Vitamin B12
 General skeletal formula of cobalamins | |
 | |
| Clinical data | |
|---|---|
| Other names | Vitamin B12, vitamin B-12, cobalamin |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a605007 |
| License data |
|
intramuscular (IM), intranasal | |
| ATC code | |
| Legal status | |
| Legal status |
|
transcobalamins plasma proteins. Binding of hydroxocobalamin is slightly higher than cyanocobalamin. | |
| Metabolism | Liver |
| Elimination half-life | Approximately 6 days (400 days in the liver). |
| Excretion | Kidney |
| Identifiers | |
| |
JSmol) | |
| |
| |
Vitamin B12, also known as cobalamin, is a water-soluble
Vitamin B12 is the most chemically complex of all vitamins,[6] and for humans the only vitamin that must be sourced from animal-derived foods or supplements.[2][7] Only some archaea and bacteria can synthesize vitamin B12.[8] Vitamin B12 deficiency is a widespread condition that is particularly prevalent in populations with low consumption of animal foods. This can be due to a variety of reasons, such as low socioeconomic status, ethical considerations, or lifestyle choices such as veganism.[9]
Foods containing vitamin B12 include meat,
Vitamin B12 deficiencies have a greater effect on the pregnant, young children, and elderly people, and are more common in middle and lower developed countries due to malnutrition.
The diets of vegetarians and vegans may not provide sufficient B12 unless a dietary supplement is taken.
Vitamin B12 was discovered as a result of pernicious anemia, an
Definition
Vitamin B12 is a
- adenosylcobalamin
- cyanocobalamin, the adenosyl ligand in vitamin B12 is replaced by cyanide.
- hydroxocobalamin, the adenosyl ligand in vitamin B12 is replaced by hydroxide.
- methyl.
Cyanocobalamin is a manufactured form of B12. Bacterial fermentation creates AdoB12 and MeB12, which are converted to cyanocobalamin by the addition of potassium cyanide in the presence of sodium nitrite and heat. Once consumed, cyanocobalamin is converted to the biologically active AdoB12 and MeB12. The two bioactive forms of vitamin B
12 are
Cyanocobalamin is the most common form used in dietary supplements and food fortification because cyanide stabilizes the molecule against degradation. Methylcobalamin is also offered as a dietary supplement.[12] There is no advantage to the use of adenosylcobalamin or methylcobalamin forms for the treatment of vitamin B12 deficiency.[19][20][4]
Hydroxocobalamin can be injected intramuscularly to treat vitamin B12 deficiency. It can also be injected intravenously for the purpose of treating cyanide poisoning, as the hydroxyl group is displaced by cyanide, creating a non-toxic cyanocobalamin that is excreted in urine.
"Pseudovitamin B12" refers to compounds that are corrinoids with a structure similar to the vitamin but without vitamin activity.[21] Pseudovitamin B12 is the majority corrinoid in spirulina, an algal health food sometimes erroneously claimed as having this vitamin activity.[22]
Deficiency
Vitamin B12 deficiency can potentially cause severe and irreversible damage, especially to the brain and nervous system.
The main type of
- purines and thymidine).
- Gastrointestinal symptoms: alteration in bowel motility, such as mild autoimmune attack on the parietal cells of the stomach in pernicious anemia. There is an association with gastric antral vascular ectasia (which can be referred to as watermelon stomach), and pernicious anemia.[31]
- Neurological symptoms: sensory or motor deficiencies (absent reflexes, diminished vibration or soft touch sensation) and
Vitamin B12 deficiency is most commonly caused by malabsorption, but can also result from low intake, immune gastritis, low presence of binding proteins, or use of certain medications.
Nitrous oxide overdose or overuse converts the active monovalent form of vitamin B12 to the inactive bivalent form.[37]
Pregnancy, lactation and early childhood
The U.S. Recommended Dietary Allowance (RDA) for pregnancy is 2.6 μg/d, for lactation 2.8 μg/d. Determination of these values was based on an RDA of 2.4 μg/d for non-pregnant women, plus what will be transferred to the fetus during pregnancy and what will be delivered in breast milk.[12][38]: 972 However, looking at the same scientific evidence, the European Food Safety Authority (EFSA) sets adequate intake (AI) at 4.5 μg/d for pregnancy and 5.0 μg/d for lactation.[39] Low maternal vitamin B12, defined as serum concentration less than 148 pmol/L, increases the risk of miscarriage, preterm birth and newborn low birth weight.[40][38] During pregnancy the placenta concentrates B12, so that newborn infants have a higher serum concentration than their mothers.[12] As it is recently absorbed vitamin content that more effectively reaches the placenta, the vitamin consumed by the mother-to-be is more important than that contained in her liver tissue.[12][41]
Women who consume little animal-sourced food, or who are vegetarian or vegan, are at higher risk of becoming vitamin depleted during pregnancy than those who consume more animal products. This depletion can lead to anemia, and also an increased risk that their breastfed infants become vitamin deficient.[41][38] Vitamin B12 is not one of the supplements recommended by the World Health Organization for healthy women who are pregnant,[10] however vitamin B12 is often suggested during pregnancy in a multivitamin along with folic acid[42][43] especially for pregnant mothers who follow a vegetarian or vegan diet.[44]
Low vitamin concentrations in human milk occur in families with low socioeconomic status or low consumption of animal products.[38]: 971, 973 Only a few countries, primarily in Africa, have mandatory food fortification programs for either wheat flour or maize flour; India has a voluntary fortification program.[45] What the nursing mother consumes is more important than her liver tissue content, as it is recently absorbed vitamin that more effectively reaches breast milk.[38]: 973 Breast milk B12 decreases over months of nursing in both well-nourished and vitamin-deficient mothers.[38]: 973–974 Exclusive or near-exclusive breastfeeding beyond six months is a strong indicator of low serum vitamin status in nursing infants. This is especially true when the vitamin status was poor during the pregnancy and if the early-introduced foods fed to the still breastfeeding infant are vegan.[38]: 974–975
Risk of deficiency persists if the post-weaning diet is low in animal products.[38]: 974–975 Signs of low vitamin levels in infants and young children can include anemia, poor physical growth and neurodevelopmental delays.[38]: 975 Children diagnosed with low serum B12 can be treated with intramuscular injections, then transitioned to an oral dietary supplement.[38]: 976
Gastric bypass surgery
Various methods of gastric bypass or gastric restriction surgery are used to treat morbid obesity. Roux-en-Y gastric bypass surgery (RYGB) but not sleeve gastric bypass surgery or gastric banding, increases the risk of vitamin B12 deficiency and requires preventive post-operative treatment with either injected or high-dose oral supplementation.[46][47][48] For post-operative oral supplementation, 1000 μg/d may be needed to prevent vitamin deficiency.[48]
Diagnosis
According to one review: "At present, no 'gold standard' test exists for the diagnosis of vitamin B12 deficiency and as a consequence the diagnosis requires consideration of both the clinical state of the patient and the results of investigations."
Serum haptocorrin binds 80-90% of circulating B12, rendering it unavailable for cellular delivery by transcobalamin II. This is conjectured to be a circulating storage function.[54] Several serious, even life-threatening diseases cause elevated serum HC, measured as abnormally high serum vitamin B12, while at the same time potentially manifesting as a symptomatic vitamin deficiency because of insufficient vitamin bound to transcobalamin II which transfers the vitamin to cells.[55]
Medical uses

Treatment of deficiency
Severe vitamin B12 deficiency is initially corrected with daily intramuscular injections of 1000 μg of the vitamin, followed by maintenance via monthly injections of the same amount or daily oral dosing of 1000 μg. The daily dose is far in excess of the vitamin requirement because the normal transporter protein mediated absorption is absent, leaving only very inefficient intestinal passive absorption.[56][57] Injection side effects include skin rash, itching, chills, fever, hot flushes, nausea and dizziness. Oral maintenance treatment avoids this problem and significantly reduces cost of treatment.[56][57]
Cyanide poisoning
For
Dietary recommendations
Some research shows that most people in the United States and the United Kingdom consume sufficient vitamin B12.
The US
The European Food Safety Authority (EFSA) refers to the collective set of information as "dietary reference values", with population reference intake (PRI) instead of RDA, and average requirement instead of EAR. AI and UL are defined by EFSA the same as in the United States. For women and men over age 18 the adequate intake (AI) is set at 4.0 μg/day. AI for pregnancy is 4.5 μg/day, for lactation 5.0 μg/day. For children aged 1–14 years the AIs increase with age from 1.5 to 3.5 μg/day. These AIs are higher than the U.S. RDAs.[39] The EFSA also reviewed the safety question and reached the same conclusion as in the United States—that there was not sufficient evidence to set a UL for vitamin B12.[62]
The Japan National Institute of Health and Nutrition set the RDA for people ages 12 and older at 2.4 μg/day.[63] The World Health Organization also uses 2.4 μg/day as the adult recommended nutrient intake for this vitamin.[64]
For U.S. food and dietary supplement labeling purposes, the amount in a serving is expressed as a "percent of daily value" (%DV). For vitamin B12 labeling purposes, 100% of the daily value was 6.0 μg, but on May 27, 2016, it was revised downward to 2.4 μg.
Sources
Bacteria and archaea
Vitamin B12 is produced in nature by certain bacteria, and archaea.[69][70][71] It is synthesized by some bacteria in the gut microbiota in humans and other animals, but it has long been thought that humans cannot absorb this as it is made in the colon, downstream from the small intestine, where the absorption of most nutrients occurs.[72] Ruminants, such as cows and sheep, are foregut fermenters, meaning that plant food undergoes microbial fermentation in the rumen before entering the true stomach (abomasum), and thus they are absorbing vitamin B12 produced by bacteria.[72][73]
Other mammalian species (examples:
Non-ruminant, non-hindgut herbivores may have an enlarged forestomach and/or small intestine to provide a place for bacterial fermentation and B-vitamin production, including B12.
Animal-derived foods
Animals store vitamin B12 from their diets in their
Plants and algae
There is some evidence that bacterial fermentation of plant foods and symbiotic relationships between algae and bacteria can provide vitamin B12. However, the Academy of Nutrition and Dietetics considers plant and algae sources "unreliable", stating that vegans should turn to fortified foods and supplements instead.[34]
Natural plant and algae sources of vitamin B12 include fermented plant foods such as tempeh[80][81] and seaweed-derived foods such as nori and laverbread.[82][83][84] Methylcobalamin has been identified in Chlorella vulgaris.[85] Since only bacteria and some archea possess the genes and enzymes necessary to synthesize vitamin B12, plant and algae sources all obtain the vitamin secondarily from symbiosis with various species of bacteria,[5] or in the case of fermented plant foods, from bacterial fermentation.[80]
Fortified foods
Foods for which vitamin B12-fortified versions are available include
As of 2019, nineteen countries require food fortification of wheat flour, maize flour or rice with vitamin B12. Most of these are in southeast Africa or Central America.[45]
Vegan advocacy organizations, among others, recommend that every vegan consume B12 from either fortified foods or supplements.[6][36][87][88]
Supplements

Vitamin B12 is included in multivitamin pills; in some countries grain-based foods such as bread and pasta are fortified with B12. In the US, non-prescription products can be purchased providing up to 5,000 µg each, and it is a common ingredient in energy drinks and energy shots, usually at many times the recommended dietary allowance of B12. The vitamin can also be supplied on prescription and delivered via injection or other means.[2]
Sublingual methylcobalamin, which contains no cyanide, is available in 5 mg tablets. The metabolic fate and biological distribution of methylcobalamin are expected to be similar to that of other sources of vitamin B12 in the diet.[89] The amount of cyanide in cyanocobalamin is generally not a concern, even in the 1,000 µg dose, since the amount of cyanide there (20 µg in a 1,000 µg cyanocobalamin tablet) is less than the daily consumption of cyanide from food, and therefore cyanocobalamin is not considered a health risk.[89]
Intramuscular or intravenous injection
Injection of
A person with cobalamin C disease (which results in combined
Nanotechnologies used in vitamin B12 supplementation
Conventional administration does not ensure specific distribution and controlled release of vitamin B12. Moreover, therapeutic protocols involving injection require health care people and commuting of patients to the hospital thus increasing the cost of the treatment and impairing the lifestyle of patients. Targeted delivery of vitamin B12 is a major focus of modern prescriptions. For example, conveying the vitamin to the bone marrow and nerve cells would help myelin recovery. Currently, several nanocarriers strategies are being developed for improving vitamin B12 delivery with the aim to simplify administration, reduce costs, improve pharmacokinetics, and ameliorate the quality of patients' lives.[94]
Pseudovitamin-B12
Pseudovitamin-B12 refers to B12-like analogues that are biologically inactive in humans.[21] Most cyanobacteria, including Spirulina, and some algae, such as Porphyra tenera (used to make a dried seaweed food called nori in Japan), have been found to contain mostly pseudovitamin-B12 instead of biologically active B12.[22][95] These pseudo-vitamin compounds can be found in some types of shellfish,[21] in edible insects,[96] and at times as metabolic breakdown products of cyanocobalamin added to dietary supplements and fortified foods.[97]
Pseudovitamin-B12 can show up as biologically active vitamin B12 when a microbiological assay with Lactobacillus delbrueckii subsp. lactis is used, as the bacteria can utilize the pseudovitamin despite it being unavailable to humans. To get a reliable reading of B12 content, more advanced techniques are available. One such technique involves pre-separation by silica gel and then assessment with B12-dependent E. coli bacteria.[21]
A related concept is
Drug interactions
H2-receptor antagonists and proton-pump inhibitors
Gastric acid is needed to release vitamin B12 from protein for absorption. Reduced secretion of
Metformin
Reduced serum levels of vitamin B12 occur in up to 30% of people taking long-term
Other drugs
Certain medications can decrease the absorption of orally consumed vitamin B12, including colchicine, extended-release potassium products, and antibiotics such as gentamicin, neomycin and tobramycin.[103] Anti-seizure medications phenobarbital, pregabalin, primidone and topiramate are associated with lower than normal serum vitamin concentration. However, serum levels were higher in people prescribed valproate.[104] In addition, certain drugs may interfere with laboratory tests for the vitamin, such as amoxicillin, erythromycin, methotrexate and pyrimethamine.[103]
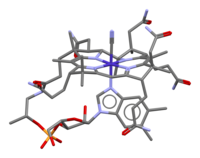
Chemistry

Vitamin B12 is the most chemically complex of all the vitamins.[6] The structure of B12 is based on a corrin ring, which is similar to the porphyrin ring found in heme. The central metal ion is cobalt. As isolated as an air-stable solid and available commercially, cobalt in vitamin B12 (cyanocobalamin and other vitamers) is present in its +3 oxidation state. Biochemically, the cobalt center can take part in both two-electron and one-electron reductive processes to access the "reduced" (B12r, +2 oxidation state) and "super-reduced" (B12s, +1 oxidation state) forms. The ability to shuttle between the +1, +2, and +3 oxidation states is responsible for the versatile chemistry of vitamin B12, allowing it to serve as a donor of deoxyadenosyl radical (radical alkyl source) and as a methyl cation equivalent (electrophilic alkyl source).[105]
Four of the six coordination sites are provided by the corrin ring, and a fifth by a

Methods for the analysis of vitamin B12 in food
Several methods have been used to determine the vitamin B12 content in foods including microbiological assays, chemiluminescence assays, polarographic, spectrophotometric and high-performance liquid chromatography processes.[107] The microbiological assay has been the most commonly used assay technique for foods, utilizing certain vitamin B12-requiring microorganisms, such as Lactobacillus delbrueckii subsp. lactis ATCC7830.[77] However, it is no longer the reference method due to the high measurement uncertainty of vitamin B12.[108]
Furthermore, this assay requires overnight incubation and may give false results if any inactive vitamin B12 analogues are present in the foods.[109] Currently, radioisotope dilution assay (RIDA) with labelled vitamin B12 and hog IF (pigs) have been used to determine vitamin B12 content in food.[77] Previous reports have suggested that the RIDA method is able to detect higher concentrations of vitamin B12 in foods compared to the microbiological assay method.[77][107]
Biochemistry
Coenzyme function
Vitamin B12 functions as a
Listed here are the three classes of enzymes that sometimes require B12 to function (in animals):- Isomerases
- Rearrangements in which a hydrogen atom is directly transferred between two adjacent atoms with concomitant exchange of the second substituent, X, which may be a carbon atom with substituents, an oxygen atom of an alcohol, or an amine. These use the adoB12 (adenosylcobalamin) form of the vitamin.[110]
- Methyltransferases
- Methyl (–CH3) group transfers between two molecules. These use the MeB12 (methylcobalamin) form of the vitamin.[111]
- Dehalogenases
In humans, two major coenzyme B12-dependent enzyme families corresponding to the first two reaction types, are known. These are typified by the following two enzymes:

Physiology
Absorption
Vitamin B12 is absorbed by a B12-specific transport proteins or via passive diffusion.
Investigations into the intestinal absorption of B12 confirm that the upper limit of absorption per single oral dose is about 1.5 µg, with 50% efficiency. In contrast, the passive diffusion process of B12 absorption — normally a very small portion of total absorption of the vitamin from food consumption — may exceed the haptocorrin- and IF-mediated absorption when oral doses of B12 are very large, with roughly 1% efficiency. Thus, dietary supplement B12 supplementation at 500 to 1000 µg per day allows pernicious anemia and certain other defects in B12 absorption to be treated with daily oral megadoses of B12 without any correction of the underlying absorption defects.[116]
After the IF/B12 complex binds to cubam the complex is disassociated and the free vitamin is transported into the
Malabsorption
Antacid drugs that neutralize stomach acid and drugs that block acid production (such as proton-pump inhibitors) will inhibit absorption of B12 by preventing release from food in the stomach.[119] Other causes of B12 malabsorption include intrinsic factor deficiency, pernicious anemia, bariatric surgery pancreatic insufficiency, obstructive jaundice, tropical sprue and celiac disease, and radiation enteritis of the distal ileum.[116] Age can be a factor. Elderly people are often achlorhydric due to reduced stomach parietal cell function, and thus have an increased risk of B12 deficiency.[120]
Storage and excretion
How fast B12 levels change depends on the balance between how much B12 is obtained from the diet, how much is secreted and how much is absorbed. The total amount of vitamin B12 stored in the body is about 2–5 mg in adults. Around 50% of this is stored in the liver. Approximately 0.1% of this is lost per day by secretions into the gut, as not all these secretions are reabsorbed. Bile is the main form of B12 excretion; most of the B12 secreted in the bile is recycled via enterohepatic circulation. Excess B12 beyond the blood's binding capacity is typically excreted in urine. Owing to the extremely efficient enterohepatic circulation of B12, the liver can store 3 to 5 years' worth of vitamin B12; therefore, nutritional deficiency of this vitamin is rare in adults in the absence of malabsorption disorders.[12] In the absence of enterohepatic reabsorption, only months to a year of vitamin B12 are stored.[121]
Cellular reprogramming
Vitamin B12 through its involvement in one-carbon metabolism plays a key role in cellular reprogramming and tissue regeneration and epigenetic regulation. Cellular reprogramming is the process by which somatic cells can be converted to a pluripotent state. Vitamin B12 levels affect the histone modification H3K36me3, which suppresses illegitimate transcription outside of gene promoters. Mice undergoing in vivo reprogramming were found to become depleted in B12 and show signs of methionine starvation while supplementing reprogramming mice and cells with B12 increased reprogramming efficiency, indicating a cell-intrinsic effect.[122][123]
Synthesis
Biosynthesis
Vitamin B12 is derived from a
Species from the following
Industrial
Industrial production of B12 is achieved through
The total world production of vitamin B12 in 2008 was 35,000 kg (77,175 lb).[134]
Laboratory
The complete laboratory synthesis of B12 was achieved by Robert Burns Woodward[135] and Albert Eschenmoser in 1972.[136][137] The work required the effort of 91 postdoctoral fellows (mostly at Harvard) and 12 PhD students (at ETH Zurich) from 19 nations. The synthesis constitutes a formal total synthesis, since the research groups only prepared the known intermediate cobyric acid, whose chemical conversion to vitamin B12 was previously reported. This synthesis of vitamin B12 is of no practical consequence due to its length, taking 72 chemical steps and giving an overall chemical yield well under 0.01%.[138] Although there have been sporadic synthetic efforts since 1972,[137] the Eschenmoser–Woodward synthesis remains the only completed (formal) total synthesis.
History
Descriptions of deficiency effects
Between 1849 and 1887,
Identification of liver as an anti-anemia food
During the 1920s,
Identification of the active compound
While working at the Bureau of Dairy Industry, U.S. Department of Agriculture,
George Whipple, George Minot and William Murphy were awarded the Nobel Prize in 1934 for their work on the vitamin. Three other Nobel laureates, Alexander R. Todd (1957), Dorothy Hodgkin (1964) and Robert Burns Woodward (1965) made important contributions to its study.[147]
Commercial production
Industrial production of vitamin B12 is achieved through
Society and culture
In the 1970s, John A. Myers, a physician residing in Baltimore, developed a program of injecting vitamins and minerals intravenously for various medical conditions. The formula included 1000 μg of cyanocobalamin. This came to be known as the Myers' cocktail. After his death in 1984, other physicians and naturopaths took up prescribing "intravenous micro-nutrient therapy" with unsubstantiated health claims for treating fatigue, low energy, stress, anxiety, migraine, depression, immunocompromised, promoting weight loss and more.[148] However, other than a report on case studies[148] there are no benefits confirmed in the scientific literature.[149] Healthcare practitioners at clinics and spas prescribe versions of these intravenous combination products, but also intramuscular injections of just vitamin B12. A Mayo Clinic review concluded that there is no solid evidence that vitamin B12 injections provide an energy boost or aid weight loss.[150]
There is evidence that for elderly people, physicians often repeatedly prescribe and administer cyanocobalamin injections inappropriately, evidenced by the majority of subjects in one large study either having had normal serum concentrations or had not been tested prior to the injections.[151]
See also
Further reading
- Gherasim C, Lofgren M, Banerjee R (May 2013). "Navigating the B(12) road: assimilation, delivery, and disorders of cobalamin". J. Biol. Chem. 288 (19): 13186–13193. PMID 23539619.
References
- PMID 27726382.
- ^ US National Institutes of Health. Archivedfrom the original on 2021-10-08. Retrieved 24 December 2021.
- PMID 24470095.
- ^ PMID 31490017.
- ^ PMID 17434786.
- ^ a b c d e f g h i j k "Vitamin B12". Micronutrient Information Center, Linus Pauling Institute, Oregon State University, Corvallis, OR. 4 June 2015. Archived from the original on 29 October 2019. Retrieved 5 April 2019.
- PMID 34199569.
- PMID 29216732.
- PMID 31316992.
- ^ PMID 38189492.
- ^ ISBN 978-0-323-66162-1.
US survey data from the NHANES What We Eat in America 2013e16 cohort reported the median vitamin B12 consumption for all adult men of 5.1 mcg and women of 3.5 mcg.95b Using the Estimated Average Requirement (EAR) for adults for Vitamin B12 of 2 mcg,93 less than 3% of men and 8% of women in the United States had inadequate diets using this comparator. However, 11% of girls 14e18 years had intakes less than their EAR of 2.0 mcg.
- ^ ISBN 978-0-309-06554-2. Retrieved February 7, 2012.
- ^ "Acid-Reflux Drugs Tied to Lower Levels of Vitamin B-12". WebMD. Archived from the original on 2018-07-23. Retrieved 2018-07-23.
- ^ a b c "Vitamin B12 Deficiency Anemia". www.hopkinsmedicine.org. 8 August 2021. Retrieved 2022-02-16.
- ^ "Pernicious anemia: MedlinePlus Medical Encyclopedia". medlineplus.gov. Retrieved 2022-01-06.
- PMID 10448529.
- ISBN 3-540-33047-X.
- ^ S2CID 37393683.
- PMID 25820384.
- PMID 28223907.
- ^ S2CID 4978703.
- ^ PMID 10552882.
- S2CID 29053617.
- ^ Skerrett PJ (February 2019). "Vitamin B12 deficiency can be sneaky, harmful". Harvard Health Blog. Archived from the original on 29 October 2019. Retrieved 6 January 2020.
- ^ "Vitamin B12 or folate deficiency anaemia – Symptoms". National Health Service, England. 23 May 2019. Archived from the original on 12 August 2017. Retrieved 6 January 2020.
- PMID 11574992.
- ^ S2CID 20350330.
- PMID 11304860.
- ^ "What Is Pernicious Anemia?". NHLBI. April 1, 2011. Archived from the original on 14 March 2016. Retrieved 14 March 2016.
- PMID 24248213.
- ^ Amarapurka DN, Patel ND (September 2004). "Gastric Antral Vascular Ectasia (GAVE) Syndrome" (PDF). Journal of the Association of Physicians of India. 52: 757. Archived (PDF) from the original on 2016-03-04.
- ISBN 978-1-60406-326-4.
- ISBN 978-1-4557-7566-8.
- ^ S2CID 4984228.
Fermented foods (such as tempeh), nori, spirulina, chlorella algae, and unfortified nutritional yeast cannot be relied upon as adequate or practical sources of B-12.39,40 Vegans must regularly consume reliable sources—meaning B-12 fortified foods or B-12 containing supplements—or they could become deficient, as shown in case studies of vegan infants, children, and adults.
- PMID 23356638.
- ^ PMID 25195560.
- PMID 28405070.
- ^ PMID 29141978.
- ^ a b "Overview on Dietary Reference Values for the EU population as derived by the EFSA Panel on Dietetic Products, Nutrition and Allergies" (PDF). 2017. Archived (PDF) from the original on 2020-01-07. Retrieved 2017-08-28.
- PMID 28108470.
- ^ PMID 30845641.
- PMID 35691683.
- ^ "Nutrition During Pregnancy". www.acog.org. Retrieved 2024-01-15.
- ^ "Pregnancy: Vegetarian Diet". myhealth.alberta.ca. Retrieved 2024-01-15.
- ^ a b "Map: Count of Nutrients In Fortification Standards". Global Fortification Data Exchange. Archived from the original on 11 April 2019. Retrieved 15 April 2020.
- PMID 26185175.
- PMID 24091055.
- ^ S2CID 35209784.
- PMID 25824066.
- S2CID 5772424.
- PMID 30626145.
- ^ "Methylmalonic acidemia". Genetics Home Reference. US National Library of Medecine. October 2015. Retrieved 10 July 2022.
- PMID 16916826.
- PMID 36680553.
- PMID 14636871.
- ^ PMID 36249776.
- ^ PMID 30261596.
- PMID 3295013.
- PMID 24994676.
- PMID 16990188.
- ^ a b c "Foods highest in Vitamin B12 (based on levels per 100-gram serving)". Nutrition Data. Condé Nast, USDA National Nutrient Database, release SR-21. 2014. Archived from the original on November 16, 2019. Retrieved February 16, 2017.
- ^ "Tolerable Upper Intake Levels For Vitamins And Minerals" (PDF). European Food Safety Authority. 2006. Archived (PDF) from the original on 2019-10-15. Retrieved 2016-03-12.
- ^ "Dietary Reference Intakes for Japanese 2010: Water-Soluble Vitamins" Journal of Nutritional Science and Vitaminology 2013(59):S67–S82.
- ISBN 978-92-4-154612-6.
- ^ "Food Labeling: Revision of the Nutrition and Supplement Facts Labels" (PDF). Federal Register. May 27, 2016. p. 33982. Archived (PDF) from the original on August 8, 2016. Retrieved August 27, 2017.
- ^ "Daily Value Reference of the Dietary Supplement Label Database (DSLD)". Dietary Supplement Label Database (DSLD). Archived from the original on 7 April 2020. Retrieved 16 May 2020.
- ^ "Changes to the Nutrition Facts Label". U.S. Food and Drug Administration (FDA). 27 May 2016. Retrieved 16 May 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ "Industry Resources on the Changes to the Nutrition Facts Label". U.S. Food and Drug Administration (FDA). 21 December 2018. Retrieved 16 May 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- PMID 28137297.
- S2CID 26057998.
- ISBN 978-0-387-78518-9.
- ^ PMID 26024497.
- ^ S2CID 103191.
- ISBN 978-0-470-37668-3. Archivedfrom the original on 2017-09-08. Retrieved 2017-01-17.
- ^ Erickson A (September 3, 2019). "Cobalt deficiency in sheep and cattle". Department of Primary Industries and Regional Development. Government of Western Australia. Archived from the original on 2015-11-11. Retrieved 2020-04-18.
- ^ a b Rooke J (October 30, 2013). "Do carnivores need Vitamin B12 supplements?". Baltimore Post Examiner. Archived from the original on January 16, 2017. Retrieved January 17, 2017.
- ^ S2CID 14732788.
- ^ Dossey AT (February 1, 2013). "Why Insects Should Be in Your Diet". The Scientist. Archived from the original on November 11, 2017. Retrieved April 18, 2020.
- ^ a b "Vitamin B-12 (µg)" (PDF). USDA National Nutrient Database for Standard Reference Release 28. 27 October 2015. Archived (PDF) from the original on 26 January 2017. Retrieved 6 January 2020.
- ^ PMID 8017933.
- PMID 23870976.
- PMID 24803097.
- PMID 20607069.
- PMID 21436999.
- PMID 25306351.
- S2CID 22232461.
- ^ Mangels R. "Vitamin B12 in the Vegan Diet". Vegetarian Resource Group. Archived from the original on December 19, 2012. Retrieved January 17, 2008.
- ^ "Don't Vegetarians Have Trouble Getting Enough Vitamin B12?". Physicians Committee for Responsible Medicine. Archived from the original on October 8, 2011. Retrieved January 17, 2008.
- ^ . "the metabolic fate and biological distribution of methylcobalamin and 5′-deoxyadenosylcobalamin are expected to be similar to that of other sources of vitamin B12 in the diet".
- S2CID 919401.
- PMID 16585128.
- S2CID 1929961.
- S2CID 23493993.
- PMID 33809596.
- PMID 10642899.
- S2CID 58651702.
- PMID 19326342.
- PMID 32956545.
- S2CID 25413839.
- PMID 27806244.
- PMID 11863489.
- ^ Copp S (1 December 2007). "What effect does metformin have on vitamin B12 levels?". UK Medicines Information, NHS. Archived from the original on September 27, 2007.
- ^ a b "Vitamin B-12: Interactions". WebMD. Retrieved 21 April 2020.
- S2CID 7282489.
- PMID 25945462.
- ISBN 978-3-527-30990-0.
- ^ a b Lawrance P (March 2015). "Vitamin B12: A review of analytical methods for use in food". LGC Limited.
- PMID 22254022.
- ISBN 978-1-315-11954-0.
- ^ PMID 22661206.
- ^ PMID 30693532.
- PMID 22961902.
- PMID 25327251.
- S2CID 34612963.
- PMID 10730193.
- ^ PMID 35337622.
- ISBN 978-0-13-981176-0.
- PMID 10714245.
- PMID 24327038.
- PMID 10448529.
- ^ "Vitamin B12 Deficiency – Nutritional Disorders". MSD Manual Professional Edition. Retrieved 2022-05-24.
- PMID 37973897.
- S2CID 265273574.
- S2CID 9070849.
- PMID 16042604.
- (PDF) from the original on 2018-07-24. Retrieved 2020-02-20.
- ISBN 0-521-82873-2.
- PMID 13854292.
- S2CID 22232461.
- ^ PMID 28137297.
- S2CID 27191837.
- PMID 29167919.
- ^ Riaz M, Ansari ZA, Iqbal F, Akram M (2007). "Microbial production of vitamin B12 by methanol utilizing strain of Pseudomonas species". Pakistan Journal of Biochemistry & Molecular Biology. 40: 5–10.[permanent dead link]
- ^ Zhang Y (January 26, 2009). "New round of price slashing in vitamin B12 sector (Fine and Specialty)". China Chemical Reporter. Archived from the original on May 13, 2013.
- S2CID 120110443.
- PMID 867037.
- ^ .
- ^ a b "Synthesis of Cyanocobalamin by Robert B. Woodward (1973)". www.synarchive.com. Archived from the original on 2018-02-16. Retrieved 2018-02-15.
- ^ ISBN 978-1-4511-7268-3. Chapter 36: Megaloblastic anemias: disorders of impaired DNA synthesis by Ralph Carmel
- ^ "George H. Whipple – Biographical". www.nobelprize.org. Archived from the original on 2017-09-13. Retrieved 2017-10-10.
- ^ "The Nobel Prize in Physiology or Medicine 1934". NobelPrize.org. Retrieved 2023-02-23.
- ^ "Mary Shorb Lecture in Nutrition". Archived from the original on March 4, 2016. Retrieved March 3, 2016.
- ^ Shorb MS (May 10, 2012). "Annual Lecture". Department of Animal & Avian Sciences, University of Maryland. Archived from the original on December 12, 2012. Retrieved August 2, 2014.
- S2CID 4220926.
- S2CID 4210164.
- ^ S2CID 61764553.
- ^ Carpenter KJ. "The Nobel Prize and the discovery of vitamins". nobelprize.org. Archived from the original on 2023-08-20. Retrieved 2023-11-19.
- ^ PMID 12410623.
- Science-Based Medicine. Archivedfrom the original on 11 January 2020. Retrieved 10 January 2020.
- ^ Bauer BA (29 March 2018). "Are vitamin B-12 injections helpful for weight loss?". Mayo Clinic. Archived from the original on 27 November 2019. Retrieved 11 January 2020.
- PMID 31305876.
External links
- Cyanocobalamin at the U.S. National Library of Medicine Medical Subject Headings (MeSH)






