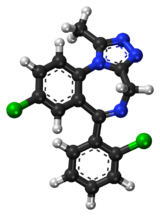
Triazolam
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Halcion |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a684004 |
| License data | |
| Pregnancy category |
|
| Routes of administration | Oral (by mouth) |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 44% (oral route), 53% (sublingual) |
| Metabolism | Liver |
| Onset of action | 15–30 minutes[4] |
| Elimination half-life | 1.5–5.5 hours |
| Excretion | Kidney |
| Identifiers | |
| |
JSmol) | |
| |
| |
| (verify) | |
Triazolam, sold under the brand name Halcion among others, is a
Triazolam was initially patented in 1970 and went on sale in the United States in 1982.[8] In 2017, it was the 289th most commonly prescribed medication in the United States, with more than one million prescriptions.[9]
Medical uses
Triazolam is usually used for short-term treatment of acute
Triazolam is frequently prescribed as a sleep aid for passengers travelling on short- to medium-duration flights. If this use is contemplated, the user avoiding the consumption of alcoholic beverages is especially important, as is trying a ground-based "rehearsal" of the medication to ensure that the side effects and potency of this medication are understood by the user prior to using it in a relatively more public environment (as disinhibition can be a common side effect, with potentially severe consequences). [citation needed] Triazolam causes anterograde amnesia, which is why so many dentists administer it to patients undergoing even minor dental procedures. This practice is known as sedation dentistry.[11]
Side effects
- Relatively common (>1% of patients): somnolence, dizziness, feeling of lightness, coordination problems
- Less common (0.9% to 0.5% of patients): euphoria, tachycardia, tiredness, confusional states/memory impairment, cramps/pain, depression, visual disturbances
- Rare (<0.5% of patients): constipation, taste alteration, diarrhea, dry mouth, dermatitis/allergy, dreams/nightmares, insomnia, paresthesia, tinnitus, dysesthesia, weakness, congestion[12]
Triazolam, although a short-acting benzodiazepine, may cause residual impairment into the next day, especially the next morning. A
In September 2020, the US Food and Drug Administration (FDA) required the boxed warning be updated for all benzodiazepine medicines to describe the risks of abuse, misuse, addiction, physical dependence, and withdrawal reactions consistently across all the medicines in the class.[15]
Tolerance, dependence, and withdrawal
A review of the literature found that long-term use of
Other withdrawal symptoms can range from mild unpleasant feelings to a major withdrawal syndrome, including stomach cramps, vomiting, muscle cramps, sweating, tremor, and in rare cases, convulsions.[12]
Contraindications
Benzodiazepines require special precautions if used in the elderly, during pregnancy, in children, in
Elderly
Triazolam, similar to other benzodiazepines and
An extensive review of the medical literature regarding the management of insomnia and the elderly found considerable evidence of the effectiveness and durability of nondrug treatments for insomnia in adults of all ages and that these interventions are underused. Compared with the benzodiazepines including triazolam, the nonbenzodiazepine sedative-hypnotics appeared to offer few, if any, significant clinical advantages in efficacy or tolerability in elderly persons. Newer agents with novel mechanisms of action and improved safety profiles, such as the melatonin agonists, hold promise for the management of chronic insomnia in elderly people. Long-term use of sedative-hypnotics for insomnia lacks an evidence base and has traditionally been discouraged for reasons that include concerns about such potential adverse drug effects as cognitive impairment, anterograde amnesia, daytime sedation, motor incoordination, and increased risk of motor vehicle accidents and falls.[21] One study found no evidence of sustained hypnotic efficacy throughout the 9 weeks of treatment for triazolam.[21]
In addition, the effectiveness and safety of long-term use of these agents remain to be determined. More research is needed to evaluate the long-term effects of treatment and the most appropriate management strategy for elderly persons with chronic insomnia.[22]
Interactions
Ketoconazole and itraconazole have a profound effect on the pharmacokinetics of triazolam, leading to greatly enhanced effects.[23] Anxiety, tremor, and depression have been documented in a case report following administration of nitrazepam and triazolam. Following administration of erythromycin, repetitive hallucinations and abnormal bodily sensations developed. The patient had, however, acute pneumonia, and kidney failure.[citation needed] Co-administration of benzodiazepine drugs at therapeutic doses with erythromycin may cause serious psychotic symptoms, especially in those with other physical complications.[24] Caffeine reduces the effectiveness of triazolam.[25] Other important interactions include cimetidine, diltiazem, fluconazole, grapefruit juice, isoniazid, itraconazole, nefazodone, rifampicin, ritonavir, and troleandomycin.[26][27] Triazolam should not be administered to patients on efavirenz/emtricitabine/tenofovir (Atripla).[28]
Overdose
Symptoms of an overdose[6][unreliable medical source?] include:
- Coma
- Hypoventilation (respiratory depression)
- Somnolence (drowsiness)
- Slurred speech
- Seizures[12]
Death can occur from triazolam overdose, but is more likely to occur in combination with other depressant drugs such as opioids, alcohol, or tricyclic antidepressants.[29]
Pharmacology
The pharmacological effects of triazolam are similar to those of most other
Society and culture
Recreational use
Triazolam, like other benzodiazepines, is susceptible to misuse and abuse. Its rapid onset of action and short half life contribute to its abuse potential, but its relative obscurity compared to other fast-acting benzodiazepines (such as alprazolam or lorazepam) prevent its abuse from becoming particularly commonplace. Likewise, because it is not prescribed as often or as readily as alprazolam or lorazepam, there is less triazolam available to be diverted for recreational use.[33]
Legal status
Its use at low doses has been deemed acceptable by the US FDA and in several other countries.[6][unreliable medical source?]
Triazolam is a
Brand names
The drug is marketed in English-speaking countries under the brand names Apo-Triazo, Halcion, Hypam, and Trilam. Other names include 2'-chloroxanax, chloroxanax, triclazolam, and chlorotriazolam.[citation needed]
References
- ^ a b "Triazolam (Halcion) Use During Pregnancy". Drugs.com. 18 September 2020. Retrieved 24 October 2020.
- FDA. Retrieved 22 October 2023.
- ^ Anvisa (31 March 2023). "RDC Nº 784 - Listas de Substâncias Entorpecentes, Psicotrópicas, Precursoras e Outras sob Controle Especial" [Collegiate Board Resolution No. 784 - Lists of Narcotic, Psychotropic, Precursor, and Other Substances under Special Control] (in Brazilian Portuguese). Diário Oficial da União (published 4 April 2023). Archived from the original on 3 August 2023. Retrieved 16 August 2023.
- ^ "What Is Triazolam Used For?". www.icliniq.com. 1 November 2022. Retrieved 30 January 2023.
- ^ "Benzodiazepine Names". non-benzodiazepines. Archived from the original on 8 December 2008. Retrieved 29 December 2008.
- ^ a b c d e Wishart, David (2006). "Triazolam". DrugBank. Retrieved 23 March 2006.
- PMID 18855614.
- ISBN 9780190292010.
- ^ "Triazolam - Drug Usage Statistics". ClinCalc. Retrieved 7 October 2022.
- PMID 7901174.
- ^ "Comparison of Triazolam and Zaleplon for Sedation of Dental Patient". Dentistry Today. September 2005.
- ^ a b c "Halcion- triazolam tablet". DailyMed. 10 December 2019. Retrieved 23 October 2020.
- S2CID 25592318.
- PMID 2068441.
- ^ "FDA expands Boxed Warning to improve safe use of benzodiazepine drug". U.S. Food and Drug Administration (FDA). 23 September 2020. Retrieved 23 September 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- PMID 10533351.
- PMID 430730.
- PMID 19900604.
- ^ "Halcion triazolam tablets" (PDF). www.fda.gov. Archived from the original (PDF) on 6 November 2003. Retrieved 15 January 2022.
- PMID 20171127.
- ^ S2CID 24226217.
- PMID 16860264.
- S2CID 39127216.
- S2CID 22742117.
- PMID 1351673.
- S2CID 1543185. Archived from the original(PDF) on 9 July 2007.
- PMID 16380358.
- ^ "Medicines You Should Not Take with Atripla". Bristol-Myers Squibb & Gilead Sciences, LLC. 2008. Archived from the original on 25 April 2010. Retrieved 3 January 2010.
- PMID 9153780.
- PMID 2570451.
- ^ Professor heather Ashton (April 2007). "Benzodiazepine equivalency table". Archived from the original on 28 September 2007. Retrieved 23 September 2007.
- PMID 2983169.
- PMID 16336040.
- ^ "List of psychotropic substances under international control" (PDF). Green list. International Narcotics Control Board. Archived from the original (PDF) on 31 August 2012. Retrieved 23 March 2006.
