Treponema pallidum
| Treponema pallidum | |
|---|---|

| |
| Scientific classification | |
| Domain: | Bacteria |
| Phylum: | Spirochaetota |
| Class: | Spirochaetia |
| Order: | Spirochaetales |
| Family: | Treponemataceae |
| Genus: | Treponema |
| Species: | T. pallidum
|
| Binomial name | |
| Treponema pallidum | |
Treponema pallidum, formerly known as Spirochaeta pallida, is a
Subspecies
Three subspecies of T. pallidum are known:[4]
- Treponema pallidum pallidum, which causes syphilis
- T. p. endemicum, which causes bejel or endemic syphilis
- T. p. pertenue, which causes yaws
The three subspecies causing yaws, bejel, and syphilis are morphologically and serologically indistinguishable.[1] These bacteria were originally classified as members of separate species, but DNA hybridization analysis indicates they are members of the same species. Treponema carateum, the cause of pinta, remains a separate species because no isolate is available for DNA analysis.[5] Disease transmittance in subspecies T. p. endemicum and T. p. pertenue is considered non-venereal.[6] T. p. pallidum is the most invasive pathogenic subspecies, while T. carateum is the least invasive of the species. T. p. endemicum and T. p. pertenue are intermediately invasive.[1]
Microbiology
Physiology

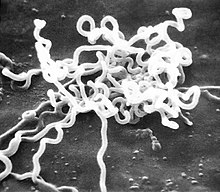
Treponema pallidum is a helically shaped bacterium with high
Outer membrane
The outer membrane (OM) of T. pallidum has several features that have made it historically difficult to research. These include details such as its low protein content, its fragility, and that it contains fewer gene sequences related to other gram negative outer membranes.[12] Progress has been made using genomic sequencing and advanced computational models. The treponemal outer membrane proteins are key factors for the bacterium's pathogenesis, persistence, and immune evasion strategies. The relatively low protein content prevents antigen recognition by the immune system and the proteins that do exist protrude out of the OM, enabling its interaction with the host.[12] Treponema's reputation as a "stealth pathogen" is primarily due to this unique OM structure, which serves to evade immune detection.[12]
TP0326
TP0326 is an ortholog of the β-barrel assembly machine Bam A. BamA apparatus inserts newly synthetized and exported outer membrane proteins into the outer membrane [13]
TP0965
TP0965 is a protein that is critical for membrane fusion in T. pallidum, and is located in the periplasm.[14] TP0965 causes endothelial barrier dysfunction, a hallmark of late-stage pathogenesis of syphilis.[15] It does this by reducing the expression of tight junction proteins, which in turn increases the expression of adhesion molecules and endothelial cell permeability, which eventually leads to disruption of the endothelial layer.[16]
TP0453
TP0453 is a 287 amino acid protein associated with the inner membrane of the microbe's outer membrane.[17] This protein lacks the extensive beta sheet structure that is characteristic of other membrane proteins, and does not traverse the outer membrane.[18] This protein's function has been hypothesized to be involved with control of nutrient uptake.[19]
TP0624
Outer Membrane Protein A (OmpA) domain-containing proteins are necessary for maintaining structural integrity in Gram-negative bacteria. These domains contain peptidoglycan binding sites which creates a "structural bridge between the peptidoglycan layer and the outer memebrane."
Treponema repeat family of proteins
The Treponema repeat family of proteins (Tpr) are proteins expressed during the infection process. Tprs are formed by a conserved N-terminal domain, an amino-terminal stretch of about 50 amino acids, a central variable region, and a conserved C-terminal domain.[13] The many different types of Tpr include TprA, TprB, TprC, TprD, and TprE, but variability of TprK is the most relevant due to the immune escape characteristics it allows.[21]
Antigen variation in TprK is regulated by gene conversion. In this way, fragments of the seven variable regions (V1–V7) present in TprK and the 53 donor sites of TprD can be combined to produce new structured sequences.[22] TprK antigen variation can help T. pallidum to evade a strong host immune reaction and can also allow the reinfection of individuals. This is possible because the newly structured proteins can avoid antibody-specific recognition.[21]
To introduce more phenotypic diversity, T. pallidum may undergo phase variation. This process mainly happens in TprF, TprI, TprG, TprJ, and TprL, and it consists of a reversible expansion or contraction of polymeric repeats. These size variations can help the bacterium to quickly adapt to its microenvironment, dodge immune response, or even increase affinity to its host.[22]
Culture
In the past century since its initial discovery, culturing the bacteria in vitro has been difficult.[23] Without the ability to grow and maintain the bacteria in a laboratory setting, discoveries regarding its metabolism and antimicrobial sensitivity were greatly impaired.[24] However, successful long-term cultivation of T. pallidum in vitro was reported in 2017.[23] This was achieved using Sf1Ep epithelial cells from rabbits, which were a necessary condition for the continued multiplication and survival of the system.[25] The medium TpCM-2 was used, an alteration of more simple media which previously only yielded a few weeks of culture growth.[25] This success was the result of switching out minimal essential medium (MEM) with CMRL 1066, a complex tissue culture medium.[23] With development, new discoveries about T. pallidum's requirements for growth and gene expression may occur and in turn, yield research beneficial for the treatment and prevention of syphilis, outside of a host.[26] However, continuous efforts to grow T. pallidum in axenic culture have been unsuccessful, indicating that it does not satisfy Koch's postulates.[27] The challenge likely stems from the organism's strong adaptation to residing in mammalian tissue, resulting in a reduced genome and significant impairments in metabolic and biosynthetic functions.[25]
Genome
The chromosomes of the T. pallidum species are small, about 1.14 Mbp. Their DNA sequences are more than 99.7% identical.[28] About 92.9% of DNA was determined to be open reading frames, 55% of which had predicted biological functions.[2] The genome ofT. pallidum was first sequenced in 1998.[29] T. pallidum is not obtainable in a pure culture, meaning that this sequencing played an important role in filling gaps of understanding regarding the microbes' functions. T. pallidum was found to rely on its host for many molecules typically provided by biosynthetic pathways, and it is missing genes responsible for encoding key enzymes in oxidative phosphorylation and the tricarboxylic acid cycle.[30] The T. pallidum group and its reduced genome is likely the result of various adaptations, such that it no longer contains the ability to synthesize fatty acids, nucleic acids, and amino acids, instead relying on its mammalian hosts for these materials.[26] The recent sequencing of the genomes of several spirochetes permits a thorough analysis of the similarities and differences within this bacterial phylum and within the species.[31][32][33] T. pallidum has one of the smallest bacterial genomes and has limited metabolic capabilities, reflecting its adaptation through genome reduction to the rich environment of mammalian tissue. T. pallidum is characterized by its helical, corkscrew-like shape.[34] To avoid antibodies attacking it, the cell has few proteins exposed on the outer membrane sheath.[35] Its chromosome is about 1000 kilobase pairs and is circular with a 52.8% G + C average.[36] Sequencing has revealed a bundle of 12 proteins and some putative hemolysins are potential virulence factors of T. pallidum.[37] These virulence factors are thought to contribute to the bacterium's ability to evade the immune system and cause disease.[38]
Clinical significance
The clinical features of syphilis, yaws, and bejel occur in multiple stages that affect the skin. The skin lesions observed in the early stage last for weeks or months. The skin lesions are highly infectious, and the spirochetes in the lesions are transmitted by direct contact. The lesions regress as the immune response develops against T. pallidum. The latent stage that results can last a lifetime in many cases. In a few cases, the disease exits latency and enters a tertiary phase, in which destructive lesions of skin, bone, and cartilage ensue. Unlike yaws and bejels, syphilis in its tertiary stage often affects the heart, eyes, and nervous system, as well.[5]
Syphilis
Treponema pallidum pallidum is a motile spirochete that is generally acquired by close
The incubation period for a T. p. pallidum infection is usually around 21 days, but can range from 10 to 90 days.[40]
Laboratory identification
Treponema pallidum was first microscopically identified in syphilitic chancres by
Treatment
During the early 1940s, rabbit models in combination with the drug
Vaccine
No vaccine for syphilis is available as of 2024. The outer membrane of T. pallidum has too few surface proteins for an antibody to be effective. Efforts to develop a safe and effective syphilis vaccine have been hindered by uncertainty about the relative importance of humoral and cellular mechanisms to protective immunity,[45] and because T. pallidum outer membrane proteins have not been unambiguously identified.[46][47] In contrast, some of the known antigens are intracellular, and antibodies are ineffective against them to clear the infection.[48][49][50] In the last century, several prototypes have been developed, and while none of them provided protection from the infection, some prevented bacteria from disseminating to distal organs and promoted accelerated healing.[51]
References
- ^ PMID 21413263. Retrieved 13 February 2019.
- ^ PMID 11200228.
- PMID 16954278.
- PMID 25157125.
- ^ PMID 24396138.
- ^ "Other Treponema pallidum infections | Immigrant and Refugee Health | CDC". www.cdc.gov. 26 February 2019. Retrieved 12 November 2019.
- PMID 29022569.
- S2CID 252916923.
- ^ PMID 20850455.
- PMID 7014451.
- S2CID 40913042.
- ^ PMID 28849315.
- ^ PMID 33972353.
- PMID 35869970.
- PMID 15972547.
- PMID 25514584.
- PMID 35869970.
- PMID 16159783.
- PMID 21965687.
- ^ PMID 27832149.
- ^ PMID 9989979.
- ^ S2CID 252994863.
- ^ PMID 29946052.
- PMID 28849315.
- ^ PMID 33622721.
- ^ PMID 33599121.
- PMID 27832942.
- S2CID 4826749.
- S2CID 8641048.
- ISBN 978-1-260-21188-7.
- PMID 23449808.
- PMID 28787460.
- PMID 15064399.
- ^ Clark DP, Dunlap PV, Madigan JT, Martinko JM (2009). Brock Biology of Microorganisms. San Francisco: Pearson. p. 79.
- ISBN 978-1-260-21188-7.
- S2CID 8641048.
- PMID 9862125.
- PMID 9862125. Retrieved 18 November 2023.
- ^ Arora N, Sadovsky Y, Dermody TS, Coyne CB. Microbial Vertical Transmission during Human Pregnancy. Cell Host Microbe. 2017 May 10;21(5):561-567. doi: 10.1016/j.chom.2017.04.007. PMID 28494237; PMCID: PMC6148370.
- ^ "STD Facts – Syphilis (Detailed)". Centers for Disease Control (CDC). Retrieved 19 April 2017.
- Schaudinn FR, Hoffmann E (1905). "Vorläufiger Bericht über das Vorkommen von Spirochaeten in syphilitischen Krankheitsprodukten und bei Papillomen" [Preliminary report on the occurrence of Spirochaetes in syphilitic chancres and papillomas]. Arbeiten aus dem Kaiserlichen Gesundheitsamte. 22: 527–534.
- ISBN 978-0-7817-8215-9.
- ^ a b Fantry LE, Tramont EC. "Treponema Pallidum (Syphilis)". Infectious Disease and Antimicrobial Agents. Retrieved 12 November 2019 – via www.antimicrobe.org.
- ^ PMID 19805553.
- S2CID 255333392.
- PMID 17890130.
- PMID 24135571.
- PMID 3884491.
- PMID 8246847.
- PMID 19820083.
- PMID 37090699.
Further reading
- Althouse BM, Hébert-Dufresne L (October 2014). "Epidemic cycles driven by host behaviour". Journal of the Royal Society, Interface. 11 (99): 20140575. PMID 25100316.
External links
- "Syphilis- CDC Fact Sheet." Centers for Disease Control and Prevention. May. 2004. Centers for Disease Control and Prevention. 7 February 2006
