ PMID 22491772.
- PMID 3446034.
- ^ PMID 18775432.
- PMID 28955329.
- ^ PMID 16304607.
- ^ PMID 22876173.
- ^ PMID 19737817.
- ^ PMID 19028680.
- ^ PMID 18327664.
- PMID 36309013.
- ^ PMID 19217908.
- ISBN 9780123695420.
- ^ PMID 19018809.
- ^ PMID 27722100.
- ^ "Toxoplasmosis". Centers of Disease Control and Prevention. 2004-11-22. Archived from the original on 2006-10-06.
- ^ PMID 22618566.
- ^ Dubey, J.P. "Swine Toxoplasmosis". Veterinary Division – Animal Health Programs. Archived from the original on 2017-03-22.
- PMID 20691951.
- S2CID 8378877. Retrieved 8 November 2023.
- S2CID 12816757.
- ^ "Parasites – Toxoplasmosis (Toxoplasma infection)". Centers of Disease Control and Prevention. 2011-04-05. Archived from the original on 2015-08-28.
- PMID 7660566.
- ^ PMID 23714347.
- ^ PMID 21856107.
- ^ PMID 26493047.
- ^ "Circular Normativa sobre Cuidados Pré-Concepcionais – Direcção-Geral de Saúde" (PDF). Archived from the original (PDF) on 2011-07-16.
- ^ PMID 16446116.
- ^ [1] Archived August 24, 2011, at the Wayback Machine
- ^ PMID 18034857.
- ^ PMID 8712198.
- ^ PMID 12390281.
- PMID 10894691.
- S2CID 9423818.
- PMID 19663709.
- S2CID 9610443.
- ^ Ian Sample, science correspondent (2006-10-12). "Pregnant women infected by cat parasite more likely to give birth to boys, say researchers | Science". The Guardian. London. Archived from the original on 2014-02-19. Retrieved 2013-02-14.
- PMID 15715713.
- ^ PMID 11865443.
- ^ PMID 24808246.
- PMID 15004036.
- ^ PMID 33904818.

- PMID 16700697.
- ^ PMID 11060078.
- PMID 12776962.
- ^ "Congenital toxoplasmosis: MedlinePlus Medical Encyclopedia". medlineplus.gov. Retrieved 2018-02-26.
- PMID 29983776.
- ^ Macedo de Resende, Luciana. "Congenital toxoplasmosis: Auditory and language outcomes in early diagnosed and treated children".
- PMID 23019377.
- PMID 3661590.
- ^ "CDC – Toxoplasmosis – Resources for Health Professionals". www.cdc.gov. Archived from the original on 26 November 2016. Retrieved 5 December 2016.
- ^ "Toxoplasmosis – treatment key research". NAM & aidsmap. 2005-11-02. Archived from the original on 2007-10-22.
- PMID 12461021.
- PMID 12776962.
- PMID 19430661.
- PMID 16619149.
- ^ "Congenital Toxoplasmosis". Baby's First Test. Retrieved 2 April 2020.
- ^ PMID 17827351.
- PMID 21192848.
- from the original on 2016-08-17.
- PMID 19687043.
- ^ "CDC: Parasites – Toxoplasmosis (Toxoplasma infection) – Pregnant Women". Archived from the original on 7 March 2013. Retrieved 13 March 2013.
- PMID 9652380.
- ISBN 978-1-4767-3823-9.
- ^ "Laboratory Tests For The Diagnosis Of Toxoplasmosis". Toxoplasma Serology Laboratory. Archived from the original on 2007-12-23.
- ^ "How Your Cat Is Making You Crazy – Kathleen McAuliffe". The Atlantic. 2012-02-06. Archived from the original on 2013-06-03. Retrieved 2013-06-03.
- ^ "'Cat Lady' Conundrum – Rebecca Skloot". The New York Times. 2007-12-09. Archived from the original on 2017-01-18.
- S2CID 205073283.
- PMID 28222824.
- PMID 10894691.
- ^ Kathleen McAuliffe (March 2012). "How Your Cat is Making You Crazy". The Atlantic. Archived from the original on 2012-08-16.
- from the original on 2015-02-19.
- ^ Arthur Ashe, Tennis Star, is Dead at 49 Archived December 10, 2008, at the Wayback Machine New York Times (02/08/93)
- ^ Merritt Butrick, A Biography Archived 2011-07-13 at the Wayback Machine Angelfire.com, accessdate Mar 18, 2011
- ^ "The Face That Defined AIDS". Archived from the original on 2016-04-02.
- ^ "Pregnancy superfoods revealed". BBC News. January 10, 2001. Archived from the original on January 5, 2007. Retrieved May 25, 2010.
- ^ "Olympics bid Coes finest race". The Times. London. June 26, 2005. Archived from the original on May 10, 2011. Retrieved May 25, 2010.
- ^ "SPORTS PEOPLE; Coe's Disorder Rare". The New York Times. 3 September 1983. Retrieved 3 May 2018.
- ^ Brody, Jane E. (27 October 1982). "PERSONAL HEALTH". New York Times. Archived from the original on 27 August 2017.
- PMID 25407506.

- ^ from the original on 2016-01-01.
- ^ Dubey (2016), p. needed.
- PMID 30767889.

- S2CID 23829241.
- PMID 24533323.
- ^ Fancourt, Bronwyn (5 October 2014). "Toxoplasmosis: how feral cats kill wildlife without lifting a paw". The Conversation. Archived from the original on 23 December 2016. Retrieved 23 December 2016.
- ^ PMID 28917302.
- ^ PMID 19559531.
- ^ Dubey (2016), p. 145.
- ^ ISBN 978-3-7091-1553-4.
- PMID 24534616.

- ^ PMID 11113252.
- ^ Dubey (2016), pp. 145–151.
- ^ Dubey (2016), p. 153.
- ^ Dubey (2016), p. 154.
- PMID 18191859.
- PMID 21515278.
- PMID 36090161.)
{{cite journal}}: CS1 maint: unflagged free DOI (link - PMID 36310233.
- S2CID 9228587.
- ^ Weiss & Kim (2011), p. 723.
- PMID 31868577.

- from the original on 2017-09-08.
- S2CID 35266490. Archived from the originalon 2020-08-09. Retrieved 2018-12-29.
- S2CID 4207372.
- ^ PMID 20202907.
- PMID 23012380.
- S2CID 25574092.
- ^ Dubey (2016), p. 96.
- ^ Dubey (2016), p. 98.
- ^ Dubey (2016), p. 95.
- ^ Dubey (2016), p. 46.
- S2CID 17789584.
- ^ PMID 20608471.
- (PDF) from the original on 2015-09-04.
- ^ PMID 11007336.
- PMID 17404235.
- S2CID 24725619.
- S2CID 21601830.
- ^ S2CID 45290208.
- ^ S2CID 17253786.
- PMID 27453897.
Epigenetic modifications caused by addictive drugs play an important role in neuronal plasticity and in drug-induced behavioral responses. Although few studies have investigated the effects of AMPH on gene regulation (Table 1), current data suggest that AMPH acts at multiple levels to alter histone/DNA interaction and to recruit transcription factors which ultimately cause repression of some genes and activation of other genes. Importantly, some studies have also correlated the epigenetic regulation induced by AMPH with the behavioral outcomes caused by this drug, suggesting therefore that epigenetics remodeling underlies the behavioral changes induced by AMPH. If this proves to be true, the use of specific drugs that inhibit histone acetylation, methylation or DNA methylation might be an important therapeutic alternative to prevent and/or reverse AMPH addiction and mitigate the side effects generate by AMPH when used to treat ADHD.
- PMID 25486626.
- PMID 23643695.
Short-term increases in histone acetylation generally promote behavioral responses to the drugs, while sustained increases oppose cocaine's effects, based on the actions of systemic or intra-NAc administration of HDAC inhibitors. ... Genetic or pharmacological blockade of G9a in the NAc potentiates behavioral responses to cocaine and opiates, whereas increasing G9a function exerts the opposite effect (Maze et al., 2010; Sun et al., 2012a). Such drug-induced downregulation of G9a and H3K9me2 also sensitizes animals to the deleterious effects of subsequent chronic stress (Covington et al., 2011). Downregulation of G9a increases the dendritic arborization of NAc neurons, and is associated with increased expression of numerous proteins implicated in synaptic function, which directly connects altered G9a/H3K9me2 in the synaptic plasticity associated with addiction (Maze et al., 2010).
"G9a appears to be a critical control point for epigenetic regulation in NAc, as we know it functions in two negative feedback loops. It opposes the induction of ΔFosB, a long-lasting transcription factor important for drug addiction (Robison and Nestler, 2011), while ΔFosB in turn suppresses G9a expression (Maze et al., 2010; Sun et al., 2012a). ... Also, G9a is induced in NAc upon prolonged HDAC inhibition, which explains the paradoxical attenuation of cocaine's behavioral effects seen under these conditions, as noted above (Kennedy et al., 2013). GABAA receptor subunit genes are among those that are controlled by this feedback loop. Thus, chronic cocaine, or prolonged HDAC inhibition, induces several GABAA receptor subunits in NAc, which is associated with increased frequency of inhibitory postsynaptic currents (IPSCs). In striking contrast, combined exposure to cocaine and HDAC inhibition, which triggers the induction of G9a and increased global levels of H3K9me2, leads to blockade of GABAA receptor and IPSC regulation.
- PMID 23199404.
- PMID 25786129.
- PMID 23225873.
- ^ PMID 22431975.
- S2CID 33572709.
- PMID 16157341.
- ^ "Treating Disease in the Developing World". Talk of the Nation Science Friday. National Public Radio. December 16, 2005. Archived from the original on April 27, 2006.
- ^ "Parasite in cats killing sea otters". NOAA magazine. National Oceanic and Atmospheric Administration. 21 January 2003. Archived from the original on 25 December 2007. Retrieved 24 November 2007.
- ^ Diep, Francie (September 3, 2019). "What's Killing California's Sea Otters? House Cats". The New York Times. Retrieved 9 September 2019.
- ^ a b Dawson, Teresa. "Cat Disease Threatens Endangered Monk Seals". Scientific American. Retrieved 11 October 2017.
- S2CID 13562317.
- ^ "3 Schizophrenia". Archived from the original on 2010-01-02.
- ^ Sidhartha Banerjee (October 15, 2018). "Parasite spread by cats threatens Quebec's endangered belugas(whales)". CBC News.
- PMID 20097009.
- ^ PMID 29068607.
- ^ PMID 23225872.
- ^ PMID 23225875.
- ^ from the original on 2015-09-04.
- ^ (PDF) from the original on 2015-09-04.
- ^ PMID 23433494.
- PMID 17426051.
- PMID 27889597.
- PMID 22325983.
- PMID 26886853.
- S2CID 33082008.
- S2CID 49234104.
- ^ PMID 26965989.
- S2CID 4448339.
- Parts of this article are taken from the public domain CDC factsheet: Toxoplasmosis
Bibliography
- Weiss, L. M.; Kim, K. (28 April 2011). Toxoplasma gondii: The Model Apicomplexan. Perspectives and Methods. Academic Press. ISBN 978-0-08-047501-1. Retrieved 12 March 2013.
- Dubey, J. P. (2016). Toxoplasmosis of Animals and Humans (2nd ed.). ISBN 9781420092363
- Dubey JP, Lindsay DS, Speer CA (April 1998). "Structures of Toxoplasma gondii tachyzoites, bradyzoites, and sporozoites and biology and development of tissue cysts". Clinical Microbiology Reviews. 11 (2): 267–299. PMID 9564564.
- Jaroslav Flegr (2011). Pozor, Toxo!. Academia, Prague, Czech Republic. ISBN 978-80-200-2022-2. Archived from the originalon 2017-07-21. Retrieved 2014-10-04.
External links
- How a cat-borne parasite infects humans (National Geographic)
- Toxoplasmosis at Merck Manual of Diagnosis and Therapy Professional Edition
- Toxoplasmosis at Health Protection Agency (HPA), United Kingdom
- Pictures of Toxoplasmosis Medical Image Database
- Video-Interview with Professor Robert Sapolsky on Toxoplasmosis and its effect on human behavior (24:27 min)
- "Toxoplasmosis". MedlinePlus. U.S. National Library of Medicine.
