Vasodilation
This article needs more primary sources. (March 2021) |  |
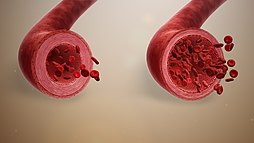
Vasodilation, also known as vasorelaxation, is the widening of blood vessels.[1] It results from relaxation of smooth muscle cells within the vessel walls, in particular in the large veins, large arteries, and smaller arterioles.[2] Blood vessel walls are composed of endothelial tissue and a basal membrane lining the lumen of the vessel, concentric smooth muscle layers on top of endothelial tissue, and an adventitia over the smooth muscle layers.[3] Relaxation of the smooth muscle layer allows the blood vessel to dilate, as it is held in a semi-constricted state by sympathetic nervous system activity.[2] Vasodilation is the opposite of vasoconstriction, which is the narrowing of blood vessels.
When blood vessels
By expanding available area for blood to circulate, vasodilation decreases
Endogenous substances and drugs that cause vasodilation are termed vasodilators. Many of these substances are neurotransmitters released by perivascular nerves of the autonomic nervous system[6] Baroreceptors sense blood pressure and allow adaptation via the mechanisms of vasoconstriction or vasodilation to maintain homeostasis.[2]
Function
The primary function of vasodilation is to increase blood flow in the body to tissues that need it most. This is often in response to a localized
Immune system
Vasodilation plays a major role in immune system function. Wider blood vessels allow more blood containing immune cells and proteins to reach the infection site. Vasodilation occurs as part of the process of inflammation, which is caused by several factors including presence of a pathogen, injury to tissues or blood vessels, and immune complexes.[7] In severe cases, inflammation can lead to sepsis or distributive shock.[11] Vasodilation is also a major component of anaphylaxis.[12]
Inflammation causes not only vasodilation but also causes increased
In the case of inflammation, vasodilation is caused by
Mechanism
A basic understanding of
Vascular resistance depends on several factors, including the length of the vessel, the viscosity of blood (determined by hematocrit) and the diameter of the blood vessel.[18] The latter is the most important variable in determining resistance, with the vascular resistance changing by the fourth power of the radius.[2] An increase in either of these physiological components (cardiac output or vascular resistance) causes a rise in MAP. Arterioles create the most vascular resistance of any blood vessel type, as they are very narrow and possess concentric layers of smooth muscle unlike venules and capillaries.[2]
Vasodilation occurs in superficial blood vessels of
Smooth muscle physiology
The
Vasodilation is the result of relaxation in
| Class | Description | Example |
|---|---|---|
| Hyperpolarization-mediated (Calcium channel blocker) | Changes in the voltage-sensitive calcium channels in the plasma membrane.
|
adenosine |
| cAMP-mediated | Adrenergic stimulation results in elevated levels of cAMP and protein kinase A, which results in increasing calcium removal from the cytoplasm. | prostacyclin |
| cGMP-mediated (Nitrovasodilator) | Through stimulation of protein kinase G .
|
nitric oxide |
PDE5 inhibitors and potassium channel openers can also have similar results.
Compounds that mediate the above mechanisms may be grouped as
Causes
Endogenous
| Vasodilators [24] | Receptor (↑ = opens. ↓ = closes) vascular smooth muscle cells if not otherwise specified
|
Transduction (↑ = increases. ↓ = decreases) [24] |
|---|---|---|
| EDHF | ? | VDCC → ↓intracellular Ca2+
|
PKG activity →
| ||
NO receptor on endothelium |
↓endothelin synthesis [25] | |
epinephrine (adrenaline) |
β-2 adrenergic receptor | ↑ MLCK → ↓MLCK activity → dephosphorylation of MLC
|
| histamine | histamine H2 receptor | |
| prostacyclin | IP receptor
| |
| prostaglandin D2 | DP receptor
| |
| prostaglandin E2 | EP receptor
| |
| VIP | VIP receptor | ↑ cAMP → ↑PKA activity →
|
| (extracellular) adenosine | adenosine receptors |
↑ VDCC → ↓intracellular Ca2+
|
| ↑P2Y receptor | activate → (see nitric oxide) | |
| L-arginine | imidazoline and α-2 receptor? | activity → ↓intracellular Ca2+ |
| bradykinin | bradykinin receptor | |
| substance P | ||
niacin (as nicotinic acid only) |
||
| platelet-activating factor (PAF) | ||
| CO2 | - | ↓ |
interstitial lactic acid (probably) |
- | |
| muscle work | - | |
|
various receptors on endothelium | ↓endothelin synthesis [25] |
The vasodilating action of activation of
Autonomic nervous system control
As referenced in the explanation of smooth muscle physiology, smooth muscle within the tunica media is innervated by the autonomic nervous system. The autonomic nervous system (ANS) controls essential involuntary body functions and originates as nerves leaving the brain stem or spinal cord; it contains both sensor and motor nerves.[2] The two divisions of the ANS, the sympathetic nervous system (SNS) and the parasympathetic nervous system (PSNS), impact blood vessels differently.[2] Traditionally we understand that these two divisions work against each other, the SNS producing "fight or flight" and the PSNS producing "rest and digest", but in the case of vascular innervation this line becomes blurred[6] ANS nerves do not directly innervate the vasculature via synapses with muscle cells; instead, they release neurotransmitters that reach target cells and effect smooth muscle contraction or relaxation.[6] Physical characteristics of the SNS and PSNS cause the SNS to have a prolonged, systemic impact on blood vessels, while the PSNS causes short-lived, localized change.[2] SNS stimulation causes a base level of vasoconstriction often referred to as basal neural tone, maintaining blood pressure.[2] Often vasodilation is simply the result of insufficient neurotransmitter to maintain basal neural tone, without the presence of a compound directly causing vasodilation.[2]
Neurotransmitters can act by binding directly to smooth muscle cells or by binding to endothelial cells mediating the effects of the neurotransmitter.[6] Below is a table summarizing major neurotransmitters involved in regulation of the vasculature.
| Neurotransmitter | Sympathetic or Parasympathetic | Target Cells and Receptors | Impact on Vasculature |
|---|---|---|---|
| norepinephrine (NE) | sympathetic (mostly) | adrenergic receptors α1, α2, β1, β2
α1- smooth muscle α2- endothelial β1, β2- smooth muscle |
α1- increase concentration calcium ions, vasoconstricton[6]
α2- inhibit cAMP, release NO, vasodilation[6] β1, β2- possible vasodilation[6] |
| Acetylcholine (Ach) | parasympathetic | nicotonic Ach receptors (nAchRs)
muscanaric Ach receptors (mAchRs) - on both endothelial and smooth muscle cells[6] |
nAchRs- modulate cytokines, counteract inflammation[6]
mAchRs- endothelial M3 AchR release NO, vasodlation smooth muscle M2 and M3 AchRs reduce release NO, vasoconstriction Note: Ach is quickly broken down, diffused, or undergoes reuptake, impacts are brief and localized[2] |
| Adenosine triphosphate (ATP) | sympathetic | purinergic receptors on smooth muscle and endothelial cells[6] | smooth muscle- increase calcium ion concentration, vasoconstriction[6]
endothelium- possible role as mediator of hyperpolarization of smooth muscle cells[6] co-released with norepinephrine[2] |
| Neuropeptide Y (NPY) | sympathetic | receptors on endothelial cells | causes vasoconstriction when co-released with norepinephrine[6] |
CGRP
|
? | CGRP1, CGRP2 receptors in endothelium[6] | vasodilation, role in vascular dysfunction if levels are abnormal[6] |
Also worthy of mention when discussing neural control of vasodilation is the renin-angiotensin-aldosterone system, or RAAS.[2] The kidneys retain water by reabsorbing sodium ions, or eliminate water by eliminating sodium ions.[29] Sympathetic nervous system activity, reduced blood volume or reduced arterial pressure trigger β-adrenergic receptors in select kidney cells[2] to release renin, which converts facilitates formation of angiotensin II from its substrate angiotensin.[29] Angiotensin II triggers adrenal glands to secrete aldosterone, a potent vasoconstrictor.[29]
Cold-induced
Cold-induced vasodilation (CIVD) occurs after cold exposure, possibly to reduce the risk of injury. It can take place in several locations in the human body but is observed most often in the extremities. The fingers are especially common because they are exposed most often.[citation needed]
When the fingers are exposed to cold,
A new phase of vasoconstriction follows the vasodilation, after which the process repeats itself. This is called the Hunting reaction. Experiments have shown that three other vascular responses to immersion of the finger in cold water are possible: a continuous state of vasoconstriction; slow, steady, and continuous rewarming; and a proportional control form in which the blood vessel diameter remains constant after an initial phase of vasoconstriction. However, the vast majority of responses can be classified as the Hunting reaction.[30]
Miscellaneous
This section needs more primary sources. (March 2022) |  |
- Other suggested vasodilators or vasodilating factors include:
- absence of high levels of environmental noise[31]
- arrhythmic[32]
- vasoconstricting effect of adrenaline)[33]
- atrial natriuretic peptide (ANP) - a weak vasodilator[34]
- ethanol (alcohol) causes immediate vasodilation followed by increase in blood pressure[35]
- nitric oxide inducers
- l-arginine (a key amino acid)[36]
- citrulline (causes increased levels of L-arginine in the body)[37]
- glyceryl trinitrate (commonly known as nitroglycerin)[38]
- isosorbide mononitrate and isosorbide dinitrate[39]
- pentaerythritol tetranitrate (PETN)[40]
- sodium nitroprusside[41]
- PDE5 inhibitors: these agents indirectly increase the effects of nitric oxide[42]
- sildenafil (Viagra)
- tadalafil (Cialis)
- vardenafil (Levitra)
- tetrahydrocannabinol (THC), the principal psychoactive constituent of cannabis[43]
- theobromine, the principal alkaloid found in Theobroma cacao, specifically in cocoa solids (which is found in chocolate, especially dark chocolate)[44]
- minoxidil[45]
- papaverine an alkaloid found in the opium poppy papaver somniferum[46]
- estrogen[47]
Treatment
Direct vasodilation drugs
These drugs can keep vessels staying opened or help vessels refrain from being narrowed.[48]
- Angiotensin II receptor blockers
- ACE inhibitors
- Calcium channel blockers
Alpha-2A adrenergic receptor agonists
Drugs that appear to work by activating the α2A receptors in the brain thereby decreasing sympathetic nervous system activity.[49][48]
- According to American Heart Association, Alpha-methyldopa may cause Orthostatic syncope as it exerts a greater blood pressure lowering effect when one is standing upright which may lead to feeling weak or fainting if the blood pressure has been lowered too far. Methyldopa's prominent side effects include drowsiness or sluggishness, dryness of the mouth, fever or anemia. Additionally to these, male patients may experience impotence.[48]
- clonidine hydrochloride
- guanabenz acetate
- guanfacine hydrochloride
- Clonidine, guanabenz or guanfacine may give rise to severe dryness of the mouth, constipation or drowsiness. Abrupt cessation taking may raise blood pressure quickly to dangerously high levels.[48]
Blood vessel muscle relaxants
Directly relax the muscle in the walls of the blood vessels (especially the arterioles), allowing the vessel to dilate (widen).[48]
- Hydralazine may cause headaches, swelling around the eyes, heart palpitations or aches and pains in the joints. In clinical setting, hydralazine is not usually used alone.[48]
- Minoxidil is a potent direct vasodilator used only in resistant severe high blood pressure or when kidney failure is present. Noted adverse effects comprise fluid retention (marked weight gain) and excessive hair growth.[48]
Therapeutic applications
Vasodilators are used to treat conditions such as
See also
References
- ^ "Definition of Vasodilation". MedicineNet.com. 27 April 2011. Archived from the original on 5 January 2012. Retrieved 13 January 2012.
- ^ PMID 21385998.
- ^ PMID 29262226. Retrieved 22 March 2024.
- ^ PMID 18771592.
- PMID 32491494. Retrieved 22 March 2024.
- ^ PMID 29593847.
- ^ PMID 19413999.
- PMID 9576114.
- S2CID 71178.
- ISBN 978-0-7216-0240-0.
- ^ PMID 24171518.
- ^ PMID 37628983.
- ^ PMID 25517612.
- ^ "What is volume flow rate? (article) | Fluids". Khan Academy. Retrieved 23 March 2024.
- PMID 34360549.
- PMID 30855814. Retrieved 23 March 2024.
- ^ Klablunde RE (29 April 2008). "Therapeutic Uses of Vasodilators". CVPharmacology. Archived from the original on 16 December 2008. Retrieved 3 December 2013.
- PMID 32310535. Retrieved 23 March 2024.
- PMID 20448028.
- PMID 20522732.
- ^ "Definition of Vasodilation". MedicineNet.com. 27 April 2011. Archived from the original on 5 January 2012. Retrieved 13 January 2012.
- ^ PMID 14627618.
- S2CID 14267377.
- ^ ISBN 978-1-4160-2328-9. Page 479
- ^ ISBN 978-0-443-06911-6.
- S2CID 8699034.
- PMID 11350258.
- S2CID 97773072.
- S2CID 22077172.
- PMID 31092312.
- PMID 32384746.
- PMID 32310526. Retrieved 24 March 2024.
- PMID 26074089.
- PMID 15837832.
- PMID 35070535.
- S2CID 3493542.
- PMID 29494004. Retrieved 24 March 2024.
- PMID 32491771. Retrieved 24 March 2024.
- PMID 20157049.
- PMID 32491419. Retrieved 24 March 2024.
- PMC 6914385.
- PMID 32575540.
- PMID 25750625.
- PMID 15133413.
- PMID 26586313.
- PMID 31173499.
- ^ a b c d e f g "Types of Blood Pressure Medications". www.heart.org. 31 October 2017. Archived from the original on 8 January 2019. Retrieved 2 May 2019.
- ^ "Guanfacine Monograph for Professionals". Drugs.com. American Society of Health-System Pharmacists. Retrieved 18 March 2019.
- ^ Klablunde RE (29 April 2008). "Therapeutic Uses of Vasodilators". CVPharmacology. Archived from the original on 16 December 2008. Retrieved 3 December 2013.
