Vascular surgery
This article needs additional citations for verification. (June 2021) |
| Vascular surgery | |
|---|---|
 Open infrarenal aortic repair model | |
| ICD-9-CM | 38-39 |
| MeSH | D014656 |
| OPS-301 code | 5-38...5-39 |
Vascular surgery is a surgical subspecialty in which
History
Early leaders of the field included Russian surgeon Nikolai Korotkov, noted for developing early surgical techniques, American interventional radiologist Charles Theodore Dotter who is credited with inventing minimally invasive angioplasty (1964), and Australian Robert Paton, who helped the field achieve recognition as a specialty. Edwin Wylie of San Francisco was one of the early American pioneers who developed and fostered advanced training in vascular surgery and pushed for its recognition as a specialty in the United States in the 1970s. The most notable historic figure in vascular surgery is the 1912 Nobel Prize winning surgeon, Alexis Carrel for his techniques used to suture vessels.
Evolution

The specialty continues to be based on operative arterial and venous surgery but since the early 1990s has evolved greatly. There is now considerable emphasis on minimally invasive alternatives to surgery. The field was originally pioneered by
The surgeon Dr.
The treatment of the aorta, the body's largest artery, dates back to Greek surgeon Antyllus, who first performed surgeries for various aneurysms in the second century AD. Modern treatment of aortic diseases stems from development and advancements from
Dr.
The development of endovascular surgery has been accompanied by a gradual separation of vascular surgery from its origin in general surgery. Most vascular surgeons would now confine their practice to vascular surgery and, similarly, general surgeons would not be trained or practise the larger vascular surgery operations or most endovascular procedures. More recently, professional vascular surgery societies and their training program have formally separated vascular surgery into a separate specialty with its own training program, meetings and accreditation. Notable societies are Society for Vascular Surgery (SVS), USA; Australia and New Zealand Society of Vascular Surgeons (ANZSVS). Local societies also exist (e.g., New South Wales Vascular and Melbourne Vascular Surgical Association (MVSA)). Larger societies of surgery actively separate and encourage specialty surgical societies under their umbrella (e.g., Royal Australasian College of Surgeons (RACS)).
Currently
Arterial and venous disease treatment by
A recent trend in the United States is the stand-alone day angiography facility associated with a private vascular surgery clinic, thus allowing treatment of most arterial endovascular cases conveniently and possibly with lesser overall community cost.[citation needed] Similar non-hospital treatment facilities for non-operative vein treatment have existed for some years and are now widespread in many countries.
NHS England conducted a review of all 70 vascular surgery sites across England in 2018 as part of its Getting It Right First Time programme. The review specified that vascular hubs should perform at least 60 abdominal aortic aneurysm procedures and 40 carotid endarterectomies a year. 12 trusts missed both targets and many more missed one of them. A programme of concentrating vascular surgery in fewer centres is proceeding.[6]
Vascular surgery encompasses surgery of the
Management of arterial diseases

The management of arterial pathology excluding coronary and intracranial disease is within the scope of vascular surgeons. Disease states generally arise from narrowing of the arterial system known as
Aneurysms
Aortic aneurysms

- Abdominal
An abdominal aortic aneurysm (AAA) refers to aneurysmal dilation of the aorta confined to the abdominal cavity. Most commonly, aneurysms are asymptomatic and located in the infrarenal position. Often, they are discovered incidentally or on screening exams in patients with risk factors such as a history of smoking. Patients with aneurysms which have a diameter less than 5 cm are at <1% rupture risk per year. When the aneurysm meets size criteria it can be treated with aortic replacement or EVAR.
- Thoracic
Thoracic aortic aneurysms are contained in the chest. Aneurysms of the descending aorta can often be treated with thoracic endovascular aortic repair or TEVAR. Treating aneurysms which involve the ascending aorta are generally within the scope of cardiac surgeons, but upcoming endovascular technology may allow for a more minimally invasive approach in some patients.
- Thoracoabdominal
Thoroacoabdominal aneurysms are those which span the chest and abdominal cavities. The Crawford classification was developed and describes five types of thoracoabdominal aneurysms.[9]
-
Abdominal aortic aneurysms can be classified as infrarenal, juxtarenal, pararenal or suprarenal as depicted in the illustration.
-
The Crawford Classification (Extent I-IV) and the Safi modification (Extent V) for thoracoabdominal aortic aneurysms is pictured above.
Other arterial aneurysms
In addition to treating aneurysms which arise from the aorta, vascular surgeons also treat aneurysms elsewhere in the body.
- Visceral arteries
Visceral artery aneurysms include those isolated to the
Indications for repair differ slightly between arteries. For instance, current guidelines recommend repair of renal and splenic artery aneurysms greater than 3 cm, and those of any size in women of childbearing age; whereas celiac and hepatic artery aneurysms are indicated for repair when their size is greater than 2 cm. This is in contrast to superior mesenteric artery aneurysms which should be repaired regardless of size when they are discovered.[11]
- Popliteal artery
A
Arterial dissections
The artery wall is composed of three concentric layers: the
Whereas cardiac surgeons are usually in charge of managing type A dissections, type B dissections are typically managed by vascular surgeons. The most common risk factor for type B aortic dissection is hypertension. The first line treatment for type B aortic dissection is aimed at reducing both heart rate and blood pressure and is referred to as anti-impulse therapy.

Should initial medical management fail or there is the involvement of a major branch of the aorta, vascular surgery may be needed for these type B dissections. Treatment may include thoracic endovascular aortic repair (TEVAR) with or without extra-anatomic bypass such as carotid-carotid bypass, carotid-subclavian bypass, or subclavian-carotid transposition.[14]
Visceral artery dissection
Visceral artery dissections are arterial dissections involving the
Mesenteric ischemia
Mesenteric ischemia results from the acute or chronic obstruction of the superior mesenteric artery (SMA). The SMA arises from the abdominal aorta and usually supplies blood from the distal duodenum through two-thirds of the transverse colon and the pancreas.
Chronic mesenteric ischemia
The symptoms of chronic mesenteric ischemia can be classified as
Acute mesenteric ischemia
Acute mesenteric ischemia (AMI) results from the sudden occlusion of the superior mesenteric artery.
Renovascular hypertension
The renal arteries supply oxygenated blood to the kidneys. The kidneys serve to filter the flood and control blood pressure through the renin-angiotensin system. One cause of resistant hypertension is atherosclerotic disease in the renal arteries and is generally referred to as renovascular hypertension. If renovascular hypertension is diagnosed and maximal medical fails to control high blood pressure, the vascular surgeon may offer surgical treatment, either endovascular or open surgical reconstruction.
Cerebrovascular disease

Vascular surgeons are responsible for treating extracranial cerebrovascular disease as well as the interpretation of non-invasive vascular imaging relating to extracranial and intracranial circulation such as
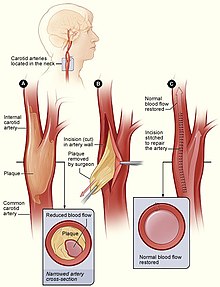
Symptoms of carotid artery stenosis can include transient ischemic attack or stroke. Both symptomatic and asymptomatic carotid stenosis can be diagnosed with the aid of carotid duplex ultrasound which allows for the estimation of severity of narrowing as well as characterize the plaque. Treatment can include medical therapy, carotid endarterectomy or carotid stenting.
The Society for Vascular Surgery publishes clinical practice guidelines for the management of extracranial cerebrovascular disease.[19] Less common diseases involving cerebral circulation treated by vascular surgeons include vertebrobasilar insufficiency, subclavian steal syndrome, carotid artery dissection, vertebral artery dissection, carotid body tumor and carotid artery aneurysm among others.
Peripheral arterial disease
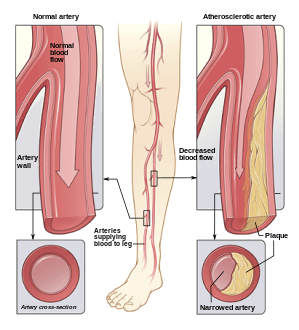
Peripheral artery disease PAD is the abnormal narrowing of the arteries which supply the limbs. Patients with this condition can present with intermittent claudication which is pain mainly in the calves and thighs while walking. If there is progression, a patient may also present with chronic limb threatening ischemia which encompasses pain at rest and non-healing wounds. Vascular surgeons are experts in the diagnosis, medical management, endovascular and open surgical treatment of PAD.[20]
A vascular surgeon may diagnose PAD using a combination of
-
Illustration of atherosclerosis causing arterial obstruction which clinically presents at peripheral artery disease.
-
ABI testing is used by vascular surgeons in the diagnosis of PAD. The blood pressure in the arm and leg are compared as a ratio.
-
Angioplasty (pictured) and stenting are two endovascular treatments employed by the vascular surgeon.
Management of venous diseases
Chronic venous disease
The vascular surgeon has several modalities to treat lower extremity venous disease which including medical, interventional and surgical procedures. For instance, venous ulceration may be treated with Unna's boots, superficial venous reflux with radiofrequency, laser ablation or vein stripping if indicated. When indicated, insufficiency in the deep veins may be treated with reconstruction of the venous valves with internal or external valvuloplasty.[23]
Varicose veins

Lower extremity
Nonthrombotic iliac vein lesions
Nonthrombotic iliac vein lesions (NIVL) include
Deep vein thrombosis
Post-thrombotic syndrome
Post-thrombotic syndrome (PTS) is a medical condition that sometimes occurs as a long-term complication of DVT and is characterized by long term edema and skin changes following DVT. Presenting symptoms may include itchiness, pain, cramps and paresthesia. It is estimated that between 20% and 50% of patients will experience some degree of PTS.[31] A treatment strategy for PTS may involve the use of compression stockings.
Pulmonary embolism
Surgical management of an acute pulmonary embolism (pulmonary thrombectomy) is uncommon and has largely been abandoned because of poor long-term outcomes. However, recently, it has gone through a resurgence with the revision of the surgical technique and is thought to benefit certain people.[32] Chronic pulmonary embolism leading to pulmonary hypertension (known as chronic thromboembolic hypertension) is treated with a surgical procedure known as a pulmonary thromboendarterectomy.[33]
Compressive venopathies
Compression of large veins by adjacent structures or masses may lead to distinct clinical syndromes including May–Thurner syndrome (MTS), nutcracker syndrome and superior vena cava syndrome to name a few. Treatment modalities include venography, intravascular ultrasound and venous stenting as well as more invasive open venous reconstruction and bypass.
Management of hemodialysis access
Patients with chronic kidney disease may have progression of disease which requires renal replacement therapy to filter their blood. One strategy for this therapy is hemodialysis, which is a procedure that involves filtering a patient's blood to remove waste products and returning their blood back to them. One method which avoids repeated arterial trauma is to create an arteriovenous fistula (AVF). The first procedure described for this purpose is named the Cimino fistula, after one of the surgeons who first had success with it. Vascular surgeons may create an AVF for a patient as well as undertake minimally invasive procedures to ensure the fistula remains patent.
Management of vascular trauma
One way that vascular trauma may be understood is by categorizing vascular injury by three criteria: mechanism of injury, anatomical site of injury and contextual circumstances. Mechanism of injury refers to etiology, e.g. iatrogenic, blunt, penetrating, blast injury, etc. Anatomical site functionally refers to whether there is compressible versus non-compressible hemorrhage, while contextual circumstances refers to injuries sustained in the civilian or military realm. Each context can be further broken down: military into combatant vs. noncombatant and civil into urban vs rural trauma.[34] This categorization scheme is of both epidemiologic and clinical significance. For instance, arterial injury in military combatants currently occurs predominantly in males in their twenties who are exposed to improvised explosive devices or gunshot wounds; whereas in the civilian realm, one study conducted in the United States showed the most common mechanisms to include motor vehicle collisions, firearm injuries, stab wounds and falls from heights.[35]
Blunt thoracic aortic injury
Advances in vascular surgery, specifically endovascular technologies, have led to a dramatic change in the operative approach to
Investigations
Major trials
| Name | Number of patients |
Description |
|---|---|---|
| Netherlands Vascular Study[37] | ||
| Multicentre Aneurysm Screening Study (MASS) | Found reduced mortality after screening for abdominal aortic aneurysms in the UK.[38]
| |
| UK Small Aneurysm Trial | 1090 | AAA 4–5.5 cm; Immediate surgery vs. ultrasound surveillance (and treatment for rapid expansion or AAA >5.5); 30-day mortality after elective AAA repair is 5.8%. No difference in survival.[39] |
| ADAM VA Cooperative Group Trial | 73451 | Patients in VA screened with no known history of aneurysm; Age 50–79; AAA 4.0-5.4 cm; similar conclusion to UK Small Aneurysm Trial.[40] |
| Joint Vascular Research Group Trial | 284 | Studied the relationship between intraoperative intravenous heparinization, blood loss during surgery and thrombotic complications. Conclusion: Intraoperative heparin, given before aortic cross-clamping, is an important prophylactic against perioperative MI[clarification needed] in aortic aneurysm surgery.[41]
|
| North American Symptomatic Carotid Endarterectomy Trial (NASCET) | 1415 | Showed carotid endarterectomy was beneficial in symptomatic patients. Two year stroke rate in patients with > 70% carotid stenosis decreased from 26% to 9%. Two year stroke rate in patients with > 50% decreased from 15% to 9%.[42][43] |
| Asymptomatic Carotid Atherosclerosis Study (ACAS) | 1662 | Demonstrated benefit in asymptomatic patients with >60% stenosis. Five year stroke rate reduced from 11% to 5.1% with carotid endarterectomy.[44][45] |
Training
Previously considered a field within general surgery, it is now considered a specialty in its own right. As a result, there are two pathways for training in the United States. Traditionally, a five-year general surgery residency is followed by a 1-2 year (typically 2 years) vascular surgery fellowship. An alternative path is to perform a five or six year vascular surgery residency. In many countries, Vascular surgeons can opt for additional training in cardiac surgery as well as post-residency.
Programs of training vary slightly between different regions of the world.
| Country | Standards bodies | Professional representation | Minimum length of training (post intern) |
|---|---|---|---|
| Australia and New Zealand | Royal Australasian College of Surgeons | Australian & New Zealand Society of Vascular Surgery (ANZSVS) | 6 years |
| Canada | Royal College of Surgeons of Canada
|
Canadian Society for Vascular Surgery | 5 years |
| Iran | Iran National Board of Vascular Surgery | Iranian College of Vascular Surgeons | 7 years (4 years of general surgery + 3 years of vascular surgery) |
| Italy | 5 years | ||
| United Kingdom | Royal College of Surgeons of England Royal College of Surgeons of Edinburgh |
Vascular Society of Great Britain and Ireland | 8 years (2 years of core surgery + 6 years of vascular surgery) |
| United States | American Board of Surgery American Osteopathic Board of Surgery |
Society for Vascular Surgery American College of Surgeons |
5 years (4 via 5-year integrated Vascular Surgery Residency). 7 if completing as a 2-year fellowship following general surgery[46] |
See also
- Society for Vascular Surgery, the major American professional society
- Ischemia-reperfusion injury of the appendicular musculoskeletal system
- Kakish Ryskulova
- Vein
- Phlebologist
- Cardiovascular disease
- Cardiology
References
- S2CID 235126667.
- PMC 5505391.
- ^ Dr. Venkatesh Ramaiah: "Dr. Ted Diethrich lessons carried forward" - The Antegrade Flow Show, retrieved 2021-10-28
- ^ "Dr. Ted Diethrich, founder of Arizona Heart Institute, dies at 81". www.beckershospitalreview.com. Retrieved 2021-10-28.
- PMID 29290495. Retrieved 23 Sep 2020.
- ^ "Trusts reveal plans to centralise services after GIRFT review". Health Service Journal. 19 March 2018. Retrieved 13 May 2018.
- ISBN 978-0-323-77557-1.)
{{cite book}}: CS1 maint: location (link - PMID 19231248.
- ^ "Crawford classification". Retrieved 13 February 2023.
- PMID 28613599.
- S2CID 214617284.
- S2CID 235170081.
- S2CID 11516764. Retrieved 13 February 2023.
- S2CID 210984324.
- PMID 33724090.
- PMID 19782510.
- S2CID 72885362.
- PMID 13541677.)
{{cite journal}}: CS1 maint: numeric names: authors list (link - S2CID 235596620.)
{{cite journal}}: CS1 maint: numeric names: authors list (link - ^ "Specialty at a Glance | Society for Vascular Surgery".
- PMID 28613694.
- PMID 29939530.
- ISBN 978-0-323-77557-1.)
{{cite book}}: CS1 maint: location (link - ISBN 978-0-340-93880-5.
- PMID 34108800.
- ISBN 978-0-323-77557-1.)
{{cite book}}: CS1 maint: location (link - ISBN 978-0-323-77557-1.)
{{cite book}}: CS1 maint: location (link - PMID 26993190.
- S2CID 236933535.
- PMID 33464575.
- PMID 31531971.
- PMID 15339878.
- ISBN 978-1-4987-1991-9.
- ISBN 978-0-323-69766-8.)
{{cite book}}: CS1 maint: location (link - PMID 20638516.
- ISBN 978-0-323-77559-5.)
{{cite book}}: CS1 maint: location (link - PMID 11282794.
- S2CID 21497118.
- S2CID 24733279.
- PMID 8040955.
- PMID 8696904.
- PMID 9811916.
- ^ LLC, Peripheral Brain. "NASCET - Wiki Journal Club". www.wikijournalclub.org. Retrieved 2021-02-11.
- )
- ^ "ACAS - Wiki Journal Club". www.wikijournalclub.org. Retrieved 2021-02-11.
- ^ VascularWeb: New Vascular Surgery Training Paradigms