Viral neuraminidase
| Neuraminidase | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| CAZy | GH34 | ||||||||||
| CDD | cd00260 | ||||||||||
| |||||||||||


Viral neuraminidase is a type of
Viral neuraminidases are the members of the glycoside hydrolase family 34 CAZY GH_34 which comprises enzymes with only one known activity;
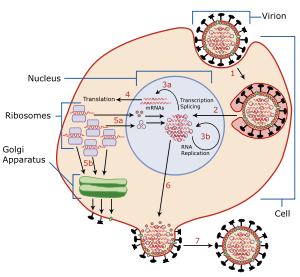
To infect a host cell, the influenza virus attaches to the exterior cell surface using hemagglutinin, a molecule found on the surface of the virus that binds to sialic acid groups. Sialic acids are found on various glycoproteins at the host cell surface. The virus then moves from sialic acid group to sialic acid group until it finds the proper cell surface receptor (whose identity remains unknown).[5] Neuraminadase enables this movement by cleaving sialic acid groups that hemagglutinin was attached to. After the virus has entered the cell and has replicated, new viral particles bud from the host cell membrane. The hemagglutinin on new viral particles remains attached to sialic acid groups of glycoproteins on the external cell surface and the surface of other viral particles; neuraminadase cleaves these groups and thereby allows the release of viral particles[6] and prevents self-aggregation.[5] Neuraminadase also facilitates the movement of virus particles in the presence of mucus rich in silicic acid.[5]
A single
Function
The enzyme helps viruses to be released after budding from the plasma membrane of a host cell. Influenza virus membranes contain two glycoproteins: hemagglutinin and neuraminidase. While the hemagglutinin on the surface of the virion is needed for infection, its presence inhibits release of the particle after budding. Viral neuraminidase cleaves terminal sialic acid residues from glycan structures on the surface of the infected cell. This promotes the release of progeny viruses and the spread of the virus from the host cell to uninfected surrounding cells. Neuraminidase also cleaves sialic acid residues from viral proteins, preventing aggregation of viruses.[medical citation needed]
Inhibitors
Neuraminidase has been targeted in structure-based enzyme inhibitor design programmes that have resulted in the production of two drugs, zanamivir (Relenza) and oseltamivir (Tamiflu). Administration of neuraminidase inhibitors is a treatment that limits the severity and spread of viral infections. Neuraminidase inhibitors are useful for combating influenza infection: zanamivir, administered by inhalation; oseltamivir, administered orally; and under research is peramivir administered parenterally, that is through intravenous or intramuscular injection.[citation needed]
Neuraminidase inhibition resistance
On February 27, 2005, a 14-year-old Vietnamese girl was documented to be carrying an
As strains of influenza are continuously mutating, it is essential that scientists quickly and efficiently determine the correct neuraminidase subtype that is responsible for the drug resistance in order to develop medications that will combat specific strains of influenza.[citation needed]
A new class of neuraminidase inhibitors that covalently attach to the enzyme have shown activity against drug-resistant virus in vitro.[7][8]
Specificity
In ideal circumstances, influenza virus neuraminidase (NA) should act on the same type of receptor the virus hemagglutinin (HA) binds to, a phenomenon that does not always happen. It is not quite clear how the virus manages to function when there is no close match between the specificities of NA and HA.[citation needed]
Exo- and endo-
Neuraminidase enzymes can have endo- or exo-
See also
- H5N1 genetic structure
- Antigenic shift
- Influenza research
- Hemagglutinin
References
- PMID 7880809.
- S2CID 41743465.
- ^ "WEHI History: 1957 Discovery of Neuraminidase - Key Flu Molecule". WEHI. Retrieved 2023-11-08.
- S2CID 41844816.
- ^ PMID 30079062.
- PMID 18321971.
- ^ BBC News: Flu drug 'shows promise' in overcoming resistance (accessed 22 February 2013)
- ^ "EC 3.2.1.129".
- ^ "EC 3.2.1.18".
External links
- Influenza Research Database Database of influenza sequences (including neuraminidase).
- Proteopedia Influenza Neuraminidase, Tamiflu and Relenza Avian Influenza Neuraminidase, Tamiflu and Relenza
