Triiodothyronine
 | |
 | |
 | |
| Names | |
|---|---|
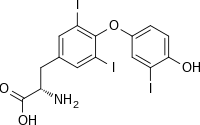
| IUPAC name
(2S)-2-amino-3-[4-(4-hydroxy-3-iodophenoxy)-3,5-diiodophenyl]propanoic acid
| |
| Other names
triiodothyronine
T3 3,3′,5-triiodo-L-thyronine | |
| Identifiers | |
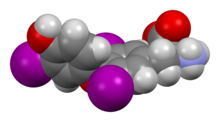
3D model (
JSmol ) |
|
| 2710227 | |
| ChEBI | |
| ChEMBL | |
| ChemSpider | |
| DrugBank | |
ECHA InfoCard
|
100.027.272 |
| EC Number |
|
IUPHAR/BPS |
|
| KEGG | |
PubChem CID
|
|
| UNII | |
CompTox Dashboard (EPA)
|
|
| |
| |
| Properties | |
| C15H12I3NO4 | |
| Molar mass | 650.977 g·mol−1 |
| Hazards | |
| GHS labelling: | |

| |
| Warning | |
| H315, H319, H335 | |
| P261, P264, P271, P280, P302+P352, P304+P340, P305+P351+P338, P312, P321, P332+P313, P337+P313, P362, P403+P233, P405, P501 | |
| NFPA 704 (fire diamond) | |
Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa).
| |
Triiodothyronine, also known as T3, is a
Production of T3 and its
At the cellular level, T3 is the body's more active and potent thyroid hormone.[2] T3 helps deliver oxygen and energy to all of the body's cells, its effects on target tissues being roughly four times more potent than those of T4.[2] Of the thyroid hormone that is produced, just about 20% is T3, whereas 80% is produced as T4. Roughly 85% of the circulating T3 is later formed in the liver and anterior pituitary by removal of the iodine atom from the carbon atom number five of the outer ring of T4. In any case, the concentration of T3 in the human blood plasma is about one-fortieth that of T4. The half-life of T3 is about 2.5 days.[3] The half-life of T4 is about 6.5 days.[4] T3 levels start to rise 45 minutes after administration and peak at about 2.5 hours. Although manufacturer of Cytomel states half-life to be 2.5 days the half-life variability is great and can vary depending on the thyroid status of the patient. Newer studies have found the pharmakokinetics of T3 to be complex and the half-life to vary between 10 – 22 hours.[5]
Production
Synthesis from T4
T3 is the more metabolically active hormone produced from T4. T4 is deiodinated by three deiodinase enzymes to produce the more-active triiodothyronine:
- Type I present in liver, kidney, thyroid, and (to a lesser extent) pituitary; it accounts for 80% of the deiodination of T4.
- Type II present in CNS, pituitary, brown adipose tissue, and heart vessel, which is predominantly intracellular. In the pituitary, it mediates negative feedback on thyroid-stimulating hormone.
- Type III present in placenta, CNS, and hemangioma. This deiodinase converts T4 into reverse T3, which, unlike T3, is inactive.
T4 is synthesised in the thyroid follicular cells as follows.
- The sodium-iodide symportertransports two sodium ions across the basement membrane of the follicular cells along with an iodine ion. This is a secondary active transporter that utilises the concentration gradient of Na+ to move I− against its concentration gradient.
- I− is moved across the apical membrane into the colloid of the follicle.
- Thyroperoxidaseoxidises I− to form the I radical.
- The thyroperoxidase iodinates the tyrosyl residues of the thyroglobulin within the colloid. The thyroglobulin was synthesised in the ER of the follicular cell and secreted into the colloid.
- Thyroid-stimulating hormone (TSH) released from the anterior pituitary gland binds the TSH receptor (a Gs protein-coupled receptor) on the basolateral membrane of the cell and stimulates the endocytosis of the colloid.
- The endocytosed vesicles fuse with the lysosomes of the follicular cell. The lysosomal enzymes cleave the T4 from the iodinated thyroglobulin.
- These vesicles are then exocytosed, releasing the thyroid hormones.

Direct synthesis
The thyroid gland also produces small amounts of T3 directly. In the
The small amount of T3 could be important because different tissues have different sensitivities to T4 due to differences in deiodinase ubiquitination in different tissues.[7] This once again raises the question if T3 should be included in thyroid hormone replacement therapy (THRT).
Mechanism of action
T3 and T4 bind to
Transportation
T3 and T4 are carried in the blood, bound to plasma proteins. This has the effect of increasing the half-life of the hormone and decreasing the rate at which it is taken up by peripheral tissues. There are three main proteins that the two hormones are bound to. Thyroxine-binding globulin (TBG) is a glycoprotein that has a higher affinity for T4 than for T3. Transthyretin is also a glycoprotein, but only carries T4, with hardly any affinity at all for T3. Finally, both hormones bind with a low affinity to serum albumin, but, due to the large availability of albumin, it has a high capacity.
The saturation of binding spots on thyronine-binding globulin (TBG) by endogenous T3 can be estimated by the triiodothyronine resin uptake test. The test is performed by taking a
Effects
T3 increases the
Skeletal growth
Thyroid hormones are essential for normal growth and skeletal maturation.
Protein
T3 stimulates the production of RNA polymerase I and II and, therefore, increases the rate of protein synthesis. It also increases the rate of protein degradation, and, in excess, the rate of protein degradation exceeds the rate of protein synthesis. In such situations, the body may go into negative ion balance.[further explanation needed]
Lipids
T3 stimulates the breakdown of cholesterol and increases the number of LDL receptors, thereby increasing the rate of lipolysis.
Heart
T3 increases the heart rate and force of contraction, thus increasing
Development
T3 has profound effect upon the developing embryo and infants. It affects the lungs and influences the postnatal growth of the central nervous system. It stimulates the production of
Neurotransmitters
T3 may increase serotonin in the brain, in particular in the cerebral cortex, and down-regulate 5HT-2 receptors, based on studies in which T3 reversed learned helplessness in rats and physiological studies of the rat brain.[15]
Physiological function
Thyroid hormones act to increase protein turnover. This might serve an adaptive function in regard to long-term calorie restriction with adequate protein.[16][17] When calories are in short supply, reduction in protein turnover may ameliorate the effects of the shortage.
Measurement
Triiodothyronine can be measured as free triiodothyronine, which is an indicator of triiodothyronine activity in the body. It can also be measured as total triiodothyronine, which also depends on the triiodothyronine that is bound to thyroxine-binding globulin.[18]
Uses
Treatment of depressive disorders
The addition of triiodothyronine to existing treatments such as
Use as a fat loss supplement
3,5-Diiodo-L-thyronine and 3,3′-diiodo-L-thyronine are used as ingredients in certain over-the-counter fat-loss supplements, designed for bodybuilding. Several studies have shown that these compounds increase the metabolization of fatty acids and the burning of adipose fat tissue in rats.[21][22]
Alternative medicine
Triiodothyronine has been used to treat
History
In 1950 Dr
While Gross & Pitt-Rivers are normally credited with discovering T3, this compound was actually first isolated by the biochemists Hird & Trikojus at the University of Melbourne in 1948.[26] It has been suggested that their published paper was little-known and therefore easily ignored.[27] It has also been stated that Pitt-Rivers had read this paper but failed to mention it.[28]
See also
References
- ^ Bowen R (2010-07-24). "Physiologic Effects of Thyroid Hormones". Colorado State University. Retrieved 2013-09-29.
- ^ a b "How Your Thyroid Works – "A delicate Feedback Mechanism"". endocrineweb. 2012-01-30. Retrieved 2013-09-29.
- ^ "Cytomel (Liothyronine Sodium) Drug Information". RxList. 2011-01-03. Retrieved 2013-09-29.
- ^ Irizarry L (23 April 2014). "Thyroid Hormone Toxicity". Medscape. WedMD LLC. Retrieved 2 May 2014.
- PMID 24977379.
- LCCN 2004051158.
- PMID 25555216.
- PMID 2254444.
- PMID 18651367.
- ^ References used in image are found in image article in Commons:Commons:File:Thyroid_system.png#References.
- ^ triiodothyronine resin uptake test from Farlex Medical Dictionary, citing: Mosby's Medical Dictionary, 8th edition. 2009, Elsevier.
- ^ OCLC 966608835.
- ^ OCLC 1076268769.
- ^ "Thyroid physiology and tests of function". Anaesthetist.com.
- S2CID 43784239.
- PMID 16720655.
- S2CID 20574006.
- ^ Military Obstetrics & Gynecology – Thyroid Function Tests In turn citing: Operational Medicine 2001, Health Care in Military Settings, NAVMED P-5139, May 1, 2001, Bureau of Medicine and Surgery, Department of the Navy, 2300 E Street NW, Washington, D.C., 20372-5300
- ^ PMID 19108898.
- PMID 19215985.
- PMID 9461551.
- S2CID 1624615.
- ^ "ATA Statement on "Wilson's Syndrome"". American Thyroid Association. 24 May 2005.
- ^ Smith TS (2018-08-05). "HISTORY: Rosalind Pitt-Rivers, the co-discoverer of T3 hormone". Thyroid Patients Canada. Retrieved 2022-09-13.
- PMID 14898765.
- PMID 18875255.
- hdl:1959.4/69845.
- ISSN 1833-7538. Retrieved 2023-07-27.
External links
- Triiodothyronine bound to proteins in the PDB
- T3 at Lab Tests Online

